Monitoring of system hemodynamics in prevention of cardiovascular pathology
Автор: Mikhail А. Yakushin, Roman V. Gorenkov, Аlexey P. Kudrin, Tatyana P. Vasilieva, Sergey Y. Yarotsky
Журнал: Cardiometry @cardiometry
Статья в выпуске: 19, 2021 года.
Бесплатный доступ
A comprehensive study of the system hemodynamics has been conducted by us in different age-related groups; regularities of the age-linked dynamics of the main indicators thereof and their mutual interrelations have been investigated. We have justified some additional prediction factors responsible for the development of arterial hyperstension and the relevant patterns of prevention measures associated therewith.
System hemodynamics, Personal profile of system hemodynamics, Monitoring of system hemodynamics, Arterial hypertension, Prevention of arterial hypertension, Volumetric compression oscillometry
Короткий адрес: https://sciup.org/148320549
IDR: 148320549 | DOI: 10.18137/cardiometry.2021.19.4347
Текст статьи Monitoring of system hemodynamics in prevention of cardiovascular pathology
Imprint
Mikhail А. Yakushin, Roman V. Gorenkov, Аlexey P. Kudrin, Tatyana P. Vasilieva, Sergey Y. Yarotsky. Monitoring of system hemodynamics in prevention of cardiovascular pathology. Car-diometry; Issue 19; August 2021; p. 43-47; DOI: 10.18137/car-diometry.2021.19.4347; Available from: http://www.cardiometry. net/issues/no19-august-2021/monitoring-of-system
Aims. The aim of our study has been formulated as follows: to identify the regularities of the age shifts of the system hemodynamics, when assessing stability of its functioning and predicting development of arterial hypertension.
The fundamental constant of the system hemodynamics (SHD) is the system arterial pressure (SAP), which is responsible for the proper circulation of blood in a human organism. The value of SAP corresponds to an averaged hemodynamic pressure and is calculated by the formula as follows:
SAP = CO x TPVS, where SAP is the system arterial pressure; CO is cardiac output, and TPVS is the total peripheral vascular resistance [1].
Since cardiac output is a derivative of stroke volume (SV) and heart rate (HR), the SAP level is determined by a ratio of three constants: HR, CO and TPVS [2].
In the different life activity periods, blood supplies to the organs and tissues in a human organism can regularly vary. In the period of high mental activity, observed is a greater supply of blood to the human brain, while the circulation in the muscle system and the viscera becomes rather poorly; under the physical activity conditions the coronary flow is increasing, and the muscle system blood vessels are expanding; in the sleeping period found is intensification of blood supplies to the viscera. However at the same time, irrespective of the intensity of the performance of the heart and the extent to what the blood vessels are actually filled, SAP must be maintained at a certain pre-specified level, which is required to provide an efficient perfusion of oxygen and energetic substrates. The SAP stability is provided by redistributing shifts of some of its derivatives: the TPVR shifts are compensated by the polar deviations of the CO parameters, and vasoconstriction in some vascular beds is balanced out by vasodilatation in the other vascular bed regions [3].
Every ergo- or trophotropic process is accompanied by a stereotypic response made by the cardiovascular system to optimize the blood supply for the proper circulation to an organ or a tissue responsible for the proper management of the process in question. In a healthy human body, such responses are provided reflexively, due to blood flow redistribution. Upon effects produced by pathogenetic factors, observed is imbalancing of the regulatory mechanisms that results initially in episodes of SHD abnormalities and later in permanent disorders thereof. In addition to stress, harmful effects made by environmental pollution, a nutritionally unsound diet and unhealthy lifestyle, the age-related factor plays an important part in disordering of the cardiovascular system performance.
Despite the fact that there are many researches devoted to investigations of regularities and patterns in the age-related degeneration of the circulatory system, we can state that unfortunately no consensus has been reached on this topic.. It may be partially attributed to shortcomings available in the existing diagnostics technologies. Up to the present time, the only Gold Standard in the SHD examination has remained the Swan-Ganz catheterization (also called pulmonary artery catheterization). The above catheterization technique is connected with a lot of technical difficulties, may involve a mortality risk and must be used for in-patients only. Recently, fresh techniques have appeared which are capable of measuring the basic constant parameters of SHD in a non-invasive way [4].
Materials and methods
Our materials have covered a cohort of 3393 patients aged from 18 to 89, including 1391 (40,4%) males and 2022 (59,6%) females, which have been examined by us in the framework of the governmental prevention medical routine check-up and/or follow-up according to the Russian National Statuary Health Insurance based on Order No. 124n “Approval of Procedure of Prevention Check-up and Follow-up of Specified Groups of Adults” dd. 13.03.2019 issued by the Healthcare Ministry of the Russian Federation (see Table 1 herein).
Table 1
Distribution of examined patients according to age groups and SYAP data
|
Age, years |
Systolic arterial pressure (SyAP) (mm Hg) |
Total |
|||
|
<110 |
110-139 |
140-159 |
>160 |
||
|
Under 20 |
22 |
57 |
3 |
1 |
83 |
|
20-24 |
35 |
107 |
87 |
1 |
230 |
|
25-29 |
8 |
27 |
48 |
0 |
83 |
|
30-34 |
15 |
89 |
152 |
12 |
268 |
|
35-39 |
7 |
19 |
156 |
18 |
200 |
|
40-44 |
10 |
23 |
202 |
25 |
260 |
|
45-49 |
25 |
62 |
549 |
33 |
669 |
|
50-54 |
23 |
254 |
580 |
45 |
902 |
|
55-59 |
31 |
131 |
77 |
15 |
254 |
|
60-64 |
1 |
75 |
44 |
10 |
130 |
|
65-69 |
7 |
53 |
56 |
14 |
130 |
|
70-74 |
0 |
19 |
24 |
13 |
56 |
|
75-79 |
2 |
26 |
31 |
18 |
77 |
|
80-84 |
0 |
15 |
1 |
17 |
33 |
|
Over 85 |
0 |
6 |
8 |
4 |
18 |
|
Total: |
186 |
963 |
2018 |
226 |
3393 |
The normal value of SI reaches 30-45 ml/m2 , and the normal level of SPVR is 32±6% arbitrary units. The normal value of HR has been accepted by us to be 60-80 beats per minute; the normal value of SYAP has been taken to be 110-130 mmHg, and that of DIAP has been accepted to be 70-80 mmHg.
Methods. The method of our examination is the compression oscillometry supported with device KAP TsG osm “GLOBUS” (Certificate of Registration No. RZN2017/6582 dd. 15.12.2017) that offers to non-in-vasively obtain 22 indicators of the actual status of SHD including the following: systolic AP (SYAP), diastolic AP (DIAP), HR, SV and TPVR. Since the SV and TPVR values depend on BMI indices and show no distinct normal limits, we have adopted in our calculations integrated indicators of SI (Stroke Index) computed as SV/T, where T is the surface area of the human body (m2) and SPVR (Specific Peripheral Vascular Resistance) derived as follows: TPVR/T. The normal values of the above indicators have been accepted as follows: HR has been considered to be 60-80 beats per min., SYAP has been taken to be 110-130 mmHg, and DIAP has been accepted to be 70-80 mmHg.
Results and discussion
In the majority of the patients (66,1%) we have detected an increase in SYAP, including SYAP degree I in 2018 test subjects (59,5%) and SYAP degree II and III in 226 patients (6,7%).
The normal SYAP values have been most commonly found in the age groups under 20 years (67,8%) and 20-24 years (46,5%) that is understandable taking into account young age of the examinees. However regardless of their young age, we have recorded in more than one third of the patients (37,8%) aged 20-24 a higher level of SYAP (140-159 mmHg) that has been considered as degree 1 hypertension. So, the share of the AH patients with degree I hypertension has been consistently increased with age in age group 25-49 years, reaching 82% in the age group of 44-49 years. Beginning with the age of 50, the said sharing changes with a greater proportion of the individuals with the normal SYAP values. As to the age group of 55-59 years, we have recorded the normal SYAP in one out of every three test subjects (28,2%), while in the age group of 55-59 years the normal SYAP values have been revealed in one out of two persons (51,6%), and in the age group of 60-64 we have detected the normal values thereof in more than half of the examined patients (57,7%) (see Figure 1 herein).
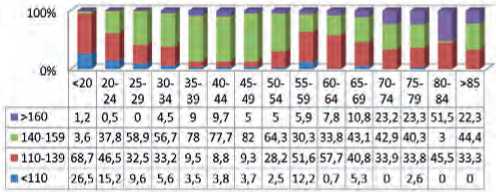
Figure 1. Age-related dynamics of SYAP profile
In our opinion, the revealed, at first glance unexpected, inconsistency in prevalence of the normal SYAP values among the older patients should be attributed to their more pronounced adherence to antihypertensive therapy. Whereas in the groups under 30 there is no antihypertensive-drug (AHD) medicated patient available, in the group aged 60-64 one out of each two participants (54,6%) has received the antihypertensive medication.
Beginning with the age of 65, observed is a further decrease in the share of the test subjects showing the normal SYAP values due to the age-determined growth of the arterial hypertension (AH) incidence. Another obvious explanation of this regularity is an age-associated aggravation of the AH progression: according to the data obtained by us, the share of those who suffer from AH grade II and III has demonstrated its growth from 5% in the age group of 55-59 years to 51,5% in the group of 80-84 years. It is particularly remarkable that in the age groups of the test subjects over 85, against the background of the AH incidence rate growth, the share of the patients with the severe disease course has been reduced to a half as against the respective data analyzed in the preceding age group (see Figure 1 herein).
The phenomenon of the paradox reduction in the AH incidence rate in the middle-age groups can be clearly traced in an analysis of the age-associated dynamics of the average data on arterial pressure (AP). The maximum depression found in the AP curves refers to the age group of 45-54 years (see Figure 2 herein).
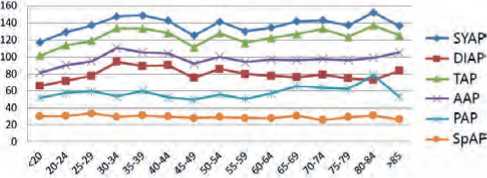
Figure 2. Age-associated dynamics of average values of arterial pressure (mmHg). Legend: SYAP is systolic arterial pressure, DIAP is diastolic arterial pressure, TAP is true arterial pressure; AAP is average arterial pressure; PAP is pulse arterial pressure and SpAP is specific arterial pressure.
The stable increase in the SYAP values is the key marker of AH and bears witness to the fact that there is a failure of the compensatory processes responsible for the maintenance of the stable SHD level. By comparing the groups with the normal SYAP values and those with the elevated SYAP levels, the prevalence of the test subjects showing higher SI values among the AH cohort persons is noticeable (see Figure 3 herein).
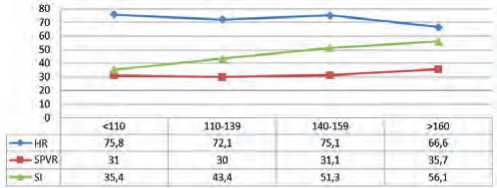
Figure 3. Correlation between SHD and SYAP values. Legend: HR – hear rate (beats per minute); SPVR – specific peripheral vascular resistance (arb.u.); SI – stroke index (ml/m2)
Our analysis of the age-related dynamics of the SI values shows that we deal with the age-associated growth of this indicator: the share of the patients with the elevated SI values has demonstrated a direct dependency on the age and progressively increased from 13% for the age group of 20-24 years up to 100% in the group of 80-84 years (see Figure 4 herein).
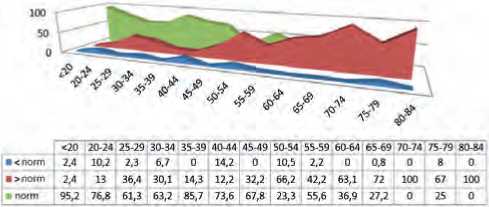
Figure 4. Age-related dynamics of SI data
The maximum share of the test subjects with the elevated level of SPVS has been found in the age group of 30-49 years. It is known that it is just the life period that is characterized by development and fixing of the major pathogenetic patterns under AH [5].
The above mentioned regularity revealed by us gives grounds to expect that an increase in SPVR, reflecting primarily the state of the vascular tonus, is one of the initiating members in the AH pathogenesis chain (see Figure 5 herein).
According to our data, we have revealed quite a lot of individuals with a predisposition of a HR increase
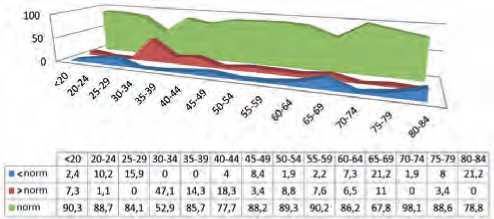
Figure 5. Age-related dynamics of SPVR data among the patients of the young and middle age; in the age groups 20-29 and 40-44 we have observed tachycardia in one out of every two individuals, and in the group of 35-39 years we have detected this phenomenon in 60,8% of the examinees (see Figure 6 herein).
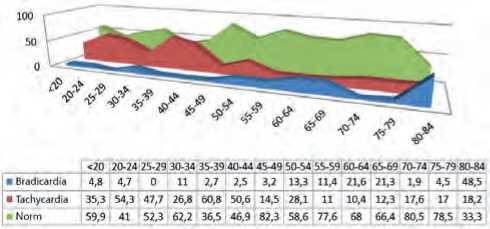
Figure 6. Age-related dynamics of HR data
This phenomenon can be explained by the fact that stable tachycardia, as it is the case with an increase in TPVR, is an initiator of imbalance in the reflector performance of the cardiovascular system, one of the precursors to the AH development.
It is noteworthy that beginning with the age of 50 we can trace a tendency towards an increase in the relative share of the patients with bradycardia as a more stable compensatory response made by SHD as compared with a reduction in SI.
Attention should be given to the fact that the dynamics of the average HR and SI data in all age groups demonstrates an inverse relationship, i.e. one of indicator becomes larger as the other becomes smaller. A similar regularity has been recorded with respect to the dynamics of the SPVR and SI data in the age groups under 49 and over 75 years.
In the age groups of 50-57 years we have revealed a phenomenon referred to as synchronization between SPVR and SI, the essence of which is the loss of the inverse relationship of the dynamics of the above mentioned indicators that may bear witness to the fact that there is a drop in effectiveness of the operation of the compensatory cardiovascular mechanisms 46 | Cardiometry | Issue 19. August 2021
responsible for the maintenance of the stable SHD: the change in the state of the vascular bed cannot be adequately compensated by modulation of the heart performance.
The phenomenon of synchronization has been discovered by us together with relationship SPVR – HR: in the age group of 20-34 years the above variables demonstrate their counteraction, while beginning with the age of 35 they are synchronized (see Figure 7 herein).
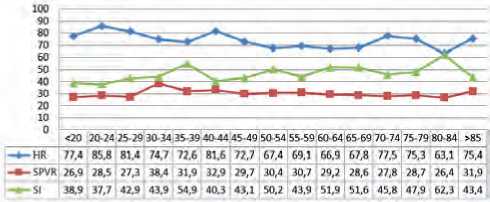
Figure 7. Age-related dynamics of average HR, SPVR and SI data
The main feature of the age-related dynamics of the average values of SPVR and SI in the group of test subjects with the SYAP level over 160, as compared with the total cohort of the examinees, is that the AH patients demonstrate the synchronization of the above curves considerably earlier: at their age of 20-24 years (see Figure 8 herein).
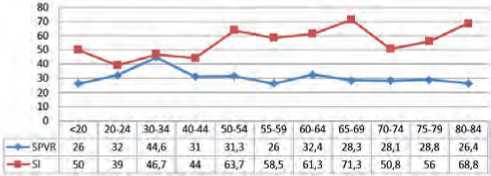
Figure 8. Age-related dynamics of average values of SPVR and
SI in test subjects with SYAP > 160
In this case, considering the individuals with the higher SYAP values, the share of the patients, who show at the same time the increased SPVR and SI values as well as the elevated SPVR and HR parameters, is 3 times greater than it is the case with the test subjects with the normal level of SYAP (see Table 2 herein).
This gives us the right to state that the synchronization of the dynamics of relations SPVR-SI and SPVR-HR has a negative prognostic value in assessment of the stability of the SHD function case with further prospects for the AH progression.
Table 2
Relationship between SHD profile and SYAP level
|
SHD profile* (HR/ SPVR/SI) |
SYAP 120-130 |
SYAP >140 |
SYAP >160 |
SYAP >170 |
|
112 |
4.8 |
17.6 |
3.6 |
0 |
|
113 |
0 |
5.2 |
0 |
0 |
|
121 |
0 |
0.7 |
4.5 |
2 |
|
122 |
9.6 |
15.3 |
0 |
0 |
|
123 |
1.2 |
1.1 |
0 |
0 |
|
211 |
3.6 |
11.8 |
12.5 |
10.4 |
|
212 |
25.3 |
4.5 |
32.1 |
37.6 |
|
213 |
0 |
0 |
0 |
0 |
|
221 |
19.3 |
18.1 |
14.3 |
8.3 |
|
222 |
22.9 |
7 |
0 |
0 |
|
223 |
0 |
0 |
0 |
0 |
|
231 |
0 |
0.2 |
0 |
0 |
|
311 |
7.3 |
7.1 |
18.7 |
22.9 |
|
321 |
6 |
11.2 |
14.3 |
18.8 |
|
322 |
0 |
0 |
0 |
0 |
* The SHD profile is represented by ratio HR/SPVR/SI, where 1 is an increased value of the indicator in question; 2 is the normal value thereof and 3 is a value below its norm.
Conclusion
The revealed regularities are capable of properly interpreting the hemodynamics-related mechanisms of the AH development, and they make possible to submit for thorough consideration by the scientific community of a set of supplements to improve the routine therapy and diagnostics approaches.
-
1. The high incidence rate of AH among young individuals dictates the necessity to provide SHD monitoring in all human individuals aged over 18 and include this type of examination into the scope of the standard prevention examination financed by the Federal Russian National Authority.
-
2. When assessing the actual state of SHD, we shall consider an increase in the levels of SPVR and SI as predictors of unfavorable prognosis; especially critical shall be their growth recorded for a number of years.
-
3. A combined increase at least of two major indicators of SHD, including HR, SPVR, SI and their dynamic synchronization, bears witness to the fact that there is a failure in operation of the compensato-
- ry mechanisms of SHD and dictates the necessity to medication correction with the AHD administration to provide the required pharmodynamic normalization by eliminating the revealed abnormalities.
-
4. The normalization of the abnormal HR, SPVR and SI values as well elimination of their reciprocal desynchronization, i.e. restoration of the physiologically normal polar dependence, shall be considered as positive criteria for effectiveness in the AH therapy.
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Monitoring of system hemodynamics in prevention of cardiovascular pathology
- Zaiko NN, Byts YuV, Ataman AV. Pathological physiology. Textbook for students of medical universities. K.: Logos, 1996. [in Russian]
- Timokhina OA, Baranov VA, Safronov MI. Noninvasive methods and means of measuring indicators of systemic hemodynamics for outpatient monitoring. Proceedings of the international symposium “Reliability and Quality”. 2019. vol. 2. pp. 225-227. [in Russian]
- Teregulov YuE. Integral indicators of central hemodynamics in healthy individuals and patients with hypertension, depending on the type of hemodynamics. Practical medicine. 2012.8-2(64):164-8. [in Russian]
- Mikhail А. Yakushin, Roman V. Gorenkov, Olga G. Dvorina, Sergey Y. Yarotsky. Prospects for cardiovascular system telemonitoring in solving tasks in Federal National Project “Generation Seniors”. Cardiometry. November 2020; 17:39-48; DOI: 10.12710/cardiometry.2020.17.3948
- Bokarev IN, Matvienko EV. Modern approaches to the treatment of primary arterial hypertension. Clinical medicine. 2013;91(3):4-8.


