Mortality from circulatory system diseases in the Kabardino-Balkarian Republic in 2015-2019
Автор: Kаrdаngushevа A.M., Dokhova M.T., Budnik A.F., Pshukova A.A., Kardanova L.D., Zhirikov Z.A., Voronova O.V., Kardanov M.A.
Журнал: Cardiometry @cardiometry
Статья в выпуске: 18, 2021 года.
Бесплатный доступ
Aim of the study is to analyze the mortality rates of the population of the Kabardino-Balkarian Republic (KBR) from circulatory system diseases (CSD) for the period 2015-2019 to determine measures to reduce the mortality of the population of the Republic.
Mortality, causes of death, diseases of the circulatory system, icd-10, kabardino-balkarian republic
Короткий адрес: https://sciup.org/148321535
IDR: 148321535 | DOI: 10.18137/cardiometry.2021.18.9299
Текст научной статьи Mortality from circulatory system diseases in the Kabardino-Balkarian Republic in 2015-2019
Aksana M. Kаrdаngushevа, Madina T. Dokhova, Antonina F. Budnik, Albina A. Pshukova, Leila D. Kardanova, Artur V. Zhirikov, Olga V. Voronova, Marat A. Kardanov. Mortality from circulatory system diseases in the Kabardino-Balkarian Republic in 2015-2019. Cardiometry; Issue 18; May 2021; p.92-99; DOI: 10.18137/cardi-ometry.2021.18.9299; Available from: issues/no18-may-2021/circulatory-system-diseases
Circulatory system diseases (CSD) are the leading cause of death both worldwide and in the Russian Federation. Despite the trend in the last decade towards a decrease in the share of deaths from CSD, the mortality rates for this class of diseases in the Russian Federation exceed the corresponding indicators of all economically developed countries [1, 2]. Ischemic heart disease (IHD) and cerebrovascular diseases (CVD) occupy the main positions in the structure of mortality from CSD among cardiovascular diseases leading to death [3-5]. It is known that the level and dynamics of mortality from CSD have some regional characteristics. It is also known that the structure and dynamics of mortality can be influenced by two groups of causes. The first group thereof includes the frequency of CSD risk factors, the implementation of preventive programs, the development of modern medical technologies, the quality and availability of medical care, and the patient adherence to treatment. The second group thereof is associated with the sys- tem of official registration of deaths from CSD, which includes the knowledge and ability of doctors to use the proper coding rules to properly select the initial cause of death and methods of formulating a postmortem clinical diagnosis [5]. The CSD prevention issues are the subject of close attention paid by the regional authorities in the Kabardino-Balkarian Republic. Currently, the Kabardino-Balkarian Republic (KBR) is implementing its regional projects “Combating cardiovascular diseases (Kabardino-Balkarian Republic)” and “Forming a system of motivating citizens to a healthy lifestyle, including healthy eating style and rejection of bad habits (Kabardino-Balkarian Republic)” within the framework of the relevant Federal Projects. There is no doubt that the planning and execution of interventions aimed at reducing CSD mortality in KBR requires an assessment of the actual mortality levels and dynamics, a thorough analysis of the nosological structure of mortality and the factors influencing these indicators.
Purpose of the study is to analyze the mortality rates of the population of the Kabardino-Balkarian Republic (KBR) from circulatory system diseases (CSD) for the period 2015-2019 to determine measures to reduce the mortality in the population of the Republic.
Material and methods
The study was carried out in the Kabardino-Balkarian Republic, which occupies an area of 12,470 km2 (the 79th region of 85 regions). The resident population of the Republic as of January 1, 2019 is 868 350 people. The structure of the Republic's population at the beginning of 2018 is represented by 21.7% of the people under the working age, 57.4% of the people of working age and 20.9% thereof over working age [6]. For our analysis, we used the official Rosstat data on the number of deaths according to causes of death based on the applicable “Brief Classification of Causes of Death”. The level and dynamics of mortality of the population of the KBR, the share of these deaths in the total number of deaths in 2015 and 2019, the share of CSD in the structure of the total mortality of the population of the KBR, the nosological structure of causes of death of the CSD class, the share of each of the causes of death in the number of deaths from CSD, the level and the dynamics of mortality from CSD over a five-year period were studied. The study used non-standardized mortality rates. The mortality rates for 2019 are analyzed based on preliminary data for January-December 2019 (excluding final medical death certificates), due to the lack of updated data at the time of the study.
Results
In 2019, 7231 people died in the KBR (the mortality rate was recorded to be 833.8 per 100 thousand of the population), among which 3333 people died from CSD (the mortality rate was recorded to be 384.3 per 100 thousand population, and the share of deaths from all causes was 46, 1 %). From 2015 to 2019, there was a decrease in mortality from CSD (see Figure 1 herein), which led to a decrease in the share of the latter in the structure of all-cause mortality from 55.6% in 2015 to 46.1% in 2019.
The nosological structure of the causes of death of the CSD class in 2015 and 2019 and the share of each of the causes of death as the numbers of deaths from CSD are presented in Table 1 herein.
CVD (I60-I69) and IHD (I20-I25) made a significant contribution to mortality from CSD. The share of CVD in the structure of mortality from CSD remained high throughout the analysis period with a slight decrease from 38.1% in 2015 to 34.5% in 2019. At the same time, the share of acute disorders of cerebral circulation (I60-I64) in the structure of mortality in different years was 45.3-38.8% of CVD (see Figure 2 herein), and most of the deaths were attributed to other cerebrovascular diseases. Thus, the number of deaths from CVD (I41-I50) was 1151 people in 2019 (34.5% of all CSDs), and acute cerebrovascular accidents (I60-I64) caused the death of 475 people, which was 14.3% of all deaths from CSD and 41.3% of all deaths from CVD.
The share of deaths from chronic atherosclerotic and other lesions of cerebrovascular vessels, which included “Cerebral atherosclerosis”, “Other specified lesions of cerebral vessels”, “Cerebrovascular disease, unspecified”, “Sequelae of cerebrovascular diseases”, “Other cerebrovascular encephalopathy” accounted for 20.3% of deaths from CSD and 58.7% of deaths from CVD. In 2015, acute disorders of cerebral circulation (I60-I64) caused the death of 724 people that accounted for 17.3% of all deaths from CSD and 45.3% of all deaths from CVD. The percentage of deaths from chronic atherosclerotic and other lesions of cerebrovascular vessels was 20.8% of all deaths from CSD and 54.8% of all deaths from CVD. In 2019, compared to 2015, there was an increase in mortality from cerebral infarction (I63), hypertensive
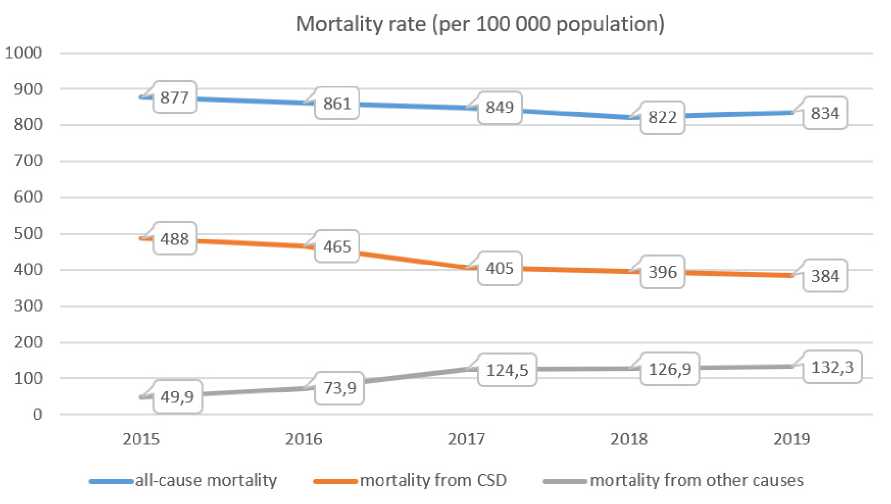
Figure 1. Dynamics of total mortality, mortality from CSD and other death causes of the population in the Kabardino-Balkarian Republic for the period 2015-2019
Table 1
The numbers and shares of deaths from CSD in 2019 compared to 2015
|
Brief classification of causes of death |
ICD 10 |
Causes of death |
The absolute number of deaths in 2019 |
Share (%) of deaths from CSD in 2019 |
The absolute number of deaths in 2015 |
Share (%) of deaths from CSD in 2015 |
|
121 |
I00-I02 |
Acute rheumatic fever |
0 |
0 |
0 |
0 |
|
122 |
I05-I09 |
Chronic rheumatic heart diseases |
16 |
0,48 |
9 |
0,21 |
|
123 |
I11 |
Hypertensive heart disease |
203 |
6,09 |
161 |
3,83 |
|
124 |
I12 |
Hypertensive chronic kidney disease |
1 |
0,03 |
0 |
0 |
|
125 |
I13 |
Hypertensive heart and chronic kidney disease |
5 |
0,15 |
3 |
0,07 |
|
123-125 |
I11- I13 |
Hypertensive heart and CKD with heart failure and /or CKD |
209 |
6,27 |
164 |
3,91 |
|
126 |
I10 |
Essential (primary) hypertension |
17 |
0,51 |
41 |
0,98 |
|
123-126 |
I10- I13 |
Hypertensive diseases |
226 |
6,78 |
205 |
4,88 |
|
127 |
I21 |
ST elevation (STEMI) and non-ST elevation (NSTEMI) myocardial infarction |
137 |
4,11 |
114 |
2,71 |
|
128 |
I22 |
Subsequent ST elevation (STEMI) and non-ST elevation (NSTEMI) myocardial infarction |
6 |
0,18 |
21 |
0,50 |
|
Brief classification of causes of death |
ICD 10 |
Causes of death |
The absolute number of deaths in 2019 |
Share (%) of deaths from CSD in 2019 |
The absolute number of deaths in 2015 |
Share (%) of deaths from CSD in 2015 |
|
127-128 |
I21- I22 |
Myocardial infarction |
143 |
4,29 |
135 |
3,21 |
|
129 |
I25.1 |
Atherosclerotic heart disease |
236 |
7,08 |
444 |
10,57 |
|
130 |
I25.0 |
Atherosclerotic cardiovascular disease, so described |
24 |
0,72 |
67 |
1,60 |
|
131 |
I25.9 |
Chronic ischemic heart disease, unspecified |
173 |
5,19 |
185 |
4,40 |
|
132 |
I25.2-.6,.8 |
Other forms of chronic ischemic heart disease |
81 |
2,43 |
82 |
1,95 |
|
133 |
I20, I24.1-.9 |
Other forms of acute ischemic heart disease |
67 |
2,01 |
128 |
3,04 |
|
127-133 |
I20- I25 |
Coronary heart disease |
724 |
21,72 |
1041 |
24,79 |
|
134 |
I26-I28 |
Pulmonary heart disease and diseases of pulmonary circulation |
295 |
8,85 |
288 |
6,86 |
|
135 |
I42.6 |
Alcoholic cardiomyopathy |
23 |
0,69 |
96 |
2,29 |
|
136 |
I42.9 |
Cardiomyopathy, unspecified |
63 |
1,89 |
1 |
0,02 |
|
137 |
I51.5 |
Myocardial degeneration |
8 |
0,24 |
52 |
1,24 |
|
138 |
I50.9 |
Heart failure, unspecified |
83 |
2,49 |
91 |
2,17 |
|
139 |
I46.1 |
Cardiac arrest |
31 |
0,93 |
50 |
1,19 |
|
140 |
I30-I41, I42.0-.5,.7,.8, I43-I45, I46.0,.9, I47- I49, I50.0,1, I51.0-.4, I51.6-.9 |
Other heart diseases |
73 |
2,19 |
67 |
1,60 |
|
141 |
I60 |
Subarachnoid hemorrhage |
29 |
0,87 |
41 |
0,98 |
|
142 |
I61-I62 |
Nontraumatic intracerebral hemorrhage and other and unspecified nontraumatic intracranial hemorrhage |
95 |
2,85 |
212 |
5,05 |
|
143 |
I63 |
Cerebral infarction |
295 |
8,85 |
241 |
5,73 |
|
144 |
I64 |
Stroke not specified as hemorrhage or infarction |
56 |
1,68 |
230 |
5,47 |
|
145 |
I67.2 |
Cerebral atherosclerosis |
283 |
8,49 |
700 |
16,67 |
|
146 |
I67.4 |
Hypertensive encephalopathy |
11 |
0,33 |
2 |
0,05 |
As to IHD, chronic rather than acute forms of this pathology were recorded as the cause of death (see Figure 2 herein). The number of deaths from IHD in 2019 was 724 (21.7% of all CSD deaths), including 143 deaths from myocardial infarction (acute MI and recurrent AMI) and 67 deaths from other forms of acute ischaemic heart disease (6.3% of all CSD deaths). The percentage of deaths from the causes “Atherosclerotic heart disease” (I25.1) and “Atherosclerotic cardiovascular disease so described” (I25.0), “Chronic ischaemic heart disease, unspecified” (I25.9) and “Other forms of chronic ischaemic heart disease” (I25.8) in 2019 was 15.4% of all CSD deaths. The vast majority of 96 | Cardiometry | Issue 18. May 2021
the IHD deaths (74.7% of all IHD deaths in 2015 and 71% of all IHD deaths in 2019) should be attributed to nonacute coronary events. Compared to 2015, an increase in deaths from chronic coronary heart disease, unspecified (I25.9), other forms of coronary heart disease (I25.2-.6,.8) and acute myocardial infarction (I21) were recorded in 2019 against a background of decreasing mortality from IHD (I20-I25) and most causes of that group.
All other causes of death from CSD accounted for 1,458 deaths in 2019 (43.7% of all CSD deaths) and 1,559 deaths in 2015 (37.1% of all CSD deaths). Among those, an increase in the number of deaths in 2019 compared to 2015 was recorded from hypertension with heart failure and CKD, chronic rheumatic heart disease, pulmonary heart disease and pulmonary circulatory disorders, unspecified cardiomyopathy, unspecified heart failure, other heart diseases, atherosclerosis, other arterial, arteriolar and capillary diseases, phlebitis and thrombophlebitis, thrombosis and embolism and other diseases of veins and lymphatic vessels. There was a decrease in the number of deaths in the other cases.
The dynamics of mortality from CVD, IHD and hypertension for the period 2015-2019 is shown in Figure 2 herein. Over the five-year period of our analysis, a decrease in mortality from acute cerebrovascular accidents (I60-I64) was revealed. Moreover, the greatest decrease in mortality took place in 2017 compared to 2016. There was a decrease in mortality from hypertension (I10-I13) from 23.8 per 100 thousand population in 2015 to 12.2 per 100 thousand population in 2018 with a subsequent increase to 26.1 per 100 thousand population in 2019. The lowest death rate from myocardial infarction was recorded in 2017 (15.3 per 100 thousand population) with an increase to 16.5 per 100 thousand population in 2019.
Discussion
As can be seen from the data presented herein, mortality from CSD and some selected causes, included in the CSD class, decreased in the Republic in the period between 2015 and 2019. The decrease in mortality is certainly a favorable factor and may indicate the effectiveness of prevention and treatment programs. However, attention should be paid to the increase in mortality for a number of reasons. Of particular practical importance is the increase in mortality from hypertensive heart and CKD with heart failure and /or CKD or ERSD hypertension. It can be assumed that the multidirectional dynamics in the causes of death from CSD is associated with an approach to determining the leading cause of death and coding the causes of death. Among the possible reasons for the decline in mortality from CSD, the possibility of the effect of distortion of statistical data on mortality rates is widely discussed. S.A. Boytsov, A.G. Vishnevsky, O. M. Drapkina, E.P. Kakorina, I.V. Samorodskaya, V.Yu. Semenov repeatedly pointed to the distortion of the statistics of mortality from CSD and individual causes of the CSD class by “transferring” deaths from one class of causes to another [1, 3-5, 7, 8]. The decrease in the mortality rates from CSD (-103.2 per 100 thousand population) in our analysis was proportional to the increase in mortality from the class of diseases according to the applicable ICD-10 R00-R99 code “Symptoms, signs, abnormal clinical and laboratory findings, not elsewhere classified” (+82.4 per 100
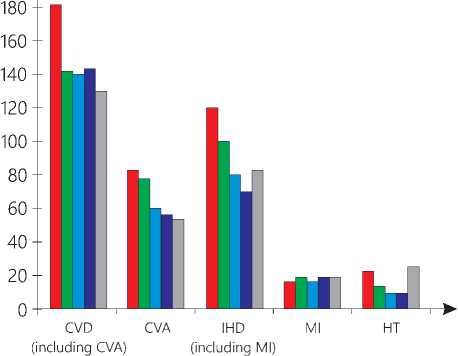
■ 2015 ■ 2016 ■ 2017 ■ 2018 □ 2019
Figure 2. Dynamics of mortality of the population in KBR from CSD for the period 2015-2019 (per 100 thousand population). Legend: CVD - cerebrovascular disease, CVA - acute cerebrovascular accident, IHD - ischemic heart disease, MI - myocardial infarction, HT - hypertension thousand population). The increase in mortality from causes of the class of diseases according to the code ICD-10 R00-R99 “Symptoms, signs abnormal clinical and laboratory findings, not elsewhere classified” took place due to the diagnosis “Old age” (R54). Thus, the share of deaths according to the code R54 ICD-10 “Old age” among all deaths was only 3.3% in 2015 (28.9 per 100 thousand of the population) and 13.3% in 2019 (82.4 per 100 thousand population).
It is known that mortality rates can be influenced by the age structure of the population. The low rates of mortality from CSD in KBR and its decrease over a five-year period, as well as an increase in mortality due to “Old age” (ICD-10 code R54) can be explained by changes in the demography of KBR, which has resulted in an increase in the number of people over working age by 65, 7 thousand people from 1990 to 2018 and by 16.1 thousand people from 2015 to 2018 [6]. Despite the negative changes in the demography of KBR, the share of the population over 65 years old at the beginning of 2018 was recorded to be 11%, and the share of people over working age was 20.9%. The impact of approaches to coding the original cause of death cannot be ignored. O.M. Drapkina and co-authors explain the widespread increase of mortality due to “Old age” by the introduction of the relevant recommendations of the Russian Ministry of Health on the use of this coding as the cause of death (Letter No 14-
9/10/2-4150 dd. 26.11.11 issued by the Russian Federation Ministry of Health Care; Letter No 13-2/1750 dd. 19.12.14 “On the Procedure of Using the Term 'Old Age' in Mortality Statistics” issued by the Russian Ministry of Health Care) [5]. The authors also point out that most elderly people in the Russian Federation die at home that reduces the possibility of verifying the diagnosis [5]. This is because the diagnosis of many diseases requires special diagnostic methods that may not be available or possible if the patient comes in late. On this basis, it can be assumed that this code used contributes significantly to the distortion of the pattern of the death statistics. This hypothesis needs to be tested by a clinical and epidemiological study. Certainly, the results of our study only allow us to identify the range of possible factors influencing the level and pattern of the CSD mortality. In our opinion, a retrospective analysis of the approaches to the determination of the causes of death in the Republic will make it possible to identify the coding errors of the original cause of death.
Researchers note repeatedly that modern scientific publications on clinical cardiology do not use diagnosis formulations such as “Atherosclerotic cardiovascular disease, so described” (I25.0 ICD10), “Atherosclerotic heart disease” (I25.1 ICD-10). In practice, these codes are used in cases of death in the elderly who have not sought medical advice by a health care provider (5). In other words, these codes indicate that the cause of death is unknown.
The increase in mortality from myocardial infarction and from hypertension with heart failure and CKD, together with the high share of CVD in the mortality structure, obtained in our study, indicates the need to strengthen the prevention and treatment of these categories of patients. The decrease in the percentage of deaths from stroke not specified as haemorrhage or infarction (I64) among CSD is a favorable trend which is associated with the introduction of modern protocols and advanced diagnostic techniques (computed tomography, magnetic resonance imaging) into practice.
Full assessment of the cardiological health state in the population of the Republic, the identification of the priorities of targeted prevention is possible only based on the results of epidemiological studies. The study of the prevalence of CSD and CSD risk factors is the most important step towards an objective assessment of the situation, identification of the regional features of public health and management of medical care followed by the subsequent development and implementation of targeted preventive measures.
Limitations of the study
The paper have used data supplied by the official medical statistics, which do not fully reflect the nosological structure of mortality. This is due to the fact that when the initial cause of death is selected, only one of the present diseases is coded in the patient suffered from. The mortality statistics system in use does not take into account comorbidities, does not allow assessing the actual contribution of certain individual diseases and risk factors to the level and structure of mortality, therefore it does not allow properly evaluating the effectiveness of regional programs for the prevention and treatment of CSD to be assessed. In other words, the data from official medical statistics can only, with certain limitations, reveal the problems on which the efforts of the health care system and other services need to be focused in order to reduce mortality rates. Recording of the initial cause of death only and the omission of comorbidities from the accounting system make mortality analysis unsuitable for assessing the management of medical care at all stages of its provision and its resource allocation and assignment. At the same time, the lack of the possibility of obtaining the real picture using data from official statistics justifies the need for an epidemiological study in the Republic, the results of which will give the actual situation with CSD and make it possible to implement preventive measures more effectively and use resources rationally when providing specialized medical care.
Conclusion
The mortality rate from CSD in 2019 decreased by 103.2 per 100 thousand people compared with 2015, while maintaining the leading position in the mortality structure of the Republic's population. The identified regional peculiarities of mortality from CSD can be used in the development and implementation of a set of measures to improve medical care for patients with CSD, as well as in improving approaches to properly determining the causes of death. An epidemiological study in KBR, the results of which will provide a realistic picture of the prevalence of CSD, appears to be an important step towards the development and implementation of preventive programs properly adapted to the needs of the region.
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Mortality from circulatory system diseases in the Kabardino-Balkarian Republic in 2015-2019
- Vishnevsky AG, Andreev EM, Timonin SA. Mortality from cardiovascular diseases and life expectancy in Russia. Demographic Review. 2016(1):6-34.
- Boytsov SA, Samorodskaya IV. High Cardiovascular Mortality in Russia: Are Approaches to Coding Causes of Death Adequate? Cardiology. 2015(1):47-51.
- Samorodskaya IV, Starinskaya MA, Semyonov VYu, Kakorina EP. Nosologically and age-stratified mortality structure from cardiovascular diseases in the years 2006 and 2014. Russian Journal of Cardiology. 2016(6;134):7-14. DOI: 10.15829/1560-4071-2016-6-7-14
- Semyonov VYu, Samorodskaya IV, Starinskaya MA, Boytsov SA. Nosological structure of mortality from diseases of the circulatory system of the population in three age groups of the population of the Russian Federation. Health Manager. 2018(5):31-41.
- Drapkina OM, Samorodskaya IV, Starinskaya MA, Masyakin AV, Kazakovtsev BA, Stupakov IN. Comparison of mortality from circulatory system diseases and nervous and mental disorders in Russia in 2013 and 2017. The Russian Journal of Preventive Medicine. 2019(22;4):7-13. DOI: 10.17116/profmed2019220417
- Gashtova AA, Aleksanova NV, Afashokova KM, Zemlyakova AA, Kisheva IN, Malamusova MKh, Guzeeva AR. Kabardino-Balkarian Republic. 2019: Statistical collection. OP of the North Caucasusstat on KBR, edited by N.V. Skorkina. N. 2019.
- Drapkina OM, Samorodskaya IV, Starinskaya MA, Boytsov SA. Comparison of Russian regions by standardized mortality rates from all causes and circulatory system diseases in 2006-2016. The Russian Journal of Preventive Medicine and Public Health. 2018(21;4):4-12. DOI: 10.17116/profmed20182144
- Resolution of the round table on the topic "Contribution of circulatory system diseases to the structure of total mortality: issues and problems". May 11, 2016. Moscow. The Russian Journal of Preventive Medicine and Public Health. 2016(19;3):58-61. DOI: 10.17116/profmed201619358-61


