Недержание мочи и инфравезикальная обструкция: Сцилла и Харибда женской урологии. Роль методов биологической обратной связи
Автор: Кукушкина Л.Ю., Ромих В.В., Сивков А.В., Каприн А.Д.
Журнал: Экспериментальная и клиническая урология @ecuro
Рубрика: Нейроурология
Статья в выпуске: 3 т.17, 2024 года.
Бесплатный доступ
Высокая распространенность нарушений мочеиспускания у женщин, как молодого, так и старшего возраста, обуславливает актуальность этой медицинской и социальной проблемы. Наиболее частыми видами являются недержание мочи различной степени тяжести и функциональная инфравезикальная обструкция. Данные нарушения приводят к снижению качества жизни, психоэмоциональному дискомфорту, что обуславливает необходимость оказания таким пациенткам ранней лечебно-диагностической помощи. Лекция посвящена состоянию проблемы нарушений мочеиспускания, а также обзору основных и перспективных методов лечения. Так как в основе дисфункции мочеиспускания у женщин значительную роль играет нарушение функционирования мышц тазового дна, методы лечения этих расстройств связаны с восстановлением мышечного тонуса тренировочными или медикаментозными средствами или механической поддержкой тазовых органов хирургическими средствами. В данной лекции представлено научное обоснование клинических эффектов тренировочных техник лечения нарушений мочеиспускания. Комплексный подход, в том числе с использованием тренировочных методов, позволяет достигнуть оптимальных результатов лечения как при недержании, так и при инфравезикальной обструкции у женщин.
Недержание мочи, тренировки мышц тазового дна, биологическая обратная связь, дисфункциональное мочеиспускание, инфравезикальная обструкция
Короткий адрес: https://sciup.org/142243277
IDR: 142243277 | DOI: 10.29188/2222-8543-2024-17-3-68-79
Текст научной статьи Недержание мочи и инфравезикальная обструкция: Сцилла и Харибда женской урологии. Роль методов биологической обратной связи
экспериментальная и клиническая урология № 3 2024
Лечение нарушений мочеиспускания у женщин является проблемой, широко обсуждаемой в медицин ских кругах, а последствия несвоевременного и некор ректного выбора лечебной тактики или неверного начала лечения делают данную проблему актуальной для исследований. Врачи многих специальностей – урологи, гинекологи, проктологи так же, как неврологи и реабилитологи сталкиваются с проблемами наруше ния мочеиспускания в своей практике. Лечение нару шений мочеиспускания – это растущий и непрерывно совершенствующийся сектор медицинской индустрии. Опубликовано большое количество работ, посвящен ных данной проблеме. Для лечения нарушений мочеиспускания используют значительный арсенал методов, имеющих как достоинства, так и ограниче ния.
В связи с этим совершенствование методов лече ния нарушений мочеиспускания является актуальной задачей современной функциональной женской уроло гии.
Распространенность нарушений мочеиспускания у женщин. Виды и терминология
По данным литературы приблизительно 24% жен щин до 60 лет и более 50% женщин старше 60 лет ис пытывают проблемы,связанные с нарушением акта мочеиспускания [1]. По данным различных авторов, распространенность симптомов нарушенного мочеис пускания среди женщин в США достигает 37%, в Ев ропе – 26%, в Великобритании – 29%, в странах восточного региона (Сингапур, Пакистан, Тунис) – 20% [2]. Различна и обращаемость за медицинской по мощью данной категории женщин. Во Франции она со ставляет 33%, в Германии – 40%, в Испании – 24%, в Великобритании – 25% [3].
В России распространенность нарушений моче испускания у женщин составляет примерно 36%, а об ращаемость пациенток за медицинской помощью сравнительно невысока [4]. В последние годы намети лась положительная тенденция увеличения числа об ращений пациенток с нарушениями мочеиспускания за высококвалифицированной медицинской помощью. Особенно актуальна эта проблема для женщин, стра дающих недержанием мочи. В нашей стране до послед него времени ее обсуждать было не принято.Многие женщины испытывали стеснение при обращении к врачу со столь «интимной проблемой». Было распро странено заблуждение,что это обычное состояние для рожавших и женщин старшего возраста, а также что оно неизлечимо и т.п. [5]. Однако, недержание мочи не является естественным признаком старения. Оно может встречаться и у молодых женщин, в том числе во время беременности, а также в раннем послеродо вом периоде.
Высокая распространенность нарушений мочеис пускания у женщин, как молодого, так и старшего воз раста, обуславливает актуальность этой медицинской и социальной проблемы.
Наиболее частыми видами нарушений мочеиспус кания являются недержание мочи различной степени тяжести и функциональная инфравезикальная об струкция, часто обозначаемая как дисфункциональное мочеиспускание.
Недержание мочи
Согласно определению Международного общества по проблемам недержания мочи (International Conti nence Society (ICS)), недержание мочи – это непро извольное вытекание мочи по уретре.Выделяют три вида недержания: стрессовое, ургентное и смешанное. Недержанием мочи страдают 6-10% населения и 1/3 женщин [6]. По терминологии ICS стрессовое недержа ние мочи – это непроизвольное подтекание мочи при напряжении, физической нагрузке (исключая спортив ные нагрузки) или при чихании и кашле. Стрессовое недержание мочи выявляют у 25-70% женщин [7].
Согласно данным российских публикаций, недер жание мочи при напряжении наблюдали у 19% жен щин из общего числа обратившихся за помощью в урологическую клинику [5]. Симптомы заболевания выявляли у каждой 10–15-й больной при обращении в женскую консультацию. Согласно нашим ранее опуб ликованным данным,частота клинических симптомов недержания мочи у женщин старше 25 лет достигает 30% случаев [8]. Самым распространенным видом не держания мочи по-прежнему остается стрессовая форма. У женщин старше 50 лет распространенность клинических симптомов возрастает в 2,5 раза, дости гая 70% [9].
Имеются данные, что физическая активность уве личивает риск развития стрессового недержания мочи у женщин, хотя патофизиологические механизмы этого влияния неясны. У спортсменок, занимающихся спортом с тяжелыми физическими нагрузками,дис функцию мочеиспускания отмечают чаще, чем в общей популяции женщин.
Наличие недержания мочи существенно влияет на психологическое состояние женщины.Часто разви вается депрессия и постоянная тревожность, происхо дит снижение половой активности и работоспособ ности. В итоге, это приводит к значительному ухудше нию качества жизни [10].
При этом,далеко не все женщины,страдающие недержанием мочи, обращаются за медицинской помо щью, так как многие даже не предполагают, что это за болевание можно не только контролировать, но и лечить. По данным M. Sjöström и соавт., обращаемость к врачу в европейских странах не превышает 25%, а лечение получают только 6% женщин. Признано, что эффективность лечения во многом зависит от своевременности обращения за медицинской помощью:чем раньше начата терапия, тем лучших результатов можно добиться [11].
Функциональная инфравезикальная обструкция (дисфункциональное мочеиспускание)
Функциональную инфравезикальную обструкцию (фИВО) или дисфункциональное мочеиспускание у женщин в настоящее время рассматривают, как важную медицинскую проблему, о чем свидетельствует выделение этой темы в рекомендациях Европейской ассоциации урологов (EAU) в отдельную главу [12]. Согласно терминологии ICS, дисфункциональное мочеиспускание определяют, как прерывистое или неравномерное выделение мочи вследствие непроизвольных периодических сокращений периуретральных поперечнополосатых мышц в процессе мочеиспускания у неврологически здоровых пациенток.
Определение, терминология и классификация ИВО у женщин такие же, как для мужчин, что отражено в материалах комитета стандартизации ICS. Несмотря на то,что у женщин преобладают симптомы накопления, нередко они предъявляют жалобы и на задержку мочеиспускания, вялое мочеиспускание и чувство неполного опорожнения мочевого пузыря.При уродинамическом исследовании выявляют низкие показатели скорости мочеиспускания и повышенные значения объема остаточной мочи.
В отличие от проблемы недержания мочи, в специальной литературе встречаются лишь отдельные сообщения, посвященные попыткам стандартизации жалоб женщин с ИВО. A.J. Flisser, J.G. Blaivas указывают, что у пациенток со значительной обструкцией показатель шкалы IPSS (International Prostate Symptom Score – международная система суммарной оценки симптомов болезней предстательной железы в баллах) достоверно выше,чем при незначительной или умеренной обструкции. Средний показатель выраженности симптомов в группе с обструкцией составил 15,8±8,4 балла против 10,3±6,4 у женщин со стрессовым недержанием мочи и 2,1±2,7 – у здоровых жен-щин.Некоторые авторы считают возможным применение шкалы IPSS при симптомах нарушенного мочеиспускания у женщин. Такая шкала получила название IPSS women (IPSSw) [13].
Диагноз фИВО ставят после исключения механической причины обструкции,обусловленной такими клиническими состояниями, как цистоцеле, пролапс органов малого таза, стеноз и дивертикул уретры, предшествующие операции на органах таза, в том числе по поводу недержания мочи. Также необходимо исключить гипотонию мочевого пузыря,что опреде ляют при сопоставлении значений детрузорного дав ления и скорости мочеиспускания. Для упрощения оценки сократимости детрузора используют номо граммы Abrams-Griffiths и часто номограммы Blaivas-Groutz [14].
Нередко диагностика дисфункционального моче испускания требует специальных методов исследова ния, таких как видеоурография, электромиография или изучение профиля давления уретры в дополнение к стандартному определению и сопоставлению данных микционной цистометрии.Предложен метод диагно стики этого состояния только на основании исследо вания с определением плато детрузорного давления. На основании этого показателя, с последующим расче том индекса обструкции нижних мочевых путей (BOOI) и разницы между максимальным давлением детрузора и максимальными значениями давления детрузора при максимальном потоке мочи (Pdetmax-pdetQmax), диагноз дисфункционального мочеиспус кания устанавливают у 86% женщин с расстройством мочеиспускания [15].
По данным R. Terlikowski и соавт., обструкцию функционального генеза выявляют у 30-40% пациен ток с симптомами затрудненного мочеиспускания [16].
Распространенность фИВО у женщин варьирует в широких пределах от 2,7 до 29% [17]. Столь значи тельная разница показателей, во многом, связана с не однозначностью определений и отсутствием общепринятого диагностического алгоритма выявления инфра везикальной обструкции (ИВО). В зависимости от выбранного уродинамического критерия,частота вы явления ИВО у пациенток с симптомами нарушения функции нижних мочевых путей колеблется от 2 до 8% [18]. По данным большинства исследователей, частота выявления ИВО, в том числе функционального харак тера, зависит от возраста [19]. У 16% пациенток при чину ИВО точно установить не удается [20]. В этом случае говорят об «идиопатической инфравезикальной обструкции».
Несмотря на проводимое лечение, при выявлении дисфункционального мочеиспускания у девочек-под ростков в 40% случаев дисфункция сохраняется во взрослом возрасте [21].
Патофизиологические аспекты развития нарушений мочеиспускания
В обеспечении нормальной функции тазовых ор ганов существенную роль играет мышечно-связочный аппарат малого таза, обеспечивающий механическую поддержку тазовых органов,их нормальное взаимо расположение и механизм удержания мочи и кала. Раз личные варианты дисфункции мочеиспускания часто связаны с нарушением поддерживающей функции та зового дна.
Основными мышцами, формирующими тазовое дно, являются: мышца, поднимающая задний проход – лобково-копчиковая мышца, она же лобково-проста тическая (у мужчин); лобково-влагалищная; лобково анальная; лобково-ректальная; подвздошно-копчи ковая (идет от сухожильной дуги к нижним копчико вым позвонкам ниже лобково-копчиковой мышцы); седалищно-копчиковая мышца. Взаиморасположение основных мышц тазового дна, связок и тазовых орга нов представлено на рис. 1.
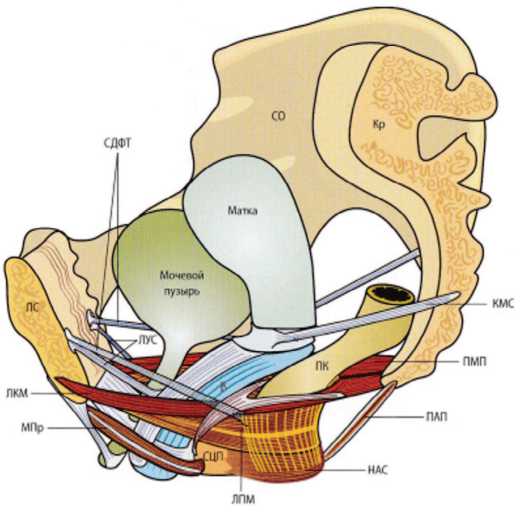
Рис. 1. Схема мышечно-связочного аппарата малого таза [22]. Обозначения: ЛС – лобковый симфиз, Кр – крестец, ЛКМ – лобково-копчиковая мышца, ПМП – поднимающая мышечная пластина, ПМА – продольная мышца ануса, ЛПМ – лобково-прямокишечная мышца, ЛУС – лобково-уретральная связка, СДФТ – сухожильная дуга фасции таза, КМС – крестцово-маточная связка, КСМ – кардиальная связка матки, ЛШФ – лобково-шеечная фасция, ВПФ – влагалищно-прямокишечная фасция, СЦП – сухожильный центр промежности, НАС – наружный анальный сфинктер
Fig. 1. Scheme of the muscular-ligamentous apparatus of the small pelvis [22] Designations: ЛС – pubic symphysis, Кр – sacrum, ЛКМ– pubococcygeus muscle, ПМП – levator muscular plate, ПМА – longitudinal muscle of the anus, ЛПМ – puborectalis muscle, ЛУС – pubourethral ligament, СДФТ – tendinous arcus of the pelvic fascia, КМС – sacrouterine ligament, KСМ – cardiac ligament of the uterus, ЛШФ– pubocervical fascia, ВПФ – vaginal-rectal fascia, СЦП – tendinous center of the perineum, НАС – external anal sphincter
Согласно интегральной теории P.E. Petros и U. Ulmsten, именно взаимодействие тазовых мышц и связок таза обеспечивает механизм удержания мочи. Нагрузка на связочный аппарат таза ведет к постепен ному его растяжению, что нарушает механизм удержа ния мочи. В конечном итоге, это может приводить к изменению топографии органов малого таза и нару шению их функции,в том числе к дисфункции моче испускания в виде недержания мочи или инфраве зикальной обструкции, а также к другим нарушениям таким как пролапс тазовых органов, недержание кала сексуальная дисфункция, диастаз прямых мышц жи вота, хроническая тазовая боль [23].
Ослабление мышечно-связочного аппарата ведет к опущению мочевого пузыря и изменению взаимо расположения шейки мочевого пузыря, уретры и вла галища. Хотя влагалище в норме не участвует в поддержании расположения мочевого пузыря, при опущении мочевого пузыря влагалище становится его опорой.Опущение передней стенки влагалища спо собствует дисфункции везико-уретрального сегмента и непроизвольному подтеканию мочи. Фиксация верх него отдела влагалища восстанавливает функцию удержания мочи.
Основным фактором развития дисфункции тазо вого дна у женщин считается возраст. После наступ ления менопаузы частота развития недержания мочи, опущения тазовых органов и других видов дисфунк ции мочеиспускания возрастает. К причинам этих рас стройств относят ослабление сфинктера уретры, мышц тазового дна, а также слабость фасциального и связочного аппарата таза.
В формировании дисфункции тазового дна также могут играть роль генетические факторы,такие как коллагеновая недостаточность, в том числе I и III типов. По данным некоторых исследователей, обнару жена прямая взаимосвязь генетических дефектов и стрессового недержания мочи. Появляются публика ции, подтверждающие роль полиморфизма гена COL3A1 в развитии этого состояния [24].
Подтверждением роли дисфункции мышц тазо вого дна в развитии симптомов нарушенного мочеис пускания является исследование L.P. Cacciari и соавт., в котором приняли участие 23 женщины с недержа нием мочи и 31 женщина без недержания. В исследо вании определяли профили влагалищного давления с использованием мультисенсорного устройства Pliance. Проводили регистрацию профиля давления в 10 участках вдоль влагалища. У женщин с недержанием мочи выявили более низкое вагинальное давление в покое и сниженную возможность поддерживать на пряжение мышц в течение определенного времени. Особенно большая разница между группами выявлена в средней части влагалища на расстоянии 3-4 см от его входа, что соответствует проекции мышц тазового дна [25].
В основе фИВО лежит гиперактивность мышц, участвующих в регуляции мочеиспускания (наружный сфинктер мочевого пузыря, лонно-копчиковая мышца, являющаяся частью мышцы, поднимающей анус), что было продемонстрировано в ряде исследований, в том числе с применением метода электромиографии. По казано, что затруднение мочеиспускания связано с не достаточным расслаблением уретры, шейки мочевого пузыря и мышц тазового дна во время акта мочеис пускания [26].
В норме продолжительное сокращение детрузора синхронизировано с релаксацией наружного сфинктера. «Неполноценная» работа периуретраль ных мышц во время мочеиспускания может явиться причиной функциональной обструкции. В свое время,это состояние получило название «ненейро генного нейрогенного мочевого пузыря» или син дрома Hinman. A. Groutz и соавт. считают, что более правильными терминами в этой ситуации являются «псевдодиссенергия» или «дисфункциональное моче испускание» [27]. Однако, наряду с этими терминами, широко используют и понятие фИВО, подчеркивая, что нарушением является именно функциональная обструкция.
Вероятной причиной мышечного гипертонуса могут быть нарушения мышечно-тонических реак ций, связанных как с заболеваниями органов таза, так и с дистрофическими или органическими пораже ниями позвоночника, учитывая, что органы, распо ложенные в полости таза и тазовое дно имеют общую систему иннервации. При этом все функции тазовых органов находятся под контролем центральной нерв ной системы (ЦНС), которая представляет собой сба лансированный механизм, но в определенных ситуациях предрасположенный к нейронной неустой чивости. Сбой, возникший в этой системе, может вы звать центральное функциональное нарушение или дисфункцию периферических нервов,в частности, органов таза. Такая взаимосвязь, в свою очередь, может привести к изменениям в ЦНС, в результате которых возникает нарушение обработки ноцицеп тивной сенсорной информации.
Косвенные указания на связь сбоев в ЦНС и дис функции мочеиспускания описаны в публикации J. Panicker и соавт., где изучена роль психологического состояния и наличия определенных функциональных неврологических симптомов в развитии фИВО. Уста новлено,что у женщин с дисфункциональным моче испусканием чаще выявляют симптомы депрессии и тревожности, а также ослабление мышц бедра. Ав торы полагают, что перенесенные стрессовые ситуа ции, особенно сексуального характера, повышают риск развития затрудненного мочеиспускания [28].
Методы лечения нарушений мочеиспускания у женщин
Консервативная терапия нарушений мочеиспускания
В основе дисфункции мочеиспускания у женщин значительную роль играет нарушение функциониро вания мышц тазового дна.В связи с этим основные методы лечения этих расстройств направлены на вос становление мышечного тонуса тренировочными или лекарственными средствами,а также восстановле нием механической поддержки тазовых органов хи рургическим путем.
Тренировочные подходы, укрепляющие мышцы тазового дна, являются методами лечения первой линии у женщин с дисфункцией мочеиспускания. Большинство женщин с недержанием мочи пред почитают именно этот вариант первичной терапии, и лишь немногие сразу соглашаются на хирургическое вмешательство.
При неэффективности тренировочных методов лечения назначают медикаментозную терапию с использованием препаратов различных механизмов действия. При недержании мочи применяют терапию М-холиноблокаторами, β3-адреномиметиками, антидепрессантами [29]. Отмечена высокая частота развития побочных эффектов лекарственной терапии, нередко приводящих к отказу от ее продолжения. Учитывая, что недержание мочи в большинстве случаев развивается у женщин в менопаузе при эстрогенной недостаточности, гинекологи широко применяют эстрогены в лечении стрессового недержания мочи, даже в режиме монотерапии, несмотря на то, что применение эстрогенов не обеспечивает необходимой эффективности, увеличивая риск возникновения сердечно-сосудистых заболеваний, злокачественных образований эндометрия и молочных желез [30].
Имеются немногочисленные работы, описываю щие применение лекарственной терапии при фИВО у женщин. Если причину функциональной обструкции определить не удается, то назначают средства, спо собствующие расслаблению наружного сфинктера уретры и усиливающие сократительную способность детрузора.
Проведены исследования по изучению неселек тивных (феноксибензамин) или селективных (альфу зозин, теразозин) α1-адреноблокаторов или М2-холи-номиметиков (бетанехол хлорид) [31]. Анализ этих данных указывает на низкую эффективность лекарст венной терапии.
Описан опыт применения малых доз миорелак сантов центрального действия,снижающих макси мальное внутриуретральное давление в зоне наружного сфинктера уретры, которое обычно повышено у женщин с ИВО функционального типа. Среди неже лательных явлений данного метода отмечают сниже ние артериального давления, головокружение и мышечную слабость.Эти препараты противопока заны при черепно-мозговой травме, сотрясениях го ловного мозга в анамнезе.Эффективность данного лечения не превышает 50% [32].
Хирургические методы лечения дисфункции мочеиспускания у женщин
При недостаточном эффекте консервативных методов терапии обычно прибегают к малоинвазив ному и хирургическому методам лечения.
У женщин с недержанием мочи используют такие малоинвазивные методы лечения как:парауретраль-ное введение объемообразующих субстанций на основе аутожира, препаратов коллагена, силикона и др. В последнее время широкое распространение получил метод парауретрального введения объемобразующего геля Bulkamid, который представляет собой гомогенный биосовместимый гидрогель (97,5% апирогенная вода и 2,5% полиакриламид). Эффективность его введения, составляет 65%. Через год наблюдения после введения повторные инъекции понадобились в 35% случаев [33].
Одним из вариантов малоинвазивного лечения у женщин с дисфункциональным мочеиспусканием является денервация сфинктера мочевого пузыря методом введения ботулотоксина. Ботулинотерапию можно рассматривать как метод терапии нарушенного мочеиспускания 3-й линии.
Применение ботулинического токсина при фИВО обладает высокой эффективностью.Основным показанием к проведению лечения данным методом является тяжелая степень функциональной обструкции. По данным НИИ урологии, средняя продолжительность действия ботулинического токсина при введении в зону наружного сфинктера уретры составляет от 3 до 8 месяцев,что влечет за собой необходимость неоднократных повторных введений [18, 32].
Y.H. Jiang и соавт. описали результаты видеоуро-графического обследования 81 женщины с дисфункциональным мочеиспусканием для выявления преимущественной локализации области обструкции с последующим введением ботулотоксина в эту зону. Эффективность данного метода составила 67,9%, авторы делают вывод о его высокой результативности [34].
При неэффективности малоинвазивного лечения прибегают к хирургическим вмешательствам, особенно при сочетании дисфункции мочеиспускания с пролапсом тазовых органов, поскольку восстановление нормальной топографии тазовых органов способствует устранению симптомов нарушенного мочеиспускания.
Для оперативного лечения недержания мочи у женщин предложено более 200 вариантов оперативных вмешательств. Эффективность большинства операций с использованием собственных тканей ограничена в силу изменений,приводящих к снижению их прочности и эластичности.Как известно,у женщин старшей возрастной группы, страдающих стрессовым недержанием мочи, снижена прочность и эластичность тканей тазового дна.Подобные изменения обуславливают неэффективность большинства вмешательств с использованием собственных тканей,на-правленных на восстановление функции тазового дна. В связи с этим при корректирующих операциях преимущественно используют синтетические материалы.
При недержании мочи наиболее частым вариан том малоинвазивной операции является установка среднеуретрального слинга (TVT, TVT-O), что в на стоящее время считают «золотым стандартом».Од нако, накопление опыта этих операций свидетель ствует, что их долгосрочная эффективность состав ляет около 60%, а необходимость повторных вмеша тельств возникает у 17,7% пациенток в течение последующих 5 лет [35]. По данным различных иссле дований, частота рецидивов или сохранение стрессо вого недержания мочи после слинговых операций в ближнесрочном периоде варьирует от 10 до 55%, а в течение 5 лет возрастает до 70% [36]. В то же время имеются более оптимистичные мнения.По данным исследований,проведенных в Англии и Шотландии, необходимость в повторных операциях возникает в 4 5% случаев [37]. По данным метаанализа, проведен ного F. Fusco и соавт., частота развития осложнений при слинговой уретропексии варьирует от 0,5 до 11,5%, хотя при использовании метода позадилонного слинга частота осложнений оказалась ниже, чем при установке трансобтураторного слинга [38].
Из других вариантов хирургической коррекции недержания мочи при сочетании с опущением тазо вых органов используют такие операции,как уретро суспензия, везикокольпосуспензия, а при выраженном пролапсе – везикосакропексию, цервикосакропек сию,в том числе с использованием сетчатых имплан татов.
Для восстановления нормального расположения везико-уретрального сегмента доказана целесообраз ность таких операций, как кольпосуспензия (операция Burch). Эффективность кольпосуспензии, по данным I. Giarenis и соавт., составила 85-93% [39].
Международный и отечественный опыт лечения ИВО у женщин неоднозначен. Выбор метода лечения зависит от этиологии состояния.Оперативное лече ние применяют у относительно небольшой группы пациенток. В случае анатомической/механической об струкции, связанной с пролапсом органов малого таза, выполняют оперативное пособие, направленное на ликвидацию опущения.
Ранние результаты баллонной дилатации уретры обнадеживали, однако в последующем долгосрочная эффективность метода не подтвердилась, а после 1994 года новых публикаций не было.При стенозе уретры или шейки мочевого пузыря может быть выполнена трансуретральная инцизия.
Оперативное лечение не потеряло своей значи мости у пациенток,которые не способны выполнять интермиттирующую катетеризацию или имеют посто янный катетер/цистостому. Устранение ИВО методом сфинктеротомии может быть достигнуто без полного разрушения удерживающей функции сфинктера. У части больных операцию приходится периодически повторять, так как вторично могут развиться сужение шейки мочевого пузыря и фиброз [40].
Стентирование уретры при ИВО у женщин при меняют в единичных случаях. Возможность их уста новки зависит от состоятельности шейки мочевого пузыря. Результаты применения уретральных стентов сопоставимы с таковыми при сфинктеротомии,но высокая стоимость, осложнения и необходимость по вторения процедуры являются ограничивающими факторами для этого метода [41].
Тренировка мышц тазового дна, как метод терапии первой линии
Методом лечения первой линии при дисфунк ции мочеиспускания у женщин является тренировка мышц тазового дна.Целесообразность тренировоч ной терапии обоснована патогенезом стрессового не держания мочи, связанным с дисфункцией мышц тазового дна. Тренировки, направленные на про извольное сокращение и расслабление тазовых мышц, позволяют повысить «управляемость» ими, что повы шает способность мышц к сокращению и является важным фактором удержания мочи. Тренировка на «расслабление» способствует релаксации сфинктер ного аппарата нижних мочевых путей при фИВО.
У женщин с недержанием мочи комплекс упраж нений,направленный на периодическое напряжение и расслабление мышц тазового дна (упражнения Ке геля, использование влагалищных конусов), способ ствует увеличению силы сокращений мышц диафрагмы таза и обеспечивает возможность более дли тельно удерживать мышцы в состоянии сокращения, что способствует функции удержания мочи. Метод используют при различных положениях тела – лежа, стоя, сидя, в зависимости от состояния пациента.
Имеется ряд исследований, подтверждающих положительное влияние тренировочных методов на состояние мочеиспускания у женщин с недержанием мочи.Однако информация об эффективности этого метода, по данным разных авторов, существенно раз личается – от 27% до 75% или даже до 90% при 12-не дельной тренировке,тогда как при использовании только поведенческой терапии и коррекции образа жизни улучшение состояния мочеиспускания от мечали только 7,2% пациенток [42, 43].
В систематическом обзоре S. Alouini и соавт., охватывающем 15 рандомизированных контролируемых исследований (997 пациенток), проанализирована и выявлена эффективность методов тренировки мышц тазового дна у женщин со стрессовым недержанием мочи. У 21,8% достигнута полая континенция по pad-тесту, а у 50,5% отмечено существенное улучшение [44].
В исследовании P. Rygh и соавт. на основании ре зультатов анкетирования 24602 женщин с недержа нием мочи было показано,что тренировка мышц та зового дна позволяет уменьшить выраженность симптомов по опроснику ISIQ-UI SF (International Conférence on Incontinence Questionnaire Short Form – Международное соглашение по вопроснику о недер жании мочи) в среднем на 1,31 балл, причем эффект был выше у пациенток с более выраженным недержа нием: при тяжелой степени регистрировали улучше ние на 3,23 балла, при средней тяжести – на 1,41 балл, а при легкой степени – на 0,24 балла. При оценке эф фективности тренировочной терапии по анкете PGI-I (Patient Global Imression of Improvement – Общее впечатление пациента об улучшении) улучшение со стояния отметили 65% женщин. В когорте пациенток в рандомизированном контролируемом исследовании подтверждена высокая эффективность: по опроснику ISIQ-UI SF сумма баллов уменьшилась на 3,9 пункта, а по анкете PGI-I улучшение удержания отметили 92% пациенток [45].
Имеются данные,что тренировка мышц тазо вого дна у женщин в период беременности и в раннем послеродовом периоде уменьшает риск развития не держания мочи, а у женщин с уже развившимся не держанием после родов тренировочные методы являются терапией первой линии.
Тренировочные методики также эффективны у женщин, занимающихся атлетическими видами спорта, у которых риск развития недержания мочи в 3 раза превышает риск в общей популяции, а также у физически активных женщин. Тренировки проводят как для профилактики развития недержания, так и в качестве лечебных мероприятий. Использование про граммы тренировок мышц тазового дна увеличивает силу мышечных сокращений и уменьшает объем те ряемой при нагрузке мочи, повышая качество жизни.
У женщин с недержанием мочи, обусловленным пролапсом тазовых органов,тренировочная терапия не только повышает степень удержания, но и умень шает выраженность пролапса, оцененного по системе РОР.
Для повышения эффективности тренировочной терапии разработаны специальные вспомогательные программы с использованием дополнительных ин структирующих устройств (Femiscan, Myself и др.). В исследовании S.S. Hoseini и соавт. показано, что тре нировка мышц тазового дна с использованием теле инструктора при выполнении упражнений Кегеля позволяет улучшить способность удерживать мочу даже у женщин старшего возраста, способствуя их со циальной адаптации [46].
В проспективном рандомизированном исследо вании, оценившем эффективность использования 4-недельной программы тренировок с дополнитель ным использованием устройств EmbaGYN (Велико британия) или Magic Kegel Master device (Китай) у 80
женщин с послеродовым недержанием мочи,проде монстрирована эффективность с уменьшением доли женщин с симптомами ургентного недержания с 35,3% до 8,8%, а со стрессовым недержанием – с 41,2% до 11,8% [47].
Многие авторы рекомендуют дополнять тренировки мышц тазового дна физиотерапевтическими методами. Показано, что использование электромагнитной стимуляции мышц тазового дна достоверно улучшает состояние женщин с недержанием мочи, оцененное методом анкетирования с использованием 8 опросников, характеризующих выраженность стрессового недержания мочи,пролапс тазовых органов, гиперактивность детрузора,ургентность и качество жизни без побочных эффектов [48].
Имеется ряд публикаций, свидетельствующих, что тренировка мышц тазового дна помогает не только повысить степень удержания, но и, наоборот, снизить повышенный тонус мышц,вызывающих затруднение мочеиспускания, что позволяет использовать этот метод для лечения женщин с дисфункциональным мочеиспусканием.
Вовлечение тазовых мышц в развитие дисфункционального мочеиспускания обусловило разработку специальных программ тренировок, направленных на снижение тонуса мышц тазового дна.
В проспективном исследовании, проведенном T. Lazaros и соавт., включающем 48 женщин с фИВО (Qmax < 12 мл/сек), оценили результаты тренировочной терапии, проводимой в течение 6 месяцев. Среднее значение максимальной скорости мочеиспускания увеличилось незначительно (с 7,5 до 8,5 мл/сек), объем остаточной мочи уменьшился с 110 до 65 мл. У 7 женщин параметры мочеиспускания нормализовались. Количество женщин с тяжелой степенью обструкции уменьшилось с 8 до 3, со средней степенью обструкции – с 16 до 8. Исходно 20 женщин отмечали 3 и более эпизодов мочевой инфекции в год, а 12 – эпизоды острой задержки мочи. После терапии эпизоды мочевой инфекции отмечены только у 4 пациенток, а случаев острой задержки мочи не было ни у кого [49].
Таким образом, тренировка мышц тазового дна оказывает существенный терапевтический эффект как при недержании мочи, так и при фИВО, хотя в последнем случае в литературе имеются ограниченные сведения.
Использование биологической обратной связи (БОС) как метода повышения эффективности тренировочной терапии при лечении женщин с нарушениями мочеиспускания
В большинстве исследований приводят данные о высокой эффективности тренировочной терапии у женщин с нарушенным мочеиспусканием,однако в ряде публикаций показано, что при самостоятельном применении 25-50% женщин не способны корректно управлять необходимыми мышцами,ошибочно на прягая мышцы антагонисты (ягодичные, мышцы бедра и передней брюшной стенки). Устные и пись менные инструкции не повышают результативность таких тренировок. Для повышения эффективности тренировочных программ у этих женщин необходимо сочетание обычных самостоятельных тренировок с аппаратными тренировочными технологиями с меди цинским контролем.
Для повышения эффективности тренировочных методов терапии все чаще используют тренировки, ос нованные на принципе БОС. Сущность БОС заключа ется в преобразовании биологических сигналов, получаемых от мышц с помощью электромиографии или датчиков давления, установленных во влагалище или на промежности, в аудио-, визуальные или вибра ционные сигналы, что позволяет пациентке контроли ровать тренировочный процесс.
Разработаны специальные устройства, обеспечи вающие функцию БОС и помогающие пациенткам контролировать степень напряжения тазовых мышц.
БОС постоянно информирует женщин о состоя нии их мышц, обеспечивая сознательный контроль их тонуса через обратную связь. Лучший контроль фи зиологического состояния мышц способствует фор мированию лучшего управления их тонусом, что улучшает результаты лечения.
В обзоре A.E. Matsi и соавт. проанализирована эффективность применения метода БОС при недер жании мочи разных форм (стрессовое, ургентное или смешанное), и показано статистически значимое улуч шение контроля мочеиспускания у женщин со стрес совым недержанием при использовании БОС по сравнению с другими вариантами тренировочной те рапии,тогда как при ургентном и смешанном недер жании эффективность БОС существенно ниже [50].
В обзоре F. Fitz и соавт. приведены данные о по вышении способности влиять на тонус мышц тазового дна при использовании технологии БОС по сравне нию с традиционными тренировками у женщин со стрессовым недержанием мочи [51].
В работе T.A. Ong и соавт. выявили достоверное повышение возможности напрягать мышцы тазового дна и более быстрое улучшение качества мочеиспускания после 4-недельного курса тренировочной терапии с использованием БОС, по сравнению с аналогичной терапией без БОС. Похожие результаты получены в исследовании M.M. Weinstein и соавт. Быстрое достижение результатов при использовании БОС объясняют более быстрой и более точной идентификацией пациенткой мышц, которые необходимо тренировать, что позволяет целенаправленно влиять на сокращение мышц. Таким образом, БОС может ускорить повыше ние мышечного тонуса и нейромышечного взаимодействия, способствуя повышению функции удержания мочи. Кроме того, более ранее улучшение степени континенции повышает мотивацию пациен ток к продолжению терапии. К таким же выводам приходят F. Goulart и соавт., считающие, что исполь зование БОС улучшает произвольную функцию мышц, усиливает нейропластичность или активирует механизм формирования новых нейронных связей в центральной нервной системе,за счет создания для нее новых потребностей.Процесс нейропластично сти позволяет пациенткам постоянно контролировать мышечную активность и управлять ею, давая возможность обеспечивать функцию удержа ния мочи [52-54].
Помимо более быстрого увеличения силы сокра щений, использование принципа БОС позволяет уве личить способность удерживать напряжение тазовых мышц в течение определенного времени,что также повышает возможность удерживать мочу, в том числе при смешанной форме недержания.
В исследовании S. Firinci и соавт. сравнили эф фективность тренировочной терапии у женщин с идиопатической гиперактивностью мочевого пузыря и недержанием мочи в сравнении с терапий,допол ненной БОС, электростимуляцией или БОС+электро стимуляцией. Было показано преимущество комбинированной терапии в группе тренировки+БОС+ электростимуляция, хотя определенное улучшение состояния функции мочеиспускания отмечено во всех группах пациенток. Уменьшались частота моче испусканий, частота эпизодов недержания, выражен ность ноктурии, повышалась оценка качества жизни [55, 56].
В Национальных рекомендациях Великобрита нии указано,что использование БОС при трениров ках мышц тазового дна в бóльшей степени способствует улучшению качества жизни пациенток, чем применение только тренировочной терапии [57].
Об удовлетворенности результатами лечения с использованием БОС как дополнения к тренировоч ной терапии свидетельствуют данные о том, что около 60% женщин не прибегают к другим методам лечения и, при необходимости, проходят повторные курсы тренировок [58].
На результаты лечения могут влиять субъектив ные факторы восприятия пациентками процесса те рапии. В частности, использование поверхностных миографических датчиков для осуществления БОС более предпочтительно, чем использование вагиналь ных датчиков, поскольку при их применении нередко отмечалось жжение во влагалище, болезненное моче испускание, раздражение кожи вблизи влагалища. Преимуществом поверхностных электродов является наличие облегченных высокочувствительных моде лей, надежно фиксируемых на теле пациентки, что позволяет проводить исследование в различных по ложениях тела и более точно оценивать динамику ле чебного процесса.
Важным вопросом является длительность сохра нения эффекта тренировок в отношении способности удерживать мочу. По данным M. Gameiro и соавт., эф фект тренировки сохранялся в течение 6 месяцев, но постепенно исчезал к 12 месяцам. По другим данным, уменьшение степени удержания сохранялось в тече ние 1 года у 70-74% пациенток [59].
В отношении оценки эффективности БОС при терапии дисфункционального мочеиспускания име ется существенно меньше публикаций.
C.H. Chiang и соавт. оценили клиническую эф фективность БОС в составе тренировочной терапии у женщин с фИВО и установили, что через 3 месяца улучшение качества мочеиспускания и, соответ ственно, качества жизни отметили более 80% женщин [60].
О более высокой эффективности использования БОС в программе тренировок мышц тазового дна у женщин с фИВО,по сравнению с традиционной тре нировочной терапией, сообщается в публикации E. Sam и соавт. При использовании БОС как компо нента тренировочной терапии,достигали значитель ного увеличения максимальной и средней скоростей мочеиспускания, а также значительного уменьше ния объема остаточной мочи, по сравнению с груп пой, где использовались только тренировки. Также в группе с использованием БОС, выраженность симп томов, оцененная по шкале UDI-6 (Urinary Distress In ventory-6 – Шкала оценки расстройств мочеиспускания), оказалась достоверно ниже. Электромиографи ческая активность мышц тазового дна также умень шалась в большей степени в группе женщин при использовании метода БОС [61].
Таким образом, суммируя вышеизложенные дан ные, можно сделать заключение, что применение ме тода БОС повышает эффективность тренировочной терапии стрессового недержания мочи,но в отноше нии ургентного или смешанного вариантов недержа ния данные неоднозначны. Технология БОС также позволяет улучшить результаты лечения пациенток с дисфункциональным мочеиспусканием.
ЗАКЛЮЧЕНИЕ
Проблема лечения женщин с различными функциональными нарушениями является актуальной.Из методов консервативного лечения наиболее часто используют тренировку мышц тазового дна в различных модификациях (самостоятельные тренировки, дополнительное использование теле- или аудио-инструктирую-щих устройств), считающуюся методом терапии первой линии. Тренировка мышц тазового дна позволяет уве- личить силу их сокращений и возможность более дли тельно удерживать мышцы в сокращенном состоянии, что способствует улучшению функции удержания мочи. При этом, не все исследователи находили прямую связь между увеличением мышечного тонуса и улучшением функции нижних мочевыводящих путей, придавая значение психологической составляющей тренировоч ного процесса.Дополнительное использование метода биологической обратной связи (БОС) позволяет лучше контролировать процесс тренировки и достижения не обходимой степени сокращения или расслабления, осо бенно для тех женщин, у которых самостоятельное управление необходимыми мышцами вызывает трудно сти. Во многих публикациях приводятся данные о боль шей эффективности включения БОС в схему трени ровок,тогда как в других сообщениях авторы не вы являли различий между группами женщин с трениров ками, дополненными БОС или изолированными тренировками. Однако,в части из них оценка проводилась только на основании изменения тонуса тазовых мышц. В отношении тренировочных методов,в том числе с использованием БОС,у женщин с функциональной ИВО данные литературы крайне ограничены, хотя в имеющихся публикациях отмечается положительный эффект включения БОС в схему тренировок.
БОС терапия относится к высокотехнологичным методам лечения, совершенствуется аппаратное сопровождение, в том числе по программе импортозамещения, что открывает широкие перспективы его использования и обеспечения большей доступности в различных звеньях оказания медицинской помощи (поликлиники, женские консультации, санатории, реабилитационные центры).
Список литературы Недержание мочи и инфравезикальная обструкция: Сцилла и Харибда женской урологии. Роль методов биологической обратной связи
- Abdel Raheem A, Madersbacher H. Voiding dysfunction in women: How to manage it correctly. Arab J Urol 2013;11(4):319-30. https://doi.org/10.1016/j.aju.2013.07.005.
- Gormley EA, Lightner DJ, Faraday M, Vasavada SP. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. J Urol 2015;193(5):1572-80. https://doi.org/10.1016/j.juro.2015.01.087.
- García-Sánchez E, Rubio-Arias JA, Ávila-Gandía V, Ramos-Campo DJ, López-Román. Effectiveness of pelvic floor muscle training in treating urinary incontinence in women: A current review. J Actas Urol Esp 2016;40(5):271-8. https://doi.org/10.1016/j.acuro.2015.09.001.
- Сивков А.В., Ромих В.В. Инфравезикальная обструкция у женщин. Урология 2006;(5):90-4. [Sivkov A.V., Romikh V.V. Infravesical obstruction in women. Urologiya = Urologiia 2006;(5):90-4. (In Russian)].
- Ермакова Е.И., Балан В.Е., Краснопольская И.В., Тихомирова Е.В. Консервативная терапия недержания мочи у женщин. Российский вестник акушера-гинеколога 2014;(4):113-5. [Ermakova E.I.,Balan V.E., Krasnopol'skaia I.V., Tikhomirova E.V. Medical therapy for female urinary incontinence. Rossiyskiy vestnik akushera-ginekologa = Russian Bulletin of Obstetrician-Gynecologis 2014;(4):113-5. (In Russian)].
- Weber-Rajek M, Strączyńska A, Strojek K, Piekorz Z, Pilarska B, Podhorecka M, et al. A. Assessment of the Effectiveness of Pelvic Floor Muscle Training (PFMT) and Extracorporeal Magnetic Innervation (ExMI) in treatment of stress urinary incontinence in women: A randomized controlled trial. BioMed Res Int 2020;2020:1019872. https://doi.org/10.1155/2020/1019872.
- Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric 2019;22(3):217-22. https://doi.org/10.1080/13697137.2018.1543263
- Ромих В.В. Клиническая уродинамика и нейроурология: от диагностики к эффективному лечению и реабилитации. Экспериментальная и клиническая урология 2010(4):92-8. [Romih V.V. Clinical urodynamics and neurourology: from diagnosis to effective treatment and rehabilitation. Eksperimentalnaya i Klinicheskaya Urologiya = Experimental and Clinical Urology 2010(4):92-8. (In Russian)].
- Серегин А.В., Синякова Л.А., Довлатов З.А., Матвеевская Т.А. Недержание мочи: возможности консервативной терапии. Проблемы женского здоровья 2010;5(1):74-6. [Seryogin A.V., Sinyakova L.A., Dovlatov Z.A., Matveyevskaya T.A. Urinary incontinence: opportunities of conservative treatment. Problemy zhenskogo zdorov'ya = Women's Health Issues 2010;5(1):74-6. (In Russian)].
- Caruso S, Brescia R, Matarazzo MG, Giunta G, Rapisarda AMC, Cianci A. Effects of urinary incontinence subtypes on women's sexual function and quality of life. Urology 2017;108:59-64. https://doi.org/10.1016/j.urology.2017.06.025.
- Sjöström M, Umefjord G, Stenlund H, Carlbring P, Andersson G, Samuelsson E. Internet-based treatment of stress urinary incontinence: 1and 2-year results of a randomized controlled trial with a focus on pelvic floor muscle training. BJU Int 2015;116(6):955-64. https://doi.org/10.1111/bju.13091.
- Harding CK, Lapitan MC, Arlandis S, Cobussen-Boekhorst, E. Costantini, J. Groen, et. al. Management of non-neurogenic female lower urinary tract symptoms. EAU Guidelines 2022:148.
- Flisser AJ, Blaivas JG. Using urodynamics to diagnose bladder outlet obstruction in women. Contemporary Urology 2002:223-5.
- Mytilekas KV, Oeconomou A, Sokolakis I, Kalaitzi M, Mouzakitis G, Nakopoulou E, et al. Defining voiding dysfunction in women: bladder outflow obstruction versus detrusor underactivity. Int Neurourol J 2021;25(3):244-51. https://doi.org/10.5213/inj.2040342.171.
- Agarwal MM, Sharma S, Jain S, Prasad D, Bhaskar V, Gupta S, et al. Can urodynamic diagnosis of dysfunctional voiding/external sphincter nonrelaxation be made on two-channel pressure-flow study without video-urodynamics, electromyography, or urethral pressure profilometry? Plateau detrusor pattern in perspective. Neurourol Urodyn 2022;41(4):935-44. https://doi.org/10.1002/nau.24897.
- Terlikowski R, Dobrzycka B, Kinalski M, Kuryliszyn-Moskal A, Terlikowski SJ. Transvaginal electrical stimulation with surface-EMG biofeedback in managing stress urinary incontinence in women of premenopausal age: a double-blind, placebo-controlled, randomized clinical trial. Int Urogynecol J 2013;24(10):1631-8. https://doi.org/10.1007/s00192-013-2071-5.
- Brucker BM, Fong E, Shah S, Kelly C, Rosenblum N, Nitti VW. Urodynamic differences between dysfunctional voiding and primary bladder neck obstruction in women. Urology 2012;80(1):55-60. https://doi.org/10.1016/j.urology.2012.04.011.
- Hickling D, Aponte M, Nitti V. Evaluation and management of outlet obstruction in women without anatomical abnormalities on physical exam or cystoscopy. Curr Urol Rep 2012t;13(5):356-62. https://doi.org/10.1007/s11934-012-0267-8.
- Vo A, Kielb SJ. Female voiding dysfunction and urinary incontinence. Med Clin North Am 2018;102(2):313-24. https://doi.org/10.1016/j.mcna.2017.10.006.
- Imamura M, Jenkinson D, Wallace S, Buckley B, Vale L, Pickard R. Conservative treatment options for women with stress urinary incontinence: clinical update. Br J Gen Pract 2013;63(609):218-20. https://doi.org/10.3399/bjgp13X665477.
- van Geen FJ, van de Wetering EHM, Nieuwhof-Leppink AJ, Klijn AJ, de Kort LMO. Dysfunctional voiding: exploring disease transition from childhood to adulthood. Urology 2023;177:60-4. https://doi.org/10.1016/j.urology.2023.03.018.
- Petros PE. The pelvic floor muscle training manoeuvre works by increasing intraurethral resistance. Comment on «Influence of voluntary pelvic floor muscle contraction and pelvic floor muscle training on urethral closure pressures: a systematic literature review». Int Urogynecol J 2016;27(12):1943-4. https://doi.org/10.1007/s00192-016-3182-6.
- Petros PE, Ulmsten U. An integral theory of female urinary incontinence. Acta Obstet Gynecol Scand Suppl 1990;153:7-31. https://doi.org/10.1111/j.1600-0412.1990.tb08027.x.
- Касян Г.Р., Вишневский Д.А., Акуленко Л.В., Козлова Ю.О., Шарова Е.И., Тупикина Н.В., Пушкарь Д.Ю. Ассоциация полиморфизма 1800255 гена СОL3A1 с развитием пролапса тазовых органов и недержания мочи у женщин: предварительные данные. Урология 2017;(6):30-3. [Kasyan G.R., Vishnevskii D.A., Akulenko L.V., Kozlova Yu.O., Sharova E.I., Tupikina N.V., Pushkar D.Yu. association of polymorphism of 1800255 COL3A1. Urologiya = Urologiia 2017;(6):30-3. (In Russian)]. https://doi.org/10.18565/urology.2017.6.30-33.
- Cacciari LP, Amorim AC, Pyssaro AC, Dumoulin C, Sacco ICN. Intravaginal pressure profile of continent and incontinent women. J Biomech 2020;99:10972. https://doi.org/10.1016/j.jbiomech.2019.10972.
- Deindl FM, Vodusek DB, Bischoff C, Hofmann R, Hartung R. Dysfunctional voiding in women: which muscles are responsible? Br J Urol 1998;2(6):814-9. https://doi.org/10.1046/j.1464-410x.1998.00866.x.
- Groutz A, Blaivas JG, Pies C, Sassone AM. Learned voiding dysfunction (nonneurogenic, neurogenic bladder) among adults. Neurourol Urodyn 2001;20(3):259-68. https://doi.org/10.1002/nau.1003.
- Panicker JN, Selai C, Herve F, Rademakers K, Dmochowski R, Tarcan T, et al. Psychological comorbidities and functional neurological disorders in women with idiopathic urinary retention: International Consultation on Incontinence Research Society (ICI-RS) 2019. Neurourol Urodyn 2020;39(Suppl 3):S60-S69. https://doi.org/10.1002/nau.24233.
- Peyronnet B, Lapitan MC, Tzelves L, O'Connor E, Nic An Riogh A, et al. Benefits and harms of conservative, pharmacological, and surgical management options for women with bladder outlet obstruction: A systematic review from the European Association of Urology Non-neurogenic Female LUTS Guidelines Panel. Eur Urol Focus 2022;8(5):1340-61. https://doi.org/10.1016/j.euf.2021.10.006.
- Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev 2012;10(10):CD001405. https://doi.org/10.1002/14651858.CD001405.pub3.
- Minardi D, Pellegrinelli F, Conti A, Fontana D, Mattia M, Milanese G, et al. α1Blockers for the treatment of recurrent urinary tract infections in women with dysfunctional voiding: a prospective randomized study. Int J Urol 2015;22(1):115-21. https://doi.org/10.1111/iju.12601.
- Ромих В.В., Захарченко А.В., Коршунова Е.С., Кукушкина Л.Ю. Использование ботулинического токсина тина А у пациентов с нейрогенными нарушениями мочеиспускания. Экспериментальная и клиническая урология 2010;(1):81-4. [Romikh V.V., Zaharchenko A.V., Korshunova E.S., Kukushkina L.U. Using of botulinum a toxin in treatment of neurogenic voiding desorders patients. Eksperimentalnaya i Klinicheskaya urologiya = Experimental and Clinical Urology 2010;(1):81-4. (In Russian)].
- Sokol ER, Karram MM, Dmochowski R. Efficacy and safety of polyacrylamide hydrogel for the treatment of female stress incontinence: a randomized, prospective, multicenter North American study. J Urol 2014;192(3):843-9. https://doi.org/10.1016/j.juro.2014.03.109.
- Jiang YH, Lee CL, Chen SF, Kuo HC. Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women. Toxins (Basel) 2021;13(5):362. https://doi.org/10.3390/toxins13050362.
- Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 2017;7(7):CD006375. https://doi.org/10.1002/14651858.CD006375.pub4.
- Колотева Е.В., Чаркина О.В., Шилина А.В., Бельских О.Л. Результат использования TVT-петли при пролапсе тазовых органов, осложненном недержанием мочи. Молодежный инновационный вестник 2018;7(S1):109. [Koloteva E.V., Charkina O.V., Shilina A.V., Belskikh O.L. The result of using TVT-loop in pelvic organ prolapse complicated by urinary incontinence. Molodozhnyy innovatsionnyy vestnik 2018;7(S1):109. (In Russian)].
- Gurol-Urganci I, Geary RS, Mamza JB, Duckett J, El-Hamamsy D, Dolan L, et al. Long-term rate of mesh sling removal following midurethral mesh sling insertion among women with stress urinary incontinence. JAMA 2018;320(16):1659-69. https://doi.org/10.1001/jama.2018.14997.
- Fusco F, Abdel-Fattah M, Chapple CR, Creta M, La Falce S, Waltregny D, et al. Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Eur Urol 2017;72(4):567-91. https://doi.org/10.1016/j.eururo.2017.04.026.
- Giarenis I, Mastoroudes H, Cardozo L, Robinson D. Rediscovery of open colposuspension as a salvage continence operation. Int Urogynecol J 2012;23(8):1117-22. https://doi.org/10.1007/s00192-012-1720-4.
- Utomo E, Groen J, Blok BF. Surgical management of functional bladder outlet obstruction in adults with neurogenic bladder dysfunction. Cochrane Database Syst Rev 2014;2014(5):CD004927. https://doi.org/10.1002/14651858.CD004927.pub4.
- Brasure M, Fink HA, Risk M, MacDonald R, Shamliyan T, Ouellette J, et al. Chronic urinary retention: Comparative effectiveness and harms of treatments. Rockville (MD): AHRQ (US) 2014.
- Leong BS, Mok NW. Effectiveness of a new standardized urinary continence physiotherapy program for community-dwelling older women in Hong Kong. Hong Kong Med J 2015;21(1):30-7. https://doi.org/10.12809/hkmj134185.
- Curillo-Aguirre CA, Gea-Izquierdo E. Effectiveness of pelvic floor muscle training on quality of life in women with urinary incontinence: A systematic review and meta-analysis. Medicina (Kaunas) 2023;59(6):1004. https://doi.org/10.3390/medicina59061004.
- Alouini S, Memic S, Couillandre A. Pelvic floor muscle training for urinary incontinence with or without biofeedback or electrostimulation in women: A systematic review. Int J Environ Res Public Health 2022;19(5):2789. https://doi.org/10.3390/ijerph19052789.
- Rygh P, Asklund I, Samuelson E. Real-world effectiveness of app-based treatement for urinary incontinence: a cohort study. BMJ Open 2021;11(1):e040819. https://doi.org/10.1136/bmjopen-2020-040819.
- Hoseini SS, Ghahremani L, Khorasani F, Yarelahi M, Asadollahi A. Training of pelvic floor muscle training improves the severity and quality of urine incontinence and increases social participation of older women in Southern Iran. Curr Aging Sci 2024;17(1):68-73. https://doi.org/10.2174/1874609816666230816125026.
- Artymuk NV, Khapacheva SY. Device-assisted pelvic floor muscle postpartum exercise programme for the management of pelvic floor dysfunction after delivery. J Matern Fetal Neonatal Med 2022;35(3):481-5. https://doi.org/10.1080/14767058.2020.1723541.
- Борисенко Л.Ю., Сивков А.В., Ромих В.В., Захарченко А.В., Пантелеев В.В., Костин А.А., Аполихин О.И. Результаты исследования метода биологической обратной связи с тестовой электростимуляцией мышц тазового дна в качестве монотерапии и в сочетании с экстракорпоральной магнитной стимуляцией мышц тазового дна при функциональной инфравезикальной обструкции у женщин. Экспериментальная и клиническая урология 2019;(2):146-51. [Borisenko L.Yu., Sivkov A.V., Romikh V.V., Zakharchenko A.V., Panteleyev V.V., Kostin A.A., Apolikhin O.I. The results of the comparative study of biofeedback with test electrostimulation of the pelvic floor muscles as monotherapy and in combination with extracorporeal magnetic stimulation of the pelvic floor muscles with functional infravesical obstruction in women. Eksperimentalnaya i Klinicheskaya Urologiya = Experimental and Clinical Urology 2019;(2):146-51. (In Russian)].
- Lazaros T, Ioannis T, Vasileios S, Christina P, Michae S. The effect of pelvic floor muscle training in women with functional bladder outlet obstruction. Arch Gynecol Obstet 2023;307(5):1489-94. https://doi.org/10.1007/s00404-023-06930-z.
- Matsi AE, Billis E, Lampropoulou S, Xergia SA, Tsekoura M, Fousekis K. The effectiveness of pelvic floor muscle exercise with biofeedback in women with urinary incontinence: A systematic review. Appl Sci 2023;23:12743. https://doi.org/10.3390/app132312743.
- Fitz FF, Resende AP, Stüpp L, Costa TF, Sartori MG, Girão MJ, et al. Effect the adding of biofeedback to the training of the pelvic floor muscles to treatment of stress urinary incontinence. Rev Bras Ginecol Obstet 2012;34(11):505-10. https://doi.org/10.1590/s0100-72032012001100005.
- Ong TA, Khong SY, Ng KL, Ting JR, Kamal N, Yeoh WS, et al. Using the Vibrance Kegel Device with pelvic floor muscle exercise for stress urinary incontinence: A randomized controlled pilot study. Urology 2015;86(3):487-91. https://doi.org/10.1016/j.urology.2015.06.022.
- Weinstein MM, Collins S, Quiroz L, Anger JT, Paraiso MFR, DeLong J, et al. Multicenter randomized controlled trial of pelvic floor muscle training with a motionbased digital therapeutic device versus pelvic floor muscle training alone for treatment of stress-predominant urinary incontinence. Female Pelvic Med Reconstr Surg 2022;28(1):1-6. https://doi.org/10.1097/SPV.0000000000001052.
- Goulart F, Vasconcelos KS, de Souza MR, Pontes PB. Physical therapy for facial paralysis using the biofeedback. Acta Fisiátr 2002(9):134-40.
- Firinci S, Yildiz N, Alkan H, Aybek Z. Which combination is most effective in women with idiopathic overactive bladder, including bladder training, biofeedback, and electrical stimulation? A prospective randomized controlled trial. Neurourol Urodyn 2020;39(8):2498-508. https://doi.org/10.1002/nau.24522.
- Özengin N, Bakar Y, Özdemir C, Duran B. The comparison of EMGbiofeedback and extracorporeal magnetic innervation treatments in women with urinary incontinence. Clin Exp Obstet Gynecol 2016;43(4):550-4.
- National Guideline Alliance UK. Urinary Incontinence and Pelvic Organ Prolapse in Women: Management 2019. [Electronic resource]. URL: www.nice.ork.uk/guidance/ng123.
- Yoo EH, Kim YM, Kim D. Factors predicting the response to biofeedback-assisted pelvic floor muscle training for urinary incontinence. Int J Gynaecol Obstet 2011;112(3):179-81. https://doi.org/10.1016/j.ijgo.2010.09.016.
- Sigurdardottir T, Steingrimsdottir T, Geirsson RT, Halldorsson TI, Aspelund T, Bø K. Can postpartum pelvic floor muscle training reduce urinary and anal incontinence? An assessor-blinded randomized controlled trial. Am J Obstet Gynecol 2020;222(3):247.e1-247.e8. https://doi.org/10.1016/j.ajog.2019.09.011.
- Chiang CH, Jiang YH, Kuo HC. Therapeutic efficacy of biofeedback pelvic floor muscle exercise in women with dysfunctional voiding. Sci Rep 2021;11(1):13757. https://doi.org/10.1038/s41598-021-93283-9.
- Hagen S, Elders A, Stratton S, Sergenson N, Bugge C, Dean S, et al. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: Multicentre randomised controlled trial. BMJ 2020;371:m3719. https://doi.org/10.1136/bmj.m3719.