Нейропсихиатрические последствия COVID-19
Автор: Петрова Н.Н.
Журнал: Juvenis scientia @jscientia
Рубрика: Обзорные статьи
Статья в выпуске: 4 т.8, 2022 года.
Бесплатный доступ
Обзор литературы посвящен постковидным нейропсихиатрическим расстройствам. В статье раскрывается понятие постковидного синдрома, приводятся определения NICE и ВОЗ, дается характеристика клинической картины с системным поражением организма. Приводятся данные о росте психиатрической заболеваемости в различные сроки после перенесенной коронавирусной инфекции, включая депрессию, тревогу, когнитивные нарушения, астению. В качестве основной характеристики постковидного синдрома описан астеноневротический симптомокомплекс с выраженной астенией и когнитивной дисфункцией, к которому нередко присоединяется затяжная тревожно-депрессивная симптоматика. Когнитивные нарушения в рамках постковидного синдрома представлены преимущественно нарушениями памяти, снижением способности к концентрации внимания, ухудшением исполнительских функций независимо от возраста и предшествующего когнитивного снижения. Отмечено, что делирий в остром периоде коронавирусной инфекции является значимым фактором риска развития когнитивных нарушений в постковидном периоде. Описываются предполагаемые механизмы и факторы риска нейропсихиатрических последствий COVID-19, при этом подчеркивается значение системного воспаления, как ведущего патогенетического механизма постковидных психических расстройств.
Covid-19, постковидный синдром, нейропсихиатрические расстройства, астения, депрессия, тревога, когнитивные нарушения, механизмы развития
Короткий адрес: https://sciup.org/14126339
IDR: 14126339 | DOI: 10.32415/jscientia_2022_8_4_5-14
Текст обзорной статьи Нейропсихиатрические последствия COVID-19
This article is licensed under a Creative Commons Attribution 4.0 International License.
ПОНЯТИЕ ПОСТКОВИДНОГО СИНДРОМА
Значительное число лиц (10-30 % или даже более), перенесших новую коронавирусную инфекцию, вызванную SARS-CoV-2, продолжают испытывать симптомы, связанные с COVID-19, после острой фазы заболевания [1].
Такое постковидное состояние обозначается термином «постковидный синдром» или «long-COVID» — «длинный» или затяжной ко-вид. Есть мнение, что более корректным является термин «постковидный синдром» или post-acute COVID-19 syndrome, т. к. термин «затяжной COVID-19» может создавать ложное представление о хронической вирусной инфекции как основе постковидных нарушений [2]. Согласно определению NICE (National Institute for Health and Care Excellence), под пост-COVID-19-синдромом понимают признаки и симптомы, которые развиваются во время или после COVID-19, продолжаются более 12 недель и не объясняются альтернативным диагнозом. Термин «длительный COVID» или «длинный COVID» обычно используется для описания признаков и симптомов, которые продолжаются или развиваются после острого COVID-19. Сюда входят как текущие симптомы COVID-19 (от 4 до 12 недель), так и пост-COVID-19-синдром (12 недель и более) [3]. В октябре 2021 года ВОЗ дала определение термина: «Постковидный синдром возникает у лиц после коронавирусной инфекции с подтвержденным заражением SARS-CoV-2, либо у лиц с подозрением на коронавирусную инфекцию, обычно через 3 месяца после начала COVID-19, с симптомами, которые длятся не менее 2 месяцев и не могут быть объяснены альтернативным диагнозом» [4].
СТРУКТУРА ПОСТКОВИДНОГО СИНДРОМА: ФОКУС НА НЕЙРОПСИХИАТРИЧЕСКИЕ НАРУШЕНИЯ
«Постковидный синдром» может затрагивать дыхательную, сердечно-сосудистую, иммунную системы организма. Метаанализ 15 исследований из разных стран, включав- ших 440 800 пациентов в возрасте от 17 до 87 лет показал, что не менее 80 % пациентов не чувствуют себя полностью выздоровевшими, а у некоторых симптомы коронавирусной инфекции не только сохраняются, но и усиливаются спустя месяцы после COVID-19. Авторы выделили 55 симптомов, с которыми миллионы людей борются длительное время после заболевания, среди которых наиболее часто встречаются: сильная утомляемость (58 %), головная боль (44 %), нарушение концентрации внимания и памяти (25 %), потливость, депрессия, тревожность и навязчивости [5]. Часто наблюдаются усталость, одышка, нарушения со стороны сердечно-сосудистой системы, нарушения сна, симптомы посттравматического стрессового расстройства (ПТСР), боль в суставах и мышцах, потеря вкуса или обоняния, выпадение волос. Несколько реже встречаются кожная сыпь, снижение аппетита, нарушения функций легких, почек [6, 7].
Согласно метаанализу, утомляемость и диспноэ часто встречаются у пациентов, как госпитализированных, так и не госпитализированных, спустя 60 и 90 дней после COVID-19: 56 % и 35 % для усталости: 27 % и 26 % для диспноэ, соответственно. Европейские показатели распространенности усталости и диспноэ существенно выше, чем в Китае, что, возможно, связано с более молодым возрастом и меньшей коморбидностью у китайских пациентов [8].
Развитие психических нарушений встречается в 2 раза чаще по сравнению с гриппом или другими острыми респираторными инфекциями, причем психиатрическая заболеваемость возрастает в течение 6 месяцев после заражения COVID-19, независимо от ее тяжести [9]. По сравнению с другими острыми респираторными инфекциями вирус SARS-CoV-2 обладает явно большей нейротропной активностью и значительно чаще вызывает поражение ЦНС, в связи с чем большое внимание уделяется поражению нервной системы в виде неврологической и/или психопатологической симптоматики
[10]. Несмотря на соответствие клиническим критериям выздоровления, у пациентов обнаруживаются проблемы с психическим здоровьем, как основные последствия COVID-19 [11]. Спустя 6 месяцев после COVID-19 13 % от 236 тысяч пациентов был установлен психиатрический или неврологический диагноз [12]. Пациенты подвержены риску возникновения психических расстройств спустя 30 и более дней после получения положительного теста на SARS-CoV-2, включая тревожные и депрессивные расстройства, расстройства адаптации, употребление психоактивных веществ, нейро-когнитивные нарушения и расстройства сна [13]. Более половины пациентов сообщают хотя бы об одном из психопатологических симптомов (тревоге, депрессии, ПТСР или когнитивных нарушениях) через 6 месяцев после заболевания [14].
Распространенность тревоги, депрессии и нарушений сна у перенесших COVID-19 пациентов составляет 47 %, 45 % и 34 %, соответственно [8]. Частота симптомов депрессии спустя 12 недель от острого состояния составляет 11-28 %, в то время как частота проявления клинической депрессии 3-12 % [15]. Расстройства настроения спустя 6 месяцев после острого COVID-19 встречаются заметно чаще, чем после гриппа или другой ОРВИ в те же промежутки времени [16].
Систематический анализ исследований, посвященных изучению различных психических нарушений в рамках постковидного синдрома продолжительностью от 2 недель до 10 месяцев, т. е. в соответствии с определениями МКБ-10 и NICE в течение всего постковидного периода (более 4 недель от начала заболевания при условии отрицательного теста полимеразной цепной реакции — ПЦР), установил в качестве характеристики длительно текущего мультисистемного пост-ковидного синдрома особый астеноневро-тический симптомокомплекс с выраженной астенией и когнитивной дисфункцией (нарушения памяти, внимания, исполнительских функций), к которому нередко присоединя- ются затяжная тревожно-депрессивная симптоматика и ПТСР. Этот психопатологический симптомокомплекс выявляется почти у трети всех заболевших и у двух третей пациентов с тяжелым течением коронавирусной инфекции и госпитализацией [17].
Когнитивные нарушения в рамках пост-ковидного синдрома представлены преимущественно нарушениями памяти и внимания независимо от возраста [18]. 18 % пациентов, перенесших COVID-19, имеют новые или усилившиеся проблемы с памятью и 16 % — с концентрацией внимания [7]. Онлайн-опрос в США выявил более 50 % когнитивных нарушений после COVID-19, особенно долго сохранялись трудности концентрации внимания [19]. 28-56 % пациентов с нетяжелым или бессимптомным течением COVID-19 обнаружили постковидные когнитивные нарушения, преимущественно в виде нарушения внимания и исполнительных функций (планирование, целеполагание, решение задач) [20]. Жалобы включают трудности с концентрацией внимания, формулировкой мыслей, принятием решений («мозговой туман»). Отмечена корреляция когнитивного дефицита и тяжести заболевания (рис. 1). Есть данные, что COVID-19 ухудшает понимание текста и смысла слов (гнозис) [21]. Делирий в остром периоде коронавирусной инфекции выступает значимым фактором риска развития постковидных когнитивных нарушений [22].
ВОЗМОЖНЫЕ МЕХАНИЗМЫ РАЗВИТИЯ ПОСТКОВИДНЫХ НЕЙРОПСИХИАТРИЧЕСКИХ НАРУШЕНИЙ
Постковидный синдром расценивают как осложнение COVID-19, связанное с непосредственным вирусным поражением ЦНС и с системными нарушениями (прежде всего, сердечно-сосудистыми и дыхательными), а также со стрессовыми факторами [23, 24]. Инфекция, вызванная SARS-CoV-2, является системным заболеванием, поэтому патогенез психопатологической симптоматики, по-видимому, носит мультифакторный харак-
Без Респираторные Респираторные Лечение Лечение
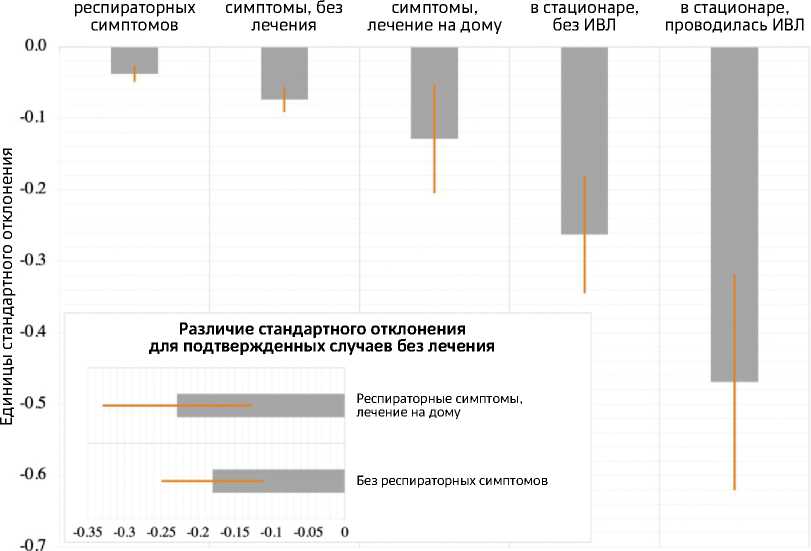
Рисунок 1. Когнитивный дефицит среди разных групп пациентов, перенесших COVID-19 (перевод автора) [21]
тер. Коронавирусы способны индуцировать психопатологические осложнения через прямое воздействие на ЦНС или опосредованно, путем иммунного ответа [25]. Клинические, посмертные, биологические, in vitro, исследования, а также исследования культуры клеток, продемонстрировали потенциальную нейротропность и способность коронавирусов вызывать нейрональные повреждения [26]. «Цитокиновый шторм» может привести к психиатрической симптоматике через процесс нейровоспаления [27-30]. Вероятность возникновения нейропсихиатрических осложнений в постковидном периоде ассоциирована с повышенным индексом системного иммунного воспаления. Среди молекул воспаления выделяются ФНО-альфа, ИЛ-6, ИЛ-1 бета, интерферон-гамма, гранулоцитарномакрофагальный колониестимулирующий фактор. Тучные клетки активируются и также поддерживают воспаление за счет гистамина, цитокинов и хемокинов [31]. Повышенные уровни провоспалительных цитокинов способствуют их проникновению через гематоэнцефалический барьер и активации астроцитов и микроглии. Клетки микроглии и астроциты начинают синтезировать ИЛ-1 бета, рецепторы к которому распространены в зоне гиппокампа [32]. Активация клеток глии и астроцитов влияет на обмен нейротрансмиттеров, факторы роста, участвующие в процессе дифференцировки и выживания нейронов.
Стигматизация в связи с коронавирусной инфекцией, травматические воспоминания пережитого заболевания, социальная изоляция, ухудшение материального благосостояния являются мощными психологическими триггерами, которые оказывают влияние на развитие психических расстройств и определяют психопатологический исход [33, 34]. Имеются данные, что пациенты с коморбид-ными заболеваниями и иммуносупрессией более подвержены развитию когнитивных нарушений, тревоги и депрессии [35]. Респираторные симптомы COVID-19 могут обусловить развитие панического расстройства [36]. Развитие аффективных расстройств в постковид-ном периоде частично объясняется системным воспалением вследствие COVID-19, когда реакция гипервоспаления в острой фазе продолжается в персистирующее хроническое воспаление, являющееся патогенетическим механизмом расстройств настроения [37]. Среди ведущих факторов, ассоциированных с депрессией, также выделяют женский пол, предшествующий психиатрический анамнез. Выявлена обратная корреляция между выраженностью депрессивной симптоматики и продолжительностью госпитализации пациентов [38]. Серопозитивность по коронавирусу ассоциирована с суицидальным поведением в течение года после острого заболевания [39]. Дисбаланс центральных нейротрансмиттеров (норадреналина, эпинефрина, серотонина) также может влиять на развитие пост-ковидных аффективных расстройств [40].
Женщины и пациенты с имевшимся диагнозом депрессии или тревожного расстройства имеют больший риск развития усталости [41]. Вероятной физической основой для усталости в постковидном периоде может выступать эндотелиальная дисфункция в капиллярах головного мозга [42]. Выраженность астенического синдрома не коррелирует с тяжестью перенесенного заболевания, однако значительно выше у пациентов, прошедших через отделение реанимации и интенсивной терапии [22].
Развитие когнитивных нарушений на фоне COVID-19 многофакторно и не связано прямо с тяжестью заболевания. Предполагается, что вирус SARS-CoV-2 способен снижать активность мозгового нейротрофического фактора, повышать уровни маркеров аксо- нального повреждения, что свидетельствует о потенциальном повреждении ЦНС во время острой фазы болезни. К патогенетическим механизмам когнитивных нарушений при COVID-19 относят дыхательную недостаточность и гипоксию, цитокиновый шторм, нарушения гемостаза, повреждение эндотелия микроциркуляторного русла, непосредственное поражение головного мозга, возможно, по механизму молекулярной мимикрии [43, 44]. Нарушения ряда когнитивных функций (исполнительных функций и внимания) сопровождаются изменениями метаболизма глюкозы в префронтальных, подкорковых и островковых областях головного мозга [45]. COVID-19 повышает риск нарушения когнитивного функционирования независимо от наличия предшествующих когнитивных нарушений [46, 47]. На ухудшение внимания, вербальных и исполнительных функций влияет острый респираторный синдром и ассоциированная гипоксия [48]. В одном из исследований выраженность депрессивных симптомов выступила предиктором нарушений когнитивной сферы у пациентов, перенесших коронавирусную инфекцию [21].
ЗАКЛЮЧЕНИЕ
Долгосрочное негативное воздействие COVID-19 на здоровье населения очевидно. В настоящее время идут масштабные исследования по изучению распространенности депрессии, тревоги, делирия и посттравматического стрессового расстройства у пациентов с COVID-19 [49]. Эти пациенты имеют ряд длительных мультисистемных симптомов без доказанного поражения органов и при нормальных физических и лабораторных показателях, сопровождающихся снижением работоспособности разной степени выраженности, связанным, в том числе, с когнитивными нарушениями, одинаково представленными во всех возрастных группах [50].
Развитие постковидных нейропсихиатри-ческих расстройств связывают с сочетанным влиянием нейротропности вируса, системно- го воспаления и стрессовых психологических факторов. Полиморфность клинических последствий инфекции, вызванной SARS-CoV-2, обусловливает трудности диагностики и организации медицинской помощи пациентам, перенесшим COVID-19. Отсутствуют унифицированный подход к трактовке многочисленных фенотипических проявлений постковида и общепринятая терминология [51].
Постковидный синдром является социально значимым заболеванием, требует динамического наблюдения за больными и разработки реабилитационных программ. Необходимы широкий круг различных обследований пациентов и интегративный междисциплинарный подход к лечебно-реабилитационной помощи, сочетающий традиционную фармакотерапию, нефармакологические методы лечения, изменение поведения и образа жизни [52, 53]. Актуальна разработка единой стратегии в области общественного здравоохранения, направленной на борьбу с неблагоприятными долгосрочными последствиями пандемии [54-56].
Финансирование: Автор заявляет об отсутствии финансирования.
Список литературы Нейропсихиатрические последствия COVID-19
- Yong SJ, Liu S. Proposed subtypes of post-COVID-19 syndrome (or long-COVID) and their respective potential therapies. Rev Med Virol. 2022;32(4):e2315. DOI: 10.1002/rmv.2315
- Montani D, Savale L, Beurnier A, et al. Multidisciplinary approach for post-acute COVID-19 syndrome: time to break down the walls. Eur Respir J. 2021;58(1):2101090. DOI: 10.1183/13993003.01090-2021
- COVID-19 rapid guideline: managing the long-term effects of COVID-19. London: National Institute for Health and Care Excellence (NICE); December 18, 2020.
- World Health Organization. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. URL: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1
- Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021;11(1):16144. DOI: 10.1038/s41598-021-95565-8
- Crook H, Raza S, Nowell J, et al. Long covid-mechanisms, risk factors, and management. BMJ. 2021;374:n1648. DOI: 10.1136/bmj.n1648
- Wu L, Wu Y, Xiong H, et al. Persistence of Symptoms After Discharge of Patients Hospitalized Due to COVID-19. Front Med (Lausanne). 2021;8:761314. DOI: 10.3389/fmed.2021.761314
- Deng J, Zhou F, Hou W, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. 2021;1486(1):90-111. DOI: 10.1111/nyas.14506
- Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. ACS Chem Neurosci. 2020;11(7):995-998. DOI: 10.1021/acschemneuro.0c00122
- Shimohata T. Neuro-COVID-19. Clin Exp Neuroimmunol. 2022;13(1):17-23. DOI: 10.1111/cen3.12676
- Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611-627. DOI: 10.1016/S2215-0366(20)30203-0
- Taquet M, Geddes JR, Husain M, et al. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8(5):416-427. DOI: 10.1016/S2215-0366(21)00084-5
- Xie Y, Xu E, Al-Aly Z. Risks of mental health outcomes in people with covid-19: cohort study. BMJ. 2022;376:e068993. DOI: 10.1136/bmj-2021-068993
- Shanbehzadeh S, Tavahomi M, Zanjari N, et al. Physical and mental health complications post-COVID-19: Scoping review. J Psychosom Res. 2021;147:110525. DOI: 10.1016/j.jpsychores.2021.110525
- Daher A, Cornelissen C, Hartmann NU, et al. Six Months Follow-Up of Patients with Invasive Mechanical Ventilation due to COVID-19 Related ARDS. Int J Environ Res Public Health. 2021;18(11):5861. DOI: 10.3390/ijerph18115861
- Taquet M, Geddes JR, Husain M, et al. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8(5):416-427. DOI: 10.1016/S2215-0366(21)00084-5
- Beaud V, Crottaz-Herbette S, Dunet V, et al. Pattern of cognitive deficits in severe COVID-19. J Neurol Neurosurg Psychiatry. 2021;92(5):567-568. DOI: 10.1136/jnnp-2020-325173
- Carvalho-Schneider C, Laurent E, Lemaignen A, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect. 2021;27(2):258-263. DOI: 10.1016/j.cmi.2020.09.052
- Lambert NJ, Survivor Corps. COVID-19 “Long Hauler” Symptoms Survey Report. Indiana University School of Medicine; 2020. URL: https://dig.abclocal.go.com/wls/documents/2020/072720-wls-covid-symptomstudy-doc.pdf.
- Damiano RF, Guedes BF, de Rocca CC, et al. Cognitive decline following acute viral infections: literature review and projections for post-COVID-19. Eur Arch Psychiatry Clin Neurosci. 2022;272(1):139-154. DOI: 10.1007/s00406-021-01286-4
- Hampshire A, Trender W, Chamberlain SR, et al. Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine. 2021;39:101044. DOI: 10.1016/j.eclinm.2021.101044
- Мосолов С.Н. Длительные психические нарушения после перенесенной острой коронавирусной инфекции SARS-CoV-2 // Современная терапия психических расстройств. 2021. № 3. С. 2-23. [Mosolov SN. Long-term psychiatric sequelae of SARS-CoV-2 infection. Current Therapy of Mental Disorders. 2021;(3):2-23. (in Russ)]. DOI: 10.21265/PSYPH.2021.31.25.001. EDN: YLXJWB.
- Sher L. Are COVID-19 survivors at increased risk for suicide? Acta Neuropsychiatr. 2020;32(5):270. DOI: 10.1017/neu.2020.21
- Steardo L Jr, Steardo L, Verkhratsky A. Psychiatric face of COVID-19. Transl Psychiatry. 2020;10(1):261. DOI: 10.1038/s41398-020-00949-5
- Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18-22. DOI: 10.1016/j.bbi.2020.03.031
- Desforges M, Le Coupanec A, Dubeau P, et al. Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System? Viruses. 2019;12(1):14. DOI: 10.3390/v12010014
- Dantzer R. Neuroimmune Interactions: From the Brain to the Immune System and Vice Versa. Physiol Rev. 2018;98(1):477-504. DOI: 10.1152/physrev.00039.2016
- Netland J, Meyerholz DK, Moore S, et al. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82(15):7264-7275. DOI: 10.1128/JVI.00737-08
- Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol. 2016;16(1):22-34. DOI: 10.1038/nri.2015.5
- Najjar S, Pearlman DM, Alper K, et al. Neuroinflammation and psychiatric illness. J Neuroinflammation. 2013;10:43. DOI: 10.1186/1742-2094-10-43
- Mingoti MED, Bertollo AG, Simões JLB, et al. COVID-19, Oxidative Stress, and Neuroinflammation in the Depression Route. J Mol Neurosci. 2022;72(6):1166-1181. DOI: 10.1007/s12031-022-02004-y
- Montani D, Savale L, Noel N, et al. Post-acute COVID-19 syndrome. Eur Respir Rev. 2022;31(163):210185. DOI: 10.1183/16000617.0185-2021
- Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-920. DOI: 10.1016/S0140-6736(20)30460-8
- Carvalho PMM, Moreira MM, de Oliveira MNA, et al. The psychiatric impact of the novel coronavirus outbreak. Psychiatry Res. 2020;286:112902. DOI: 10.1016/j.psychres.2020.112902
- Ismael F, Bizario JCS, Battagin T, et al. Post-infection depressive, anxiety and post-traumatic stress symptoms: A prospective cohort study in patients with mild COVID-19. Prog Neuropsychopharmacol Biol Psychiatry. 2021;111:110341. DOI: 10.1016/j.pnpbp.2021.110341
- Javelot H, Weiner L, Hingray C, et al. COVID-19 and its psychological consequences: Beware of the respiratory subtype of panic disorder. Respir Physiol Neurobiol. 2020;282:103530. DOI: 10.1016/j.resp.2020.103530
- Lee CH, Giuliani F. The Role of Inflammation in Depression and Fatigue. Front Immunol. 2019;10:1696. DOI: 10.3389/fimmu.2019.01696
- Mazza MG, Palladini M, De Lorenzo R, et al. Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: Effect of inflammatory biomarkers at three-month follow-up. Brain Behav Immun. 2021;94:138-147. DOI: 10.1016/j.bbi.2021.02.021
- Okusaga O, Yolken RH, Langenberg P, et al. Association of seropositivity for influenza and coronaviruses with history of mood disorders and suicide attempts. J Affect Disord. 2011;130(1-2):220-225. DOI: 10.1016/j.jad.2010.09.029
- Robinson-Agramonte MA, Gonçalves CA, Noris-García E, et al. Impact of SARS-CoV-2 on neuropsychiatric disorders. World J Psychiatry. 2021;11(7):347-354. DOI: 10.5498/wjp.v11.i7.347
- Seang S, Itani O, Monsel G, et al. Long COVID-19 symptoms: Clinical characteristics and recovery rate among non-severe outpatients over a six-month follow-up. Infect Dis Now. 2022;52(3):165-169. DOI: 10.1016/j.idnow.2022.02.005
- Augustin M, Schommers P, Stecher M, et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. Lancet Reg Health Eur. 2021;6:100122. DOI: 10.1016/j.lanepe.2021.100122
- Lasso G, Honig B, Shapira SD. A Sweep of Earth’s Virome Reveals Host-Guided Viral Protein Structural Mimicry and Points to Determinants of Human Disease. Cell Syst. 2021;12(1):82-91.e3. DOI: 10.1016/j.cels.2020.09.006
- Yapici-Eser H, Koroglu YE, Oztop-Cakmak O, et al. Neuropsychiatric Symptoms of COVID-19 Explained by SARS-CoV-2 Proteins’ Mimicry of Human Protein Interactions. Front Hum Neurosci. 2021;15:656313. DOI: 10.3389/fnhum.2021.656313
- Kas A, Soret M, Pyatigoskaya N, et al. The cerebral network of COVID-19-related encephalopathy: a longitudinal voxel-based 18F-FDG-PET study. Eur J Nucl Med Mol Imaging. 2021;48(8):2543-2557. DOI: 10.1007/s00259-020-05178-y
- Beaud V, Crottaz-Herbette S, Dunet V, et al. Pattern of cognitive deficits in severe COVID-19. J Neurol Neurosurg Psychiatry. 2021;92(5):567-568. DOI: 10.1136/jnnp-2020-325173
- Halpin SJ, McIvor C, Whyatt G, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol. 2021;93(2):1013-1022. DOI: 10.1002/jmv.26368
- Robinson-Agramonte MA, Gonçalves CA, Noris-García E, et al. Impact of SARS-CoV-2 on neuropsychiatric disorders. World J Psychiatry. 2021;11(7):347-354. DOI: 10.5498/wjp.v11.i7.347
- Shi J, Gao Y, Zhao L, et al. Prevalence of delirium, depression, anxiety, and post-traumatic stress disorder among COVID-19 patients: protocol for a living systematic review. Syst Rev. 2020;9(1):258. DOI: 10.1186/s13643-020-01507-2
- Хасанова Д.Р., Житкова Ю.В., Васкаева Г.Р. Постковидный синдром: обзор знаний о патогенезе, нейропсихиатрических проявлениях и перспективах лечения // Неврология, нейропсихиатрия, психосоматика. 2021. Т. 13. № 3. С. 93-98. [Khasanova DR, Zhitkova YV, Vaskaeva GR. Post-COVID syndrome: a review of pathophysiology, neuropsychiatrie manifestations and treatment perspectives. Neurology, Neuropsychiatry, Psychosomatics. 2021;13(3):93-98. (in Russ)]. DOI: 10.14412/2074-2711- 2021-3-93-98.
- Deer RR, Rock MA, Vasilevsky N, et al. Characterizing Long COVID: Deep Phenotype of a Complex Condition. EBioMedicine. 2021;74:103722. DOI: 10.1016/j.ebiom.2021.103722
- Roth A, Chan PS, Jonas W. Addressing the Long COVID Crisis: Integrative Health and Long COVID. Glob Adv Health Med. 2021;10:21649561211056597. DOI: 10.1177/21649561211056597
- Verduzco-Gutierrez M, Estores IM, Graf MJP, et al. Models of Care for Postacute COVID-19 Clinics: Experiences and a Practical Framework for Outpatient Physiatry Settings. Am J Phys Med Rehabil. 2021;100(12):1133-1139. DOI: 10.1097/PHM.0000000000001892
- Ritchie K, Chan D. The emergence of cognitive COVID. World Psychiatry. 2021;20(1):52-53. DOI: 10.1002/wps.20837
- Schou TM, Joca S, Wegener G, Bay-Richter C. Psychiatric and neuropsychiatric sequelae of COVID-19 – A systematic review. Brain Behav Immun. 2021;97:328-348. DOI: 10.1016/j.bbi.2021.07.018
- Костенко Е.В., Энеева М.А., Петрова Л.В., Погонченкова И.В. Когнитивные нарушения и нейропсихиатрические последствия, связанные с COVID-19 // Доктор.Ру. 2021. Т. 20. № 5. С. 6-12. [Kostenko EV, Eneeva MA, Petrova LV, Pogonchenkova IV. Cognitive disorders and neuropsychiatric sequellae associated with COVID-19. Doctor.Ru. 2021;20(5):6-12. (in Russ)]. DOI: 10.31550/1727-2378-2021-20-5-6-12.