Некоторые молекулярно-генетические факторы риска фиброза миокарда (обзор литературы)
Автор: Гриценко О.В., Чумакова Г.А., Понасенко А.В., Груздева О.В.
Журнал: Сибирский журнал клинической и экспериментальной медицины @cardiotomsk
Рубрика: Обзоры и лекции
Статья в выпуске: 3 т.37, 2022 года.
Бесплатный доступ
Фиброз миокарда является многофакторным процессом, к которому предрасполагает ряд клеточных и молекулярных факторов, уровень которых детерминирован генетически. В данном обзоре рассмотрены некоторые генетические варианты, имеющие непосредственное отношение к развитию кардиофиброза и открывающие перспективы научных исследований по оценке риска сердечной недостаточности (СН) при различной сердечно-сосудистой патологии.
Фиброз миокарда, ген, генетическая вариабельность, сердечная недостаточность
Короткий адрес: https://sciup.org/149141436
IDR: 149141436 | УДК: 616.127-002.17:577.2 | DOI: 10.29001/2073-8552-2022-37-3-56-64
Текст научной статьи Некоторые молекулярно-генетические факторы риска фиброза миокарда (обзор литературы)
К настоящему времени получены доказательства того, что сердечно-сосудистые заболевания обладают высоким коэффициентом наследуемости. Полногеномные ассоциативные (GWAS), перекрестные «случай – контроль» и проспективные исследования выявили широкий спектр генетических вариантов, в том числе и в генах, регулирующих формирование фиброзной ткани [1]. Как известно, фиброз миокарда – это фундаментальный процесс, который наблюдается при ремоделировании сердца и считается одним из основных морфологических механизмов развития сердечной недостаточности (СН) с сохраненной фракцией выброса и ее прогрессирования. Кардиальный фиброз характеризуется накоплением внеклеточного матрикса (ВКМ) в миокарде [2]. Поскольку миокард взрослых млекопитающих обладает незначительной регенеративной способностью, наиболее обширное фиброзное ремоделирование желудочка обнаруживается при заболеваниях, связанных с острой гибелью кардиомиоцитов. Так, после инфаркта миокарда (ИМ) внезапная потеря большого количества кардиомиоцитов вызывает воспалительную реакцию, в конечном итоге приводящую к замене мертвого миокарда рубцом на основе коллагена [2]. Другие патофизиологические состояния вызывают более коварное интерстициальное и периваскулярное отложение коллагена [2]. К таковым относятся метаболические нарушения (такие как диабет [3] и ожирение [4]), которые вызывают прогрессирующие фиброзные изменения миокарда как у людей, так и у экспериментальных животных. Усовершенствованные методы диагностики, более глубокое понимание путей передачи молекулярных сигналов и потенциальные антифибротические методы лечения являются ключевыми областями исследований в данном направлении. Тем не менее лабораторная оценка фиброза миокарда требует большего изучения, а также сопоставления полученных данных с инструментальными методами исследования процесса фиброзирования [5]. В литературе описано множество генетических маркеров фиброгенеза. В работе И.А. Гончаровой и соавт. [1] были изучены однонуклеотидные маркеры (SNV – short nucleotide variant; в более ранних работах обозначено как: SNP – shot nucleotide polymorphisme), локализованные в генах, для которых показано значение изменения их экспрессии при заболеваниях, связанных с фиброзом различных органов [1]. В данном исследовании получены новые значимые для популяции Западной Сибири научные данные, которые открывают перспективы к изучению данных генов у пациентов с различной сопутствующей патологией, в том числе с различными метаболическими нарушениями. Интерес представляют выявленные нестандартные маркеры, на некоторых из которых сконцентрирован наш литературный обзор.
Некодирующая антисмысловая РНК
Недавние достижения в технологиях высокопроизводительного секвенирования сыграли решающую роль в открытии и классификации видов рибонуклеиновых кислот (РНК), известных под общим названием некодирующие РНК (нкРНК). Эти РНК являются результатом транскрипции генома млекопитающих и составляют 75% генома человека, тогда как только 3% транскриптов транслируются в белки [6]. Термин нкРНК обычно используется для РНК, которая не кодирует белок, но это не означает, что такие РНК не содержат информации и не выполняют функцию. Несколько классов нкРНК участвуют в модуляции внутренних сигналов, которые контролируют различные уровни экспрессии генов в физиологии и развитии [7]. Последние достижения в области молекулярной биологии показали, что экспрессия генов в значительной степени регулируется нкРНК [8]. Исследования подтверждают участие нкРНК в различных физиологических процессах, а технологии секвенирования нового поколения вместе с биоинформационным анализом выявили повсеместную транскрипцию неожиданно большого разнообразия молекул РНК. Было показано, что среди них микроРНК (mirRNA), длинные некодирующие РНК (lncRNAs) и кольцевые РНК (circRNAs) участвуют в регуляции транскрипции на разных уровнях. Недавние исследования свидетельствуют о том, что часть геномов млекопитающих и других сложных организмов на самом деле транскрибируется в нкРНК, многие из которых альтернативно сплайсируются и/или преобразуются в более мелкие продукты. Описаны сотни нкРНК, участвующих в нескольких процессах, таких как созревание РНК, регуляция транскрипции, ремоделирование хроматина и посттранскрипционные модификации РНК, поэтому не подлежит сомнению тот факт, что нкРНК играют решающую роль в сетях регуляции генов [8].
Полиморфизм, основанный на вариативном присутствии одного нуклеотида в структуре гена представляет собой наиболее распространенный тип изменчивости генома человека. SNP, расположенные в генах белок-ко-дирующих и нкРНК, классифицируются как нейтральные и функциональные. Нейтральные мутации не приводят к заметным нарушениям, в то время как функциональные влияют на различные биологические процессы и постоянно создают риск мультифакторных заболеваний. Функциональные SNP, обнаруженные в промоторах генов белок-кодирующих и нкРНК, называемые регуляторными SNP (rSNP) и микроРНК rSNP (miR-rSNP) соответственно, влияют на экспрессию генов [9]. Таким образом, огромный интерес к этой области вызван многочисленными исследованиями, в которых анализируются и очерчиваются функции этого нового класса РНК. Было показано, что различные нкРНК играют ключевую роль в важных биологических процессах и нарушении их регуляции с различными заболеваниями [10, 11]. Накапливаются данные о связи нкРНК с развитием фиброза сердца [12].
Так, была идентифицирована lncRNA WISPER ( Wisp2 суперэнхансер ассоциированная РНК), которая регулирует экспрессию Wisp2, вовлеченного в патологический миокардиальный фиброз. Обнаружено, что lncRNA WISPER одинаково распределен между ядром и цитоплазмой, что указывает на то, что он может играть роль как в транскрипционных, так и в посттранскрипционных регуляторных процессах. R. Micheletti и соавт. продемонстрировали, что как экспрессия Wisper в эксперименте на мышиной модели ИМ, так и экспрессия WISPER у пациентов со стенозом аорты коррелируют с тяжелым фиброзом миокарда [12]. На мышиной модели оценена экспрессия Wisper в течение 28-дневного периода после индуцированного ИМ. При этом профили экспрессии продемонстрировали ожидаемую кинетику для тех генов, которые кодируют белки, связанные с фиброзом и гипертрофией. Wisper был максимально экспрессирован через 14 дней после ИМ, что соответствует пролиферативной фазе, в которой миофибробласты активно секретируют коллаген и другие компоненты ВКМ. Временная кинетика индукции Wisper вовлекает этот транскрипт в сердечный фиброз, приводящий к патологическому ремоделированию [12]. Было показано, что несколько нкРНК контролируют важные процессы, которые вносят вклад в патофизиологические последствия ИМ. Гибель кардиомиоцитов и постишемическая неоваскуляризация также могут быть опосредованы нкРНК через регуляторные механизмы. Связывание зрелых микроРНК с мРНК отрицательно влияет на экспрессию специфических белков либо путем деградации связанной мРНК-мишени, либо путем прямого ингибирования трансляции [13]. В ранее проведенных исследованиях показана роль нкРНК в развитии СН. Гипертрофия желудочков сердца, развивающаяся на фоне множества внешних и внутренних стрессовых факторов, и опосредованная активация микроРНК (миРНК)-195 приводят к ремоделированию сердца и СН у трансгенных мышей [14]. Сверхэкспрессия отдельных стресс-индуцируемых нкРНК в первичных кардиомиоцитах in vitro вызывает гипертрофический рост и сборку саркомеров, а сверхэкспрессия миРНК-195 в опытах in vivo была достаточной, чтобы вызвать гипертрофию миоцитов и ухудшение сердечной функции, что приводило к быстрому развитию СН [15]. Исследования роли нкРНК в патогенезе фиброзирования миокарда затронули и область влияния длинных некодирующих РНК (днРНК). Показано, что в опытах in vivo нокдаун днРНК LINC00622 и LINC01711 приводит к изменениям экспрессии генов, связанным с клеточными и воспалительными реакциями соответственно [16]. На основании проведенных исследований авторами создано приложение «FibroDB», предназначенное для дальнейшего продвижения исследований в оценке функций и механизмов участия днРНК в процессах фиброзирования [16].
Матриксные металлопротеазы и тканевой ингибитор металлопротеаз (ТИМП)
Сердце реагирует на повреждение выработкой белков матрикса и последующим ремоделированием ВКМ, что приводит к изменениям геометрии желудочков и СН. В синтез ВКМ вносят вклад несколько различных типов клеток: поврежденные паренхиматозные клетки, кото- рые могут подвергаться фенотипической трансформации под влиянием микроокружения, инфильтрирующие или резидентные воспалительные клетки, которые активируются высвобождением нейрогормонов или хемокинов/ цитокинов, а также тканевые фибробласты [17]. Для этого процесса необходимы как матриксные металлопротеиназы (ММП), так и их тканевые ингибиторы (ТИМП). ММП представляют собой протеазы, активируемые цинком, секретируемые в неактивной форме, и могут быть обнаружены в растворимых и мембраносвязанных формах [18]. Из 23 белков, описанных в настоящее время у людей, только часть экспрессируется в миокарде с различной аффинностью к белкам в качестве субстратов, включая ВКМ (коллаген, ламинин, фибронектин, эластин), другие ММП, биоактивные пептиды и факторы роста [17]. Структура MMП жестко регулируются транскрипционными, посттранскрипционными и посттрансляционными контрольными точками. Транскрипционная регуляция MMP в первую очередь определяется активностью промотора восходящего гена, посредством чего ряд внутриклеточных сигнальных факторов связывается со специфическими последовательностями внутри последовательности промотора MMP. Таким образом, существует значительный интерес к заменам нуклеиновых кислот (т. е. однонуклеотидный полиморфизм), которые происходят в областях промотора MMP и связаны с общими уровнями ММП и, что наиболее важно, связаны с сердечно-сосудистыми исходами [19, 20]. Кроме того, некоторые однонуклеотидные замены в MMP-9 придают аддитивный риск сердечно-сосудистых событий у пациентов с другими факторами риска, такими как диабет и ожирение [21]. Оценка вариабельности структуры генов, связанных с индукцией MMП в подгруппах риска, является важной областью для дальнейших исследований и уточнений с точки зрения оценки сердечно-сосудистого риска. В данном обзоре рассмотрим те ММП, которые имеют потенциальное отношение к миокарду.
Известно, что интерстициальная коллагеназа (MMП-1) в основном экспрессируется лейкоцитами, фибробластами и эндотелиальными клетками [22]. Исследования MMP-1 осложняются наличием двойных изоформ и отсутствием значительной гомологии между мышами и людьми, так, у людей имеется только одна изоформа MMP-1, а у мышей – две: MMP-1а (59% гомологичности с человеческой MMP-1) и MMP-1b) 57% гомологии с человеческим MMP-1) [22]. MMП-1 преимущественно разрушает коллагены I и III; по сравнению с остальными известными ММП, ММП-1 обладает высокой субстратной специфичностью в отношении фибриллярных коллагенов, а также других белков ВКМ, таких как аггрекан, перликан, версикан и протеогликаны. ММП-1 инициирует деградацию коллагеновых волокон в левом желудочке путем расщепления коллагена на фрагменты 3/4 и 1/4. Затем эти фрагменты разворачиваются и расщепляются MMП-2, -9 и -3 [23]. Несмотря на то, что известно увеличение в 20 раз транскрипционной активности MMP-1 при наличии инсерции дополнительного нуклеотида G в сайте –1607 промотора (1G > 2G), значение мутационной изменчивости MMP-1 в литературе представлены противоречивыми данными. Так, в исследовании на когорте в Бразилии с включением 313 пациентов с СН с систолической дисфункцией левого желудочка и 367 здоровых лиц контрольной группы показано, что сайт –1607 (1G/2G) MMP-1 не связан с большей предрасположенностью раз- вития СН. Однако у носителей аллеля 2G MMP-1 чаще в анамнезе имеется СН ишемической этиологии и ИМ, но выживаемость в трехлетней перспективе у этой группы выше по сравнению с носителями гомозиготного генотипа 1G/2G [24]. В других исследованиях [24] показана связь аллеля 2G с повышенным риском ишемической болезни сердца (ИБС), риском стеноза сонных артерий и усилением ремоделирования левого желудочка после ИМ.
В исследовании, где у 42 больных жителей Шотландии, перенесших первый ИМ, изучали связь между ремоделированием левого желудочка и полиморфизмом инсерции/делеции сайта –1607 MMP-1 , выявлено, что носители гомозиготного генотипа 2G / 2G имели повышенный риск ремоделирования по сравнению с гомозиготами 1G / 1G и гетерозиготами 1G / 2G [25].
Стромелизин 1 (ММП-3) секретируется сердечными фибробластами и макрофагами [26]. MMП-3 расщепляет несколько компонентов ВКМ, включая коллаген, фибронектин, ламинины, протеогликаны и витронектин, кроме того, MMП-3 активирует ряд MMП, включая MMP-1, -7 и -9 [22]. Таким образом, MMP-3 считается вышестоящим активатором MMП. Секретируемый кислый и богатый цистеином белок (SPARC) также может быть расщеплен MMП-3 с образованием трех биологически активных пептидов (Z-1, Z-2 и Z-3). Фрагмент Z-1 увеличивает ангиогенез и рост сосудов, тогда как фрагменты Z-2 и Z-3 ингибируют пролиферацию клеток [27]. ММП широко изучались как возможные маркеры для прогнозирования развития сердечно-сосудистых заболеваний, особенно при ремоделировании после ИМ и СН. Полиморфизм структуры промотора в сайте –11171 MMP-3 считается регулятором в развитии ИМ и исходов СН [22]. Например, аллель 6A –1171 имеет более низкую промоторную активность по сравнению с аллелем 5A и обнаруживается значительно реже у пациентов с ИМ, чем у пациентов из контрольной группы. Влияние этого структурного элемента промотора MMP-3 на выживаемость у пациентов с СН с ишемической и неишемической кардиомиопатией различается. Аллель 6A MMP-3 является независимым предиктором сердечной смертности у пациентов с неишемической СН. Напротив, нет доказательств какого-либо влияния генотипа сайта –1171 MMP-3 на сердечные события у пациентов с ишемической кардиомиопатией [24].
Ген MMP-9 (также известной как желатиназа или коллагеназа типа V) MMP-9 кодирует мультидоменный фермент, участвующий в деградации ВКМ и основного белка миелина [18, 28].
ММП-9 секретируется большим количеством типов клеток, включая кардиомиоциты, эндотелиальные клетки, нейтрофилы, макрофаги и фибробласты [29]. S. Blankenberg и соавт. были первыми, кто использовал MMП-9 в качестве нового прогностического биомаркера развития дисфункции левого желудочка и поздней выживаемости у пациентов с сердечно-сосудистыми заболеваниями [30], а также было показано, что MMП-9 коррелирует с уровнем интерлейкина-6, С-реактивным белком и концентрациями фибриногена в плазме, указывая на то, что MMП-9 может прогнозировать сердечно-сосудистый исход независимо от ассоциации с воспалительными маркерами [30]. MMП-9 принимает участие в процессах воспаления, ремоделирования ткани и репарации, мобилизации матрикссвязанных факторов роста и процессинга цитокинов [31]. Имеются данные о том, что экспрессия ММП-9 повышается при сердечном фи- брозе. Используя животную модель, H. Dai и соавт. показали возможность частичного сохранения сердечной функции при ИМ и снижение фиброза в сердечной мышце на нокаутных по MMP-9 крысах [31]. В исследовании I.B. Squire и соавт. продемонстрировано, что повышенное содержание ММП-9 в плазме коррелирует с большим объемом левого желудочка и его большей дисфункцией после ИМ у людей [32]. В то же время сайт промотора –1562 C/T MMP-9 ассоциируется с повышенной частотой развития ИМ [33]. При этом наличие ассоциации генотипа и количества ММП-9 в плазме варьирует в зависимости от этнической принадлежности: у здоровых лиц европеоидной расы, вариабельный нуклеотидный сайт –1562 MMP-9 и микросателитный сайт –90 (CA)(13–25) не показали связи с изменением концентраций MMП-9 в плазме, тогда как положительная ассоциация обнаружена у здоровых афроамериканцев при носительстве генотипа HH –90 (CA)(14–24), имеющего два аллеля с частотой са-телитных повторов ≥ 21 [22]. Межэтническое различие в частоте встречаемости вариантов структуры промотора MMP-9 может обусловливать наличие противоречивых данных в исследованиях по этом направлении. Еще в 2010 г. R. Lacchini и соавт. [34] показали большую распространенность аллелей С –1306 (р < 0,0001), Т –1562 (р = 0,03), а также аллели с > 21 повтором для полиморфизма –90 (СА)(14–24) (р = 0,0017) среди чернокожих жителей Бразилии, по сравнению с белыми. Более того, два гаплотипа, сочетающие «вредные» аллели, также с большей частотой встречаются у чернокожих, чем у белых (31 против 16,4% соответственно; p < 0,05). Межэтнические различия могут помочь объяснить не только более высокую распространенность сердечно-сосудистых заболеваний у чернокожих по сравнению с белыми, но и противоречивость полученных результатов при изучении связи вариабельности сайта –1562 MMP-9 с различными фенотипами. Так, в исследовании, проведенном в Бразилии, этот сайт в промоторе MMP-9 не показал связи с предрасположенностью к СН или выживаемостью, связанной с СН [22]. В исследовании, проведенном во Франции, наличие аллеля T –1562 MMP-9 не ассоциировалось с более низкой фракцией выброса, но является независимым предиктором сердечной смертности [22]. Оба исследования имели схожие характеристики пациентов, что подтверждает ранее полученные данные в этнических различиях и что полиморфизм MMP-9 в сайте –1562 не может использоваться в качестве биомаркера во всех популяциях.
Активность ММП жестко регулируется эндогенными тканевыми ингибиторами металлопротеиназ (ТИМП), которые препятствуют деградации матрикса. Дисбаланс между уровнями MMП и TИМП приводит к нарушению регуляции протеолитической активности и обычно неблагоприятному ремоделированию ВКМ, оказывает свое влияние на клеточную пролиферацию, дифференцировку, апоптоз и ангиогенез посредством MMП-независимых механизмов, что в конечном итоге приводит к прогрессированию фиброза и последующей СН [35]. Существует четыре известных вида ТИМП, из которых наиболее изучены ТИМП-1 и ТИМП-2. Различные ТИМП ингибируют разные ММП, например, ТИМП-1 более эффективно ингибирует ММП-1, ММП-3, ММП-7 и ММП-9, тогда как ТИМП-2 ингибирует ММП-2 лучше, чем ТИМП-1. TИМП-2 является единственным членом семейства TИМП, который специфически взаимодействует как с MT1-MMП, так и с pro-MMП-2 на клеточной поверхности, поэтому действует как ингибитор MMП и как активатор MMП. Более того, ТИМП-2 обладает способностью непосредственно подавлять пролиферацию эндотелиальных клеток [36]. Учитывая двойную роль TИМП-2, была исследована его роль в заболеваниях сердца и выявлено, что недостаток TИМП-2 приводит к усилению сердечной дисфункции и ремоделированию левого желудочка после перегрузки давлением из-за избыточной активности ММП мембранного типа и потери интегрина β1D, что приводит к неравномерному ремоделированию ВКМ и нарушению взаимодействия миоцитов с ВКМ [37].
При заболеваниях сердца уровни экспрессии MMП и ТИМП не сбалансированы, что может способствовать распаду коллагена в ткани миокарда и изменению внутриклеточной передачи сигналов кардиомиоцитами [38]. Повышенные уровни TИМП-2 связаны с систолической дисфункцией, ИМ, конечной стадией идиопатической дилатационной кардиомиопатии и острым повреждением почек 2-й стадии при декомпенсированной СН [38, 39]. Однако в других исследованиях сообщалось о снижении уровня TИМП-2 у пациентов с ИБС, систолической СН и у тех, кто умер от СН или был госпитализирован по поводу СН после операции на митральном клапане [38].
ТИМП могут опосредованно влиять на ремоделирование миокарда, развитие гипертрофии и фиброз при заболеваниях сердца. Так, канадскими учеными было показано, TИМП-2 и TИМП-3 играют фундаментальную и дифференциальную роль в развитии патологического ремоделирования, независимо от их функции, ингибирующей ММП. У мышей TИМП2(-/-) и TИМП3(-/-) при проведении эхокардиографии выявлена сохранная фракция выброса, однако наблюдалось нарушение диастолической функции левого желудочка. Гипертрофия левого желудочка у мышей TИМП2(-/-) нарушала активную релаксацию, в то время как избыточный фиброз у мышей TИМП3(-/-) повышал пассивную жесткость левого желудочка [40].
Так, в исследовании с участием 300 пациентов с СН любой этиологии и сниженной фракцией выброса левого желудочка (≤45%), где СН была диагностирована в соответствии с рекомендациями ACCF/AHA, выявлено, что полиморфизм промотора –418 G/C TIMP1 не связан ни с предрасположенностью к СН, ни с выживаемостью у пациентов с СН со сниженной фракцией выброса левого желудочка в популяции из Южной Бразилии [41]. Имеются противоречивые данные о связи полиморфизма TIMP12 с ремоделированием тканей, связанным с функцией сердца при ИБС. Так, в исследовании не было выявлено связи между –418 G/C TIMP2 и ИБС или ИМ в турецкой популяции [42]. А в исследовании на китайской популяции [43] авторы проспективного исследования оценили влияние носительства тех или иных аллелей вариабельных сайтов –418 G/C TIMP2 и –1562 C/T MMP9 на параметры реполяризации, включая дисперсию интервала QT (QTd), а также пик и конец интервала зубца T (Tpe). Показано более значимое увеличение QTd (p = 0,033) и QTcd (дисперсия скорректированного QT; p = 0,010), у носителей C-аллеля TIMP2. Эта ассоциация продемонстрировала статистическую значимость и при многомерном анализе (p = 0,012 и p = 0,003 для QTd и QTcd соответственно), характеризующем динамику реполяризации у пожилых китайцев в четырехлетнем наблюдении, что, в свою очередь, демонстрирует значимость наследствен- ности в данном сигнальном каскаде, запускающем ремоделирование сердца и фиброз с изменением параметров реполяризации.
Экспериментальные работы также немногочисленны, и их результаты также неоднозначны. В эксперименте на животной модели у собак породы бигль наблюдали снижение уровня экспрессии TIMP2 и подавление белковой экспрессии TIMP-2 в тканях мышц предсердия [44]. В эксперименте in vitro [45] использованы индуцированные Ang II сердечные фибробласты (CFB), трансфицированные пре-миРНК-214, анти-миРНК-214 и их олигоконтро-ли. Установлено, что по сравнению с контролем экспрессия TIMP1 увеличивалась в опытных культурах наравне с коллагеном типа I ( COL I ), коллагеном типа III ( COL III ) и трансформирующим фактором роста –β1( TGF β1 ).
Трансформирующий фактор роста
Transforming growth factor beta type I (TGF-β1) представляет собой повсеместно экспрессируемый полифунк-циональный цитокин, участвующий во многих физиологических и патологических процессах. Было показано, что TGF-β1 имеет фундаментальное значение в развитии, физиологии и патологии сосудистой системы. Согласно литературным данным, TGF-β1 может секретироваться несколькими типами клеток, включая мононуклеарные клетки периферической крови, макрофаги, тромбоциты, эндотелиальные клетки, гладкомышечные клетки сосудов, миофибробласты и почечные клетки [46]. Вывод о том, что уровень TGF-β1 в периферической крови детерминирован генетически, в настоящее время является доказанным фактом [47].
Хотя аминокислотная последовательность активной формы TGF-β1 у млекопитающих высоко консервативна [46], также идентифицированы множественные вариации TGF-β1, которые могут вызывать вариабельную конститутивную или индуцированную экспрессию TGF-β1 или структурные изменения белка и, как следствие, измененную активность TGF-β1. К настоящему времени восемь сайтов полиморфизма однонуклеотидных замен и делеции/вставки признаны влияющими на экспрессию и активность TGF-β1, включая два сайта в области промотора: rs1800468 (–800 G/A) и rs1800469 (–509 C/T); два сайта в области сигнального пептида: rs1982073 (868 T/C, Leu10Pro) и rs1800471 (913 G/C, Arg25Pro); и сайт в районе, кодирующем прекурсорную часть белка: rs1800472 (11929 C/T, Thr263Ile) [46–48]. Исследователи уделяют особое внимание следующим полиморфизмам гена TGF-β1, связанным с сердечно-сосудистыми заболеваниями: сайт rs1800469 промотора и сайт первого экзона rs1800471 [48]. Получены данные о значимости носительства вариантных аллелей сайта –509 C > T TGF-β1, а также мажорных аллелей сайтов 869 T > C и 915 G > C TGF-β1 ассоциированы с более высоким уровнем белка в плазме [49].
Широко изучена роль полиморфизма TGF-β1 в развитии атеросклероза. Показано, что некоторые варианты TGF-β1 ассоциированы с тяжестью течения атеросклероза коронарных артерий и наследственной предрасположенностью к ИМ, но эта связь неодинакова для разных этнических групп [50]. Так, например, в одном из исследований на популяции западного региона России (Москва) при проведении комплексного анализа ассоциации ИМ с комбинациями аллелей/генотипов трех полиморфных сайтов TGFβ1 указывает на их кумулятивный эффект.
Анализ предрасположенности к раннему ИМ (≤50 лет) выявил положительную ассоциацию аллеля –509T и генотипа 869T/T TGFβ1 , а также их аддитивность. Анализ предрасположенности к рецидивирующему ИМ выявил ассоциацию генотипа –509T/T TGFβ1 . Полученные результаты свидетельствуют о важной роли структурного постоянства гена TGF-β1 в предрасположенности к ИМ, включая ранний и рецидивирующий ИМ, у русских [49], тогда как в ряде публикаций не сообщается о значимой связи полиморфизма TGFβ1 с ИМ у представителей европеоидной расы [51].
Измененная экспрессия TGFβ1, возникающая из-за множественной вариативности промоторных регионов гена, влияет на широкий спектр нормальных клеточных и патологических процессов, включая фиброзирование миокарда. Как профибротический цитокин, TGF-β1 может индуцировать дифференцировку сердечных фибробластов в миофибробласты, что играет важную роль в процессе сердечного фиброза [52]. Научных публикаций о влиянии полиморфизма TGFβ1 на развитие фиброза и СН крайне мало. Имеются лишь единичные данные, полученные на ограниченных выборках. Так, в одном из последних исследований на смешанной популяции западной части России проанализирована генетическая предрасположенность к фиброзу миокарда у реципиентов трансплантата сердца, обнаружены значимые ассоциации между этим признаком и носительством минорного аллеля rs1800470. Известно, что аллель А этого полиморфного сайта ассоциирован с высоким уровнем TGF-β1 в периферической крови, который является мощ- ным стимулятором продукции ВКМ; а его гиперпродукция связана с фиброзными нарушениями и развитием фиброза миокарда [47].
Эластин
Эластин является одним из основных нерастворимых компонентов ВКМ. Эластические волокна подвержены растяжению и сокращению, они придают ткани важное свойство эластичности и упругости, а также поддерживают архитектуру при многократном растяжении. Зрелые эластические волокна состоят из ядра из тропоэластина, окруженного фибриллином и микрофибриллами. Эластичность миокарда зависит от соотношения мышечных волокон к фиброзной ткани и плотности сшитого коллагена [53]. Ген эластина человека ( ELN ) расположен на хромосоме 7 и содержит 34 экзона, каждый из которых кодирует либо гидрофобный, либо сшивающий домен в чередующемся порядке [54] (рис. 1). В течение жизни организма экспрессия гена эластина и синтез белка происходят в узких временных рамках, начиная с позднего эмбрионального развития и заканчивая подростковым возрастом, практически без образования эластина de novo на протяжении всей взрослой жизни. Узкие временные рамки экспрессии и синтеза эластина необычны для компонента ВКМ, поскольку, как правило, производство ВКМ является динамичным. Из-за устойчивости эластина и периода полужизни около 70 лет ограниченный период времени экспрессии и синтеза достаточен для того, чтобы белок сохранялся на протяжении всей жизни у большинства видов [53].
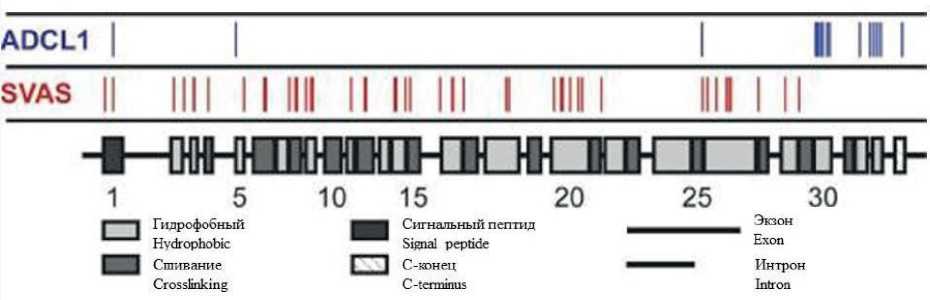
Рис. 1. Доменная структура гена эластина человека. Чередующиеся гидрофобные и сшивающие домены обычно транскрибируются с отдельных экзонов. Расположение 64 уникальных полиморфных сайтов, связанных либо с надклапанным стенозом аорты (SVAS; красный, 49 мутаций, не включая большие делеции), либо с аутосомно-доминантным кутис laxa-1 (ADCL1; синий, 15 мутаций). Адаптировано из [53]
Fig. 1. Domain structure of the human elastin gene. Alternating hydrophobic and cross-linking domains are usually transcribed from separate exons. Location of 64 unique polymorphic sites associated with either supravalvular aortic stenosis (SVAS; red, 49 mutations, not including large deletions) or autosomal dominant cutis laxa-1 (ADCL1; blue, 15 mutations). Adapted from [53]
Описаны мутации в гене эластина, которые вызывают надклапанный стеноз аорты (SVAS), связанный с недостаточностью эластина, и аутосомно-доминантный кутис laxa-1 (ADCL1), связанный с тканеспецифическими дефектами сборки эластических волокон [53]. Приобретенные заболевания, как правило, связаны с деградацией эластических волокон или их биохимической модификацией. Эта деградация инициирует деструктивный каскад ремоделирования артерий, который трудно остановить и нельзя обратить вспять [16], основываясь на уровне современных научных данных.
Изучена роль эластина в развитии СН у пациентов с ИМ. Известно, что после ИМ истончение и расширение фиброзного рубца способствуют прогрессированию СН. Потеря эластина является основным фактором неблагоприятного ремоделирования ВКМ сердца после ИМ, а восстановление эластических свойств области инфаркта может предотвратить дисфункцию желудочков. Это было показано в экспериментальном исследовании, проведенном канадскими учеными. Крысам вводили стромальные клетки костного мозга в зону ИМ для сверхэкспрессии эластина. Гиперэкспрессия эластина в зоне ИМ сохраня- ла эластическую структуру ВКМ, что, в свою очередь, сохраняло диастолическую функцию, предотвращало развитие дилатации желудочков и СН. Отложение эластина в зоне ИМ было связано с сохранением структурной целостности ткани миокарда по сравнению с контролем. В результате, толщина рубца миокарда и диастолическая растяжимость сохранялись, а распространение инфаркта предотвращалось. Модификация гена эластина имплантированного миобласта может усиливать и поддерживать долгосрочные эффекты сохранения сердечной функции [55].
Однако исследований о роли наследственности в отношении эластина при фиброзировании миокарда недостаточно для формирования объективного представления его механизмах.
Заключение
Таким образом, изучение полиморфных вариантов отдельных генов, участвующих в процессах фиброзирования миокарда, представляется крайне актуальным, так как данных о их взаимосвязи с фиброзированием миокарда, особенно при метаболических нарушениях, крайне мало. Дальнейшее изучение данной проблемы необходимо для усовершенствования ранней диагностики фиброза миокарда, в том числе на доклиническом этапе, для разработки терапевтических стратегий эффективных для ингибирования миокардиального фиброза и профилактики развития СН. В целом, основываясь на разрозненных литературных данных, можно говорить и о целесообразности проведения новых научных исследований в этом направлении.
Список литературы Некоторые молекулярно-генетические факторы риска фиброза миокарда (обзор литературы)
- Гончарова И.А., Печерина Т.Б., Марков А.В., Кашталап В.В., Тара-сенко Н.В., Пузырев В.П. и др. Роль генов фиброгенеза в формировании подверженности к коронарному атеросклерозу. Кардиология. 2018;58(8):33-44. DOI: 10.18087/cardio.2018.8.10160. Goncharova I.A., Pecherina T.B., IVIarkov A.V., Kashtalap V.V., Tarasen-ko N.V., Puzyrev V.P. et al. Fibrogenesis genes and susceptibility to coronary atherosclerosis. Kardiologiia. 2018;58(8):33-44. (In Russ.) DOI: 10.18087/cardio.2018.8.10160.
- Ping K., Panagiota C., Frangogiannis N.G. The pathogenesis of сardiac fibrosis. Cell Mol. Life Sci. 2014;71(4): 549-574. DOI: 10.1007/s00018-013-1349-6.
- Asbun J., Villarreal F.J. The pathogenesis of myocardial fibrosis in the setting of diabetic cardiomyopathy. J. Am. Coll. Cardiol. 2006;47(4):693-700. DOI: 10.1016/j.jacc.2005.09.050.
- Bharati S., Lev М. Cardiac conduction system involvement in sudden death of obese young people. Am. Heart J. 1995;129(2):273-281. DOI: 10.1016/0002-8703(95)90008-x.
- Печерина Т.Б., Кутихин А.Г. Биомаркеры фиброза миокарда и их генетическое регулирование у пациентов с сердечной недостаточностью. Российский кардиологический журнал. 2020;25(10):3933. DOI: 10.15829/1560- 4071-2020-3933. Pecherina T.B., Kutikhin A.G. Biomarkers of myocardial fibrosis and their genetic regulation in patients with heart failure. Russian Journal of Cardiology. 2020;25(10):3933. (In Russ.). DOI: 10.15829/1560-4071-20203933.
- Chan J.J., Tay Y. Noncoding RNA: RNA regulatory networks in cancer. Int. J. Mol. Sci. 2018;19(5):1310. DOI: 10.3390/ijms19051310.
- Wlattick J.S., Wlakunin I.V. Non-coding RNA. Hum. Mol. Genet. 2006;(1):R17-29. DOI: 10.1093/hmg/ddl046.
- Panni S., Lovering R.C., Porras P., Orchard S. Non-coding RNA regulatory networks. Biochim. Biophys. Acta Gene Regul. Mech. 2020;1863(6):194417. DOI: 10.1016/j.bbagrm.2019.194417.
- Ramirez-Bello J., Jimenez-morales М. Functional implications of single nucleotide polymorphisms (SNPs) in protein-coding and non-coding RNA genes in multifactorial diseases. Gac. Med. Mex. 2017;153(2):238-250.
- Kwok Z.H., Tay Y. Long noncoding RNAs: Lincs between human health and disease. Biochem. Soc. Trans. 2017;45(3):805-812. DOI: 10.1042/ BST20160376.
- Anastasiadou E., Jacob L.S., Slack F.J. Non-coding RNA networks in cancer. Nat. Rev. Cancer. 2018;18(1):5-18. DOI: 10.1038/nrc.2017.99.
- Wlicheletti R., Plaisance I., Abraham B.J., Sarre A., Ching-Chia Ting, Alexanian М. et al. The long noncoding RNA Wisper controls cardiac fibrosis and remodeling. Sci. Transl. Med. 2017;9(395):eaai9118. DOI: 10.1126/scitranslmed.aai9118.
- Boon R.A., Dimmeler S. WlicroRNAs in myocardial infarction. Nat. Rev. Cardiol. 2015;12(3):135-142. DOI: 10.1038/nrcardio.2014.207.
- Lu P., Ding F., Xiang Y.K., Hao L., Zhao М. Noncoding RNAs in Cardiac Hypertrophy and Heart Failure. Cells. 2022;11(5):777. DOI: 10.3390/ cells11050777.
- Rooij E., Sutherland L.B., Liu N., Williams A.H., WlcAnally J., Gerard R.D. et al. A signature pattern of stress-responsive microRNAs that can evoke cardiac hypertrophy and heart failure. Proc. Natl. Acad. Sci. U S A. 2006;103(48):18255-18260. DOI: 10.1073/pnas.0608791103.
- Ilieva М., Wliller H.E., Agarwal A., Paulus G.K., Wladsen J.H., Bishop A.J.R. et al. FibroDB: Expression Analysis of Protein-Coding and Long Non-Coding RNA Genes in Fibrosis. Noncoding RNA. 2022;28;8(1):13. DOI: 10.3390/ncrna8010013.
- Trinh K., Julovi S.M., Rogers N.M. The role of matrix proteins in cardiac pathology. Int. J. Mol. Sci. 2022;23(3):1338. DOI: 10.3390/ijms23031338.
- Mohammadhosayni M., Khosrojerdi A., Lorian K., Aslani S., Imani D., Razi B. et al. Matrix metalloproteinases (MMPs) family gene polymorphisms and the risk of multiple sclerosis: Systematic review and meta-analysis. BMC Neurol. 2020;20(1):218. DOI: 10.1186/s12883-020-01804-2.
- Li T., Lv Z., Jing J.J., Yang J., Yuan Y. Matrix metalloproteinase family polymorphisms and the risk of aortic aneurysmal diseases: A systematic review and meta-analysis. Clin. Genet. 2018;93(1):15-32. DOI: 10.1111/ cge.13050.
- Opstad T.B., Arnesen H., Pettersen A.A., Seljeflot I. The MMP-9 -1562 C/T polymorphism in the presence of metabolic syndrome increases the risk of clinical events in patients with coronary artery disease. 2014;9(9):e106816 DOI: 10.1371/journal.pone.0106816.
- Luizon M.R., Belo V.A., Fernandes K.S., Andrade V.L., Tanus-Santos J.E., Sandrim V.C. Plasma matrix metalloproteinase-9 levels, MMP-9 gene haplotypes, and cardiovascular risk in obese subjects. Mol. Biol. Rep. 2016;43(6):463-471. DOI: 10.1007/s11033-016-3993-z.
- DeLeon-Pennell K.Y., Meschiari C.A., Jung M., Lindsey M.L. Matrix metalloproteinases in myocardial infarction and heart failure. Prog. Mol. Biol. Transl. Sci. 2017;147:75-100. DOI: 10.1016/bs.pmbts.2017.02.001.
- Visse R., Nagase H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: Structure, function, and biochemistry. Circ. Res. 2003;92(8):827-839. DOI: 10.1161/01.RES.0000070112.80711.3D.
- Velho F.M., Cohen C.R., Santos K.G., Silvello D., Martinelli N., Biolo A. et al. Polymorphisms of matrix metalloproteinases in systolic heart failure: Role on disease susceptibility, phenotypic characteristics, and prognosis. J. Card. Fail. 2011;17(2):115-121. DOI: 10.1016/j.card-fail.2010.09.017.
- Martin T.N., Penney D.E., Smith J.A., Groenning B.A., Dargie H.J., Hillis G.S. Matrix metalloproteinase-1 promoter polymorphisms and changes in left ventricular volume following acute myocardial infarction. Am. J. Cardiol. 2004;94(8):1044-1046. DOI: 10.1016/j.amj-card.2004.06.064.
- Lindner D., Zietsch C., Becher P.M., Schulze K., Schultheiss H.P., Tschope C. et al. Differential expression of matrix metalloproteas-es in human fibroblasts with different origins. Biochem. Res. Int. 2012;2012:875742. DOI: 10.1155/2012/875742.
- Sage E.H., Reed M., Funk S.E., Truong T., Steadele M., Puolakkainen P. et al. Cleavage of the matricellular protein sparc by matrix metallopro-teinase 3 produces polypeptides that influence angiogenesis. J. Biol. Chem. 2003;278(39):37849-37857. DOI: 10.1074/jbc.M302946200.
- Mashhadiabbas F., Neamatzadeh H., Foroughi E., Dastgheib S.A., Farahnak S., Nasiri R. et al. Association of MMP-2-753C>T and MMP-9-1562C>T Polymorphisms with Chronic/Aggressive Periodontitis Risk: A Systematic Review and Meta-Analysis. Iran. J. Public. Health. 2019;48(7):1227-1238.
- Yabluchanskiy A., Ma Y., Iyer R.P., Hall M.E., Lindsey M.L. Matrix metal-loproteinase-9: Many shades of function in cardiovascular disease. Physiology. 2013;28(6):391-403. DOI: 10.1152/physiol.00029.2013.
- Blankenberg S., Rupprecht H.J., Poirier O., Bickel C., Smieja M., Hafner G. et al. Plasma concentrations and genetic variation of matrix metalloproteinase 9 and prognosis of patients with cardiovascular disease. Circulation. 2003;107(12):1579-1585. DOI: 10.1161/01. CIR.0000058700.41738.12.
- Dai H., Chen L., Gao D., Fei A. Phosphocreatine attenuates isoprotere-nol-induced cardiac fibrosis and cardiomyocyte apoptosis. Biomed. Res. Int. 2019;2019:5408289. DOI: 10.1155/2019/5408289.
- Squire I.B., Evans J., Ng L.L., Loftus I.M., Thompson M.M. Plasma mmp-9 and mmp-2 following acute myocardial infarction in man: Correlation with echocardiographic and neurohumoral parameters of left ventricular dysfunction. Journal of Cardiac Failure. 2004;10(4):328-333. DOI: 10.1016/j.cardfail.2003.11.003.
- Wang X., Shi L.Z. Association of matrix metalloproteinase-9 c1562t polymorphism and coronary artery disease: A meta-analysis. J. Zhejiang Univ. Sci. B. 2014;15(3):256-263. DOI: 10.1631/jzus.B1300088.
- Lacchini R., Metzger I.F., Luizon M., Ishizawa M., Tanus-Santos J.E. Interethnic differences in the distribution of matrix metalloproteinases genetic polymorphisms are consistent with interethnic differences in disease prevalence. DNA Cell Biol. 2010;29(11):649-655. DOI: 10.1089/ dna.2010.1056.
- Horwich T.B., Fonarow G.C. Glucose, obesity, metabolic syndrome, and diabetes relevance to Incidence of heart failure. J. Am. Coll. Cardiol. 2010;55(4):283-293. DOI: 10.1016/j.jacc.2009.07.029.
- Kremastiotis G., Handa I., Jackson C., George S., Johnson J. Disparate effects of MMP and TIMP modulation on coronary atherosclerosis and associated myocardial fibrosis. Sci. Rep. 2021;11(1):23081. DOI: 10.1038/s41598-021-02508-4.
- Mazuchova J., Halasova E., Mazuch J., Sarlinova M., Valentova V., Franekova M. et al. Investigation of Association between Genetic Polymorphisms of MMP2, MMP8, MMP9 and TIMP2 and Development of Varicose Veins in the Slovak Population - Pilot Study. Physiol. Res. 2020;69(3):S443-S454. DOI: 10.33549/physiolres.934597.
- Kandalam V., Basu R., Moore L., Fan D., Wang X., Jaworski D.M. et al. Lack of tissue inhibitor of metalloproteinases 2 leads to exacerbated left ventricular dysfunction and adverse extracellular matrix remodeling in response to biomechanical stress. Circulation. 2011;124(19):2094-2105. DOI: 10.1161/CIRCULATIONAHA.111.030338.
- Moore L., Fan D., Basu R., Kandalam V., Kassiri Z. Tissue inhibitor of metalloproteinases (TIMPs) in heart failure. Heart Fail. Rev. 2012;17(4-5):693-706. DOI: 10.1007/s10741-011-9266-y.
- Schanz M., Shi J., Wasser C., Alscher M.D., Kimmel M. Urinary [TIMP-2] x [IGFBP7] for risk prediction of acute kidney injury in decompensated heart failure. Clin. Cardiol. 2017;40:485-491. DOI: 10.1002/clc.22683.
- Fan D., Takawale A., Basu R., Patel V., Lee J., Kandalam V. et al. Differential role of TIMP2 and TIMP3 in cardiac hypertrophy, fibrosis, and diastolic dysfunction. Cardiovasc. Res. 2014;103(2):268-280. DOI: 10.1093/cvr/cvu072.
- Polina E.R., Araujo R.R.C.V., Sbruzzi R.C., Biolo A., Rohde L.E., Clausell N. et al. Relationship of polymorphisms in the tissue inhibitor of metalloproteinase (TIMP)-1 and -2 genes with chronic heart failure. Sci. Rep. 2018;8(1):9446. DOI: 10.1038/s41598-018-27857-5.
- Alp E., Yilmaz A., Tulmac M., Dikmen A.U., Cengel A., Yalcin R. et al. Analysis of MMP-7 and TIMP-2 gene polymorphisms in coronary artery disease and myocardial infarction: A Turkish case-control study. Kaohsi-ung J. Med. Sci. 2017;33(2):78-85. DOI: 10.1016/j.kjms.2016.12.002.
- Lin T.H., Chiu H.C., Lee Y.T., Su H.M., Juo S.H., Voon W.C. et al. The C-allele of tissue inhibitor of metalloproteinases 2 is associated with increased magnitude of QT dispersion prolongation in elderly Chinese -4-year follow-up study. Clin. Chim. Acta. 2007;386(1-2):87-93. DOI: 10.1016/j.cca.2007.08.004.
- Jia M., Li Z.B., Li L., Chu H.T., Li Z.Z. Role of matrix metalloproteinase-7 and apoptosis-associated gene expression levels in the pathogenesis of atrial fibrosis in a Beagle dog model. Mol. Med. Rep. 2017;16(5):6967-6973. DOI: 10.3892/mmr.2017.7415.
- Dong H., Dong S., Zhang L., Gao X., Lv G., Chen W. et al. MicroR-NA-214 exerts a Cardio-protective effect by inhibition of fibrosis. Anat. Rec. (Hoboken). 2016;299(10):1348-1357. DOI: 10.1002/ar.23396.
- Lu Y., Boer J.M.A., Barsova R.M., Favorova O., Goel A., Müller M. et al. TGFB1 genetic polymorphisms and coronary heart disease risk: A meta-analysis. BMC Med. Genet. 2012;13:39. DOI: 10.1186/1471-235013-39.
- Gichkun O.E., Shevchenko O.P., Kurabekova R.M., Mozheiko N.P., Shevchenko A.O. The rs1800470 polymorphism of the TGFB1 gene is associated with myocardial fibrosis in heart transplant recipients. Acta Naturae. 2021;13(4):42-46. DOI: 10.32607/actanaturae.11469.
- Shah R., Hurley C.K., Posch P.E. A molecular mechanism for the differential regulation of TGF-beta1 expression due to the common SNP -509C-T (c. -1347C>T). Hum. Genet. 2006;120(4):461-469. DOI: 10.1007/s00439-006-0194-1.
- Barsova R.M., Titov B.V., Matveeva N.A., Favorov A.V., Sukhinina T.S., Shahnovich R.M. et al. Contribution of the TGFB1 gene to myocardial infarction susceptibility. Acta Naturae. 2012;4(2):74-79.
- Брусенцов Д.А., Никулина С.Ю., Шестерня П.А., Чернова А.А. Ассоциация полиморфных вариантов RS1800470 гена трансформирующего ростового фактора ß1 (TGF-ß1) с тяжестью коронарного атеросклероза. Российский кардиологический журнал. 2018;(10):43-47. DOI: 10.15829/1560-4071-2018-10-43-47. Brusentsov D.A., Nikulina S.Yu., Shesternya P.A., Chernova A.A. Association of RS1800470 polymorphic variants of the transforming growth factor ß1 (TGF-ß1) gene with the severity of coronary atherosclerosis. Russian Journal of Cardiology. 2018;(10):43-47. (In Russ.). DOI: org/10.15829/1560-4071-2018-10-43-47.
- Crobu F., Palumbo L., Franco E., Bergerone S., Carturan S., Guarrera S. et al. Role of TGF-ß1 haplotypes in the occurrence of myocardial infarction in young Italian patients. BMC Med. Genet. 2008;9:13. DOI: 10.1186/1471-2350-9-13.
- Liu S., Ke W., Liu Y., Zhao Z., An L., You X. et al. Function analysis of differentially expressed microRNAs in TGF-ß1-induced cardiac fibroblasts differentiation. Biosci. Rep. 2019;39(10):BSR20182048. DOI: 10.1042/ BSR20182048.
- Cocciolone A.J., Hawes J.Z., Staiculescu M.C., Johnson E.O., Murshed M., Wagenseil J.E. Elastin, arterial mechanics, and cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 2018;315(2):H189-H205. DOI: 10.1152/ajpheart.00087.2018.
- Tassabehji M., Metcalfe K., Donnai D., Hurst J., Reardon W., Burch M. et al. Elastin: Genomic structure and point mutations in patients with su-pravalvular aortic stenosis. Hum. Mol. Genet. 1997;6:1029-1036. DOI: 10.1093/hmg/6.7.1029.
- Li S.H., Sun Z., Guo L., Han M., Wood M.F., Ghosh N. et al. Elastin overexpression by cell-based gene therapy preserves matrix and prevents cardiac dilation. J. Cell Mol. Med. 2012;16(10):2429-2439. DOI: 10.1111/j.1582-4934.2012.01560.x.