Осложнения со стороны сердечно-сосудистой системы при респираторных вирусных инфекциях
Автор: Ишмурзин Г. П., Серебрякова О. А., Сюзев К. Н., Долганова Д. А., Гайнуллина А. Х.
Журнал: Сибирский журнал клинической и экспериментальной медицины @cardiotomsk
Рубрика: Обзоры и лекции
Статья в выпуске: 4 т.37, 2022 года.
Бесплатный доступ
Несмотря на значительный прогресс в понимании патогенеза вирусных болезней и способов их лечения, один только вирус гриппа вызывает до 35 млн тяжелых случаев заболевания и 250-500 тыс. смертей ежегодно. Однако респираторные вирусы способны влиять не только на дыхательную систему, но и в том числе вызывать осложнения со стороны сердечно-сосудистой системы (ССС), такие как: острый коронарный синдром (ОКС), миокардиты и перикардиты, обострение хронической сердечной недостаточности (ХСН), острая сердечная недостаточность, тромбоэмболия легочной артерии и аритмии. В данном обзоре представлена информация о частоте встречаемости сердечно-сосудистых осложнений, возникших в ассоциации с перенесенными острыми респираторными вирусными инфекциями (новая коронавирусная инфекция, грипп, РС-инфекция, аденои риновирусные инфекции), механизмах влияния респираторных вирусов на ССС. Понимание данных механизмов позволит предвидеть возможные сердечнососудистые осложнения у пациентов с респираторными инфекциями, как можно раньше предпринять меры для быстрого их купирования, особенно при жизнеугрожающих состояниях.
Факторы риска сердечно-сосудистых заболеваний, covid-19, грипп, рс-вирус
Короткий адрес: https://sciup.org/149141451
IDR: 149141451 | УДК: 616.1-06:616.2-022.6 | DOI: 10.29001/2073-8552-2022-37-4-31-37
Текст научной статьи Осложнения со стороны сердечно-сосудистой системы при респираторных вирусных инфекциях
Ишмурзин Г.П., Серебрякова О.А., Сюзев К.Н., Долганова Д.А., Гайнуллина А.Х. Осложнения со стороны сердечно-сосудистой системы при респираторных вирусных инфекциях. Сибирский журнал клинической и экспериментальной медицины. 2022;37(4):31–37.
Несмотря на значительный прогресс в понимании патогенеза вирусных болезней и способов их лечения, вирус SARS-CoV-2 привел к 370 тыс. смертей из 18 млн случаев заболеваний в России с начала пандемии, в то время как различные штаммы вируса гриппа (А, В, С) вызывают до 3–5 млн тяжелых случаев заболевания и 250–500 тыс. смертей ежегодно.
Известные «традиционные» факторы риска сердечно-сосудистых заболеваний (ССЗ), такие как гипертония, курение, диабет и ожирение, уже не раз рассматривались в глобальных эпидемиологических исследованиях и становились темами многочисленных литературных обзоров [1]. Некоторые исследования дополнительно рассматривают взаимосвязь развития ССЗ и таких факторов, как эмоциональный стресс и загрязнение воздуха [2]. Острые респираторные инфекции, включая вирусы SARS-CoV-2, гриппа и респираторно-синцитиальный (РС) вирус, способны влиять не только на дыхательную систему, но и вызывать осложнения со стороны ССС, в том числе: острый коронарный синдром, миокардиты и перикардиты, обострение хронической сердечной недостаточности, острую сердечную недостаточность, тромбоэмболию легочной артерии и нарушения ритма. Однако их влияние на возникновение ССЗ и течение уже имеющихся сопутствующих ССЗ недостаточно раскрываются в исследованиях [3].
В данном обзоре мы приводим данные о частоте встречаемости сердечно-сосудистых осложнений, возникших в ассоциации с перенесенными острыми респираторными вирусными инфекциями (новая коронавирусная инфекция, грипп, РС-инфекция, адено- и риновирусные инфекции), а также описываем основные патофизиологические механизмы, лежащие в основе возникновения данных осложнений.
SARS-CoV-2
SARS-CoV-2 – респираторный вирус, передающийся воздушно-капельным, аэрозольным и контактным путями. С начала пандемии в России было зарегистрировано 18 млн случаев новой коронавирусной инфекции (SARS-CoV-2), из них 373 тыс. случаев летального исхода, смертность от SARS-CoV-2 составила 2%. ССЗ как непосредственная причина смерти у пациентов с новой коронавирусной инфекцией выявляются в 7% случаев, а наличие сопутствующих ССЗ увеличивает смертность в 10 раз [4, 5].
Вирус SARS-CoV-2 способен вызывать такие ССЗ, как миокардит, нарушения ритма сердца, острый коронарный синдром и тромбоэмболии различной локализации. Были описаны клинические случаи манифестации SARS-CoV-2 именно с симптомов поражения ССС. Также для детей характерно поражение сосудов, проявляющееся в виде синдрома Кавасаки. Частота встречаемости различных осложнений со стороны ССС представлена в таблице.
Анализ литературы показал, что сердечно-сосудистые осложнения возникают в 2–10 раз чаще у пациентов, находящихся в тяжелом состоянии на искусственной вентиляции легких. Наиболее частыми осложнениями являются нарушения ритма сердца. При SARS-CoV-2 возможно развитие как тахи-, так и брадиаритмий. Наиболее часто развивается фибрилляция предсердий, реже встречаются желудочковые экстрасистолии и пароксизмальные наджелудочковые тахикардии. Гипоксия и электролитные нарушения, развивающиеся из-за поражения легких, развития острого респираторного дистресс-синдрома, предрасполагают к развитию аритмий [6]. Другими частыми осложнениями SARS-CoV-2 являются тромботические осложнения вен любых локализаций, в частности тромбоэмболия легочной артерии (ТЭЛА). В проспективном когортном исследовании аутопсийного материала у 4 из 12 (34%) пациентов причиной смерти явилась ТЭЛА, у 7 из 12 (58%) был обнаружен тромбоз глубоких вен (ТГВ), не диагностированный при жизни [7]. Тромбоз также может приводить к острой артериальной недостаточности [8]. Сравнительно более редким осложнением является острый коронарный синдром (ОКС). Проявления ОКС могут варьировать от подъема сегмента ST до острого инфаркта миокарда и могут быть первыми симптомами коронавирусной инфекции [9].
Несмотря на весь спектр сердечно-сосудистых осложнений, возникающих после SARS-CoV-2, есть основания полагать, что в ряде случаев повреждение миокарда проходит или бессимптомно или остается не диагностированным. Так, при комплексном обследовании 1597 спортсменов после перенесенной SARS-CoV-2 частота клинически выраженного миокардита составила 0,31%, после проведения МРТ-диагностики сердца частота миокардита увеличилась в 7,4 раза [10]. Около 78% пациентов, перенесших SARS-CoV-2 не менее чем 2 нед. назад, получивших отрицательный результат на наличие вируса SARS-CoV-2 и не имеющих респираторных симптомов, имели различные изменения на МРТ сердца, в том числе позднее накопление гадолиния и выпот в полости перикарда [11].
Предполагаемые механизмы поражения ССС при SARS-CoV-2 включают прямую клеточную цитотоксичность, повреждение эндотелия и его последующего тромбогенного состояния, нарушение регуляции ренин-анги-отензин-альдостероновой системы (РААС) и нарушение регуляции иммунного ответа. Роль каждого механизма в патофизиологии возникновения поражения ССС при SARS-CoV-2 до сих пор полностью не определена.
Прямое влияние вируса SARS-CoV-2 на ССС обусловлено тропностью вируса, которая реализуется за счет связывания вирусного S-белка с рецепторами ангио-тензин-превращающего фермента 2 (АПФ2), высоко экспрессирующимися на поверхности пневмоцитов II типа, а также энтероцитов тонкого кишечника, кардиомиоцитов и эндотелиальных клеток артерий и вен (рис. 1).
Таблица. Частота встречаемости сердечно-сосудистых осложнений у больных COVID-19 по данным разных исследований (в скобках указано количество человек с тяжелой степенью COVID-19, потребовавшей перевода в отделение реанимации)
Table. The incidence of cardiovascular complications in patients with COVID-19 according to different studies (numbers in parentheses indicate the number of people with severe COVID-19 who required transfer to the intensive care unit)
|
Автор, год Author, year |
Страна Country |
Количество человек Number of people |
Миокардит, % Myocarditis, % |
НРС, % Arrythmias, % |
ТЭЛА, % PTE, % |
ОКС, % ACS, % |
СН, % HF, % |
|
T. Guo, 2020 [12] |
Китай China |
184 |
– |
– |
– |
11,2% (–) |
– |
|
Fei Zhou, 2020 [13] |
Китай China |
191 |
– |
– |
– |
1% (59%) |
12% (52%) |
|
P. Goyal, 2020 [14] |
США U.S.A. |
393 |
– |
1,9% (18,5%) |
– |
11% (19,2%) |
– |
|
B.J.R. Buckley, 2021 [15] |
США U.S.A. |
718 365 |
5% (–) |
– |
– |
– |
– |
|
J. Pillarisetti, 2022 [16] |
США U.S.A. |
81 844 |
– |
6,97% (-) |
– |
1,34% (–) |
4,4% (–) |
|
D. Wang, 2020 [17] |
Китай China |
138 |
2% (22,2%) |
6.9% (44,4%) |
– |
– |
– |
|
Q. Deng, 2020 [18] |
Китай China |
112 |
12,5% (–) |
– |
– |
0,7% (–) |
– |
|
B. Malas, 2020 [19] |
США U.S.A. |
8271 |
– |
– |
13% (19%) |
– |
– |
|
А. Kollias, 2021 [20] |
Греция Greece |
3973 |
– |
– |
32% (-) |
– |
– |
Примечание: НРС – нарушение ритма сердца, ТЭЛА – тромбоэмболия легочной артерии, ОКС – острый коронарный синдром, СН – сердечная недостаточность.
Note: PTE – pulmonary thromboembolism, ACS – acute coronary syndrome, HF – heart failure.
Тонкий кишечник Small intestine
Сердце – левый желудочек Heart: left ventricle
Сердце – Коронарные предсердия артерии Heart: atria Coronary arteries
Легкие Lungs
Кожа Skin
Аорта Aorta
Клетки крови Blood cells
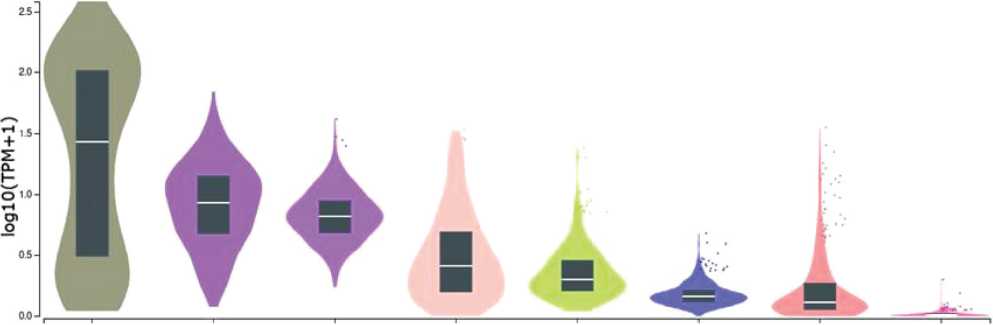
Рис. 1. Распределение экспрессии гена, кодирующего рецептор АПФ2, с которым взаимодействует вирус SARS-CoV-2 в разных тканях. Рисунок создан при помощи портала Genotype-Tissue Expression (GTEx)
Fig. 1. Distribution of expression for the gene encoding the ACE2 receptor SARS-CoV-2 virus interacts in different tissues. Figure created using the Genotype-Tissue Expression Portal (GTEx)
Активация вирусного S-белка опосредуется чаще всего трансмембранной сериновой протеазой 2 (TSP2), хотя возможно взаимодействие с другими протеазами, например, в кардиомиоцитах, поскольку экспрессия TSP2 там минимальна [21].
Тропизм вируса к кардиомиоцитам подтверждается как in vitro, так и in vivo. Исследования, проведенные на клеточных линиях плюрипотентных кардиомиоцитов, полученных из стволовых клеток, показывают, что SARS-CoV-2 способен непосредственно инфицировать кардиомиоциты через рецептор АПФ2. Наличие активированной каспазы-3 в культуре клеток свидетельствовало о ви-рус-индуцированном апоптозе. Сократительная активность кардиомиоцитов прекращалась через 72 ч после инфицирования [22]. In vivo тропизм вируса к сердечной ткани подтверждается многочисленными исследованиями, обнаруживающими вирус SARS-CoV-2 в аутопсии сердечной ткани пациентов, умерших от новой коронавирусной инфекции. В некоторых случаях миокардит устанавливался только посмертно. Обнаруживались также артериит, тромбоваскулит, перикардит и эндокардит [23, 24]. Еще одним доказательством прямого цитопатическо- го действия SARS-CoV-2 является обнаружение вирусных частиц в кардиомиоцитах и клетках эндокарда при помощи электронной микроскопии [25, 26].
Кроме того, в настоящее время представлено множество теорий непрямого поражения миокарда, каждая из которых имеет свою доказательную базу. Повреждение миокарда возможно из-за гипоксии и нарушения соотношения между потребностями миокарда и его снабжением кислородом. Другим фактором, вызывающим повреждение миокарда, является цитокиновый шторм. Проникнув в клетку, вирус начинает реплицироваться и продуцировать множество вирусных нуклеокапсидов, а нагруженные вирусными частицами клетки высвобождают множество различных цитокинов: интерлейкины (ИЛ-1, ИЛ-6, ИЛ-8, ИЛ-120 и ИЛ-12), фактор некроза опухоли α (ФНО-α), интерфероны (ИФН), CXCL-10, хемоаттрактантный белок моноцитов 1 (MCP-1) и воспалительный белок макрофагов 1α (MIP-1α). Цитокины служат хемоаттрактантами для нейтрофилов, CD4 и CD8 Т-клеток, которые, активируясь, опосредуют повреждение окружающих клеток.
Гиперпродукция цитокинов приводит к кратковременному положительному инотропному эффекту, сменяю-щимуся отрицательным инотропным эффектом за счет стимулирования цитокинами синтеза NO-синтазы, увеличения активных форм кислорода, десенситизации бета-адренорецепторов. NO-синтаза дополнительно активирует с помощью цГМФ протеинкиназу и фософодиэстеразу II, которые, в свою очередь, дополнительно участвуют в снижении чувствительности бета-адренорецепторов и фосфорилировании тропонина I, что также дополнительно снижает чувствительность миофиламентов к ионам Ca [27]. Еще одним механизмом сердечно-сосудистых осложнений является массивное тромбообразование, характерное для SARS-CoV-2. За любым повреждением эндотелия следует дегрануляция телец Вайбеля – Пала-де и высвобождение из них фактора фон Виллебранда с последующим тромбообразованием. Тромботические осложнения при новой коронавирусной инфекции встречаются гораздо чаще, чем при других респираторных инфекциях, однако причина этого достоверно неизвестна. Аритмогенное действие вируса обусловливается способностью вируса образовывать белки виропорины, которые встраиваются в клетку хозяина и служат ионным каналом, способствуя утечке иона К+ из клетки, развитию гипокалиемии и нарушению формирования потенциала действия кардиомиоцитов. Виропоринами могут служить оболочечный белок Е, а также белки 3а, 4а и 8а SARS-CoV-2 [28]. К изменению длительности потенциала действия и развитию аритмий приводит и гипоксия за счет снижения pH и увеличения уровня внеклеточного калия, и системное воспаление за счет влияния провоспалитель-ных цитокинов на ионные каналы.
Грипп
По данным центра по контролю и профилактике заболеваний США, ежегодно гриппом заболевают от 9 до 41 млн человек, приводя к смерти 12–54 тыс. человек ежегодно. Таким образом, смертность при гриппе варьирует от 0,1 до 1%. Вирус гриппа также способен оказывать патогенное действие на ССС. Пандемия гриппа A (H1N1) 2009 г. стала причиной 201 200 смертей от респираторных заболеваний во всем мире, причем еще 83 300 смертей (41%) были связаны с сердечно-сосудистыми осложнениями. 83% этих смертельных случаев приходится на людей старше 65 лет. Исследования подтверждают значительный рост смертности, связанной с ССЗ, у инфицированных вирусом гриппа. Например, в исследовании J.C. Kwong и соавт. коэффициенты заболеваемости острым инфарктом миокарда в течение 7 дней после обнаружения гриппа В и гриппа А составили 10,11 и 5,17 соответственно [29, 30].
Анализ смертности за 40 лет с 1959 по 1999 гг. также показал, что пики ишемической болезни сердца и цереброваскулярной болезни совпадали с пиками пневмонии и гриппа [31]. Наибольшему риску смерти от сердечно-сосудистых явлений, связанных с перенесенной инфекцией гриппа, подвержены люди в возрасте старше 65 лет. Риск также оказался выше после перенесенного штамма В по сравнению со штаммами гриппа А (H1N1, H3N2) [32].
Многочисленные серии клинических случаев сообщают о миокардите, ассоциированном с гриппом, с частотой встречаемости до 10%. Средний возраст больных составляет 30–33 года, сообщается также о случаях миокардита у детей. Более чем в половине случаев наблюдалось фульминантное течение, в ряде случаев осложненное кардиогенным шоком, смертность в среднем составляет 14–27% [33–36].
Инфицирование вирусом гриппа А также может осложняться нарушениями ритма. В отличие от вируса SARS-CoV-2, который наиболее часто вызывает наджелудочковые нарушения ритма, у инфицированных вирусом гриппа чаще встречаются желудочковые нарушения ритма и полная атриовентрикулярная блокада, которые чаще всего являются осложнением фульминантного миокардита [37–40]. Перикардит также может являться осложнением гриппа в среднем в 1–7% случаев и способен возникать как самостоятельно, так и в виде осложнения миокардита, то есть в виде миоперикардита [41].
Механизм, лежащий в основе возникновения сердечно-сосудистых осложнений при гриппе, может быть схож с таковым при SARS-CoV-2: возникновение дисфункции эндотелия и его тромбогенного состояния. Исследования на животных моделях доказывают склонность к повышенной коагуляции и формированию тромбов у животных, инфицированных вирусом гриппа. Однако склонность к коагуляции ниже, чем при инфицировании вирусом SARS-CoV-2, фактор фон Виллебранда при гриппе повышается в среднем на 123–211% от нормы, при SARS-CoV-2 – до 565% у пациентов с тяжелой вирусной пневмонией [42, 43].
Теоретически возможно прямое воздействие вируса на кардиомиоциты. Вирусная РНК, также как и при SARS-CoV-2, обнаруживается в аутопсийном материале миокарда людей, умерших от осложнений вируса гриппа [41].
Однако есть ряд особенностей, о которых необходимо упомянуть. Вирус гриппа способен усугублять течение атеросклероза и приводить к нестабильности атеросклеротических бляшек, тем самым увеличивая риск ОКС, несколькими механизмами. Во-первых, за счет усиления, индуцируемого окисленным липопротеином низкой плотности (ox-LDL), апоптоза эндотелиоцитов через активации передачи сигналов р53 [44]. Во-вторых, вирус гриппа усиливает экспрессию матриксных металлопротеаз в атеросклеротических бляшках, которые, в свою очередь, разрушая внеклеточный матрикс, делают атеросклеротические бляшки нестабильными.
Вакцинация от гриппа снижает вероятность госпитализации по поводу СН у пожилых пациентов с хронической болезнью почек, а также снижает риск ОКС у пожилых пациентов с хронической обструктивной болезнью легких (ХОБЛ) [45, 46]. А метаанализ показывает, что вакцинация от гриппа снижает смертность от всех причин на 25% [47].
Другие вирусы
Потенциально опасным этиологическим триггером миокардита и кардиомиопатии является аденовирус. Он имеет общий с кардиотропным вирусом Коксаки рецептор (Coxsackievirus and adenovirus receptor, CAR), связываясь с которым, аденовирус способен проникать в кардиомиоциты, реплицироваться в них и, в конечном итоге, вызывать лизис клеток. При исследовании биопсийного материала 624 пациентов с диагнозом «острый миокардит» ДНК аденовируса обнаруживался в 23% случаев. Среди 149 биопсийных материалов пациентов с диагнозом «дилатационная кардиомиопатия» аденовирус выявлялся у 14% пациентов.
Другим этиологическим триггером, вызывающим острые респираторные вирусные инфекции (ОРВИ), является РС вирус, представляющий наибольшую опасность для детей до 2 лет и пожилых людей. Наличие сопутствующих ССЗ является фактором риска для РС инфекции у пожилых людей. Частота сопутствующих ССЗ у госпитализированных по поводу РС инфекции достигает 52%, в том числе частота ХСН 21%, ишемическая болезнь сердца, по разным данным, – от 28 до 43% [48–50]. Частота сердечно-сосудистых осложнений РС инфекции – от 14 до 24,6%, чаще всего обнаруживалась декомпенсация ХСН, острый инфаркт миокарда и впервые возникшая фибрилляция предсердий [48, 51, 52]. Вероятно, сердечно-сосудистые осложнения возникают за счет непрямого воздействия вируса, а именно перенапряжения правого желудочка при легочной гипертензии, воздействия провоспалительных цитокинов и свободных радикалов на эндотелий.
Самой частой причиной сезонной ОРВИ является ри-новирус. Нет достаточных данных о сердечно-сосудистых осложнений, связанных с риновирусной инфекцией, существуют только единичные клинические случаи, сообщающие о развитии миокардита и дальнейшем развитии кардиомиопатии. Этиологическая роль риновируса в развитии миокардита в клинических случаях предполагалась на основании ПЦР тестирования. Существенным ограничением исследования является отсутствие результатов эндомиокардиальной биопсии [53, 54].
Также единичные клинические случаи развития миокардита представляются в отношении парагриппа и метапневмовируса [55, 56].
Заключение
Многочисленные исследования показывают, что наибольшую опасность для ССС представляют вирусы SARS-CoV-2 и вирус гриппа. Острые респираторные инфекции разделяют некоторые общие универсальные механизмы поражения ССС, которые включают в себя гипоксию, системное воспаление и перенапряжение правого желудочка при легочной гипертензии. Однако отдельные особенные для определенных вирусов механизмы, по всей видимости, обеспечивают отличия в спектре и частоте сердечно-сосудистых осложнений.
Список литературы Осложнения со стороны сердечно-сосудистой системы при респираторных вирусных инфекциях
- Flora G.D., Nayak M.K. A Brief review of cardiovascular diseases, associated risk factors and current treatment regimes. Curr. Pharm. Des. 2019;25(38):4063-4084. DOI: 10.2174/1381612825666190925 163827.
- Khayyam-Nekouei Z., Neshatdoost H., Yousefy A., Sadeghi M., Man-shaee G. Psychological factors and coronary heart disease. ARYA Ath-eroscler. 2013;9(1):102-111.
- Dhainaut J.-F., Claessens Y.-E., Janes J., Nelson D.R. Underlying disorders and their impact on the host response to infection. Clin. Infect. Dis. 2005;41(7):S481-S489. DOI: 10.1086/432001.
- Elezkurtaj S., Greuel S., Ihlow J., Michaelis E. G., Bischoff P., Kunze C.A. et al. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci. Rep. 2021;11(1):4263. DOI: 10.1038/s41598-021-82862-5.
- Ketcham S.W., Bolig T.C., Molling D.J., Sjoding M.W., Flanders S.A., Prescott H.C. Causes and Circumstances of Death among Patients Hospitalized with COVID-19: A Retrospective Cohort Study. Ann. A. Thorac. Soc. 2021;18(6):1076-1079. DOI: 10.1513/Annal-sATS.202011-1381RL.
- Gopinathannair R., Merchant F.M., Lakkireddy D.R., Etheridge S.P., Feigofsky S., Han J.K. et al. COVID-19 and cardiac arrhythmias: A global perspective on arrhythmia characteristics and management strategies. J. Interv. Card. Electrophysiol. 2020;59(2):329-336. DOI: 10.1007/ s10840-020-00789-9.
- Wichmann D., Sperhake J.P., Lütgehetmann M., Steurer S., Edler C., Heinemann A. et al. Autopsy Findings and Venous Thromboembolism in Patients with COVID-19: A Prospective Cohort Study. Ann. Intern. Med. 2020;173(4):268-277. DOI: 10.7326/M20-2003.
- Bellosta R., Luzzani L., Natalini G., Pegorer M.A., Attisani L., Cossu L.G. et al. Acute limb ischemia in patients with COVID-19 pneumonia. J. Vasc. Surg. 2020;72(6):1864-1872. DOI: 10.1016/j.jvs.2020.04.483.
- Stefanini G.G., Montorfano M., Trabattoni D., Andreini D., Ferrante G., Ancona M. et al. ST-Elevation Myocardial infarction in patients with COVID-19: Clinical and angiographic outcomes. Circulation. 2020;141(25):2113—2116. DOI: 10.1161/CIRCULATIONA-HA.120.047525.
- Daniels C.J., Rajpal S., Greenshields J.T., Rosenthal G. L., Chung E.H., Terrin M. et al. Prevalence of clinical and subclinical myocarditis in competitive athletes with recent SARS-CoV-2 Infection: Results from the big ten COVID-19 cardiac registry. JAMA Cardiol. 2021;6(9):1078-1087. DOI: 10.1001/jamacardio.2021.2065.
- Puntmann V.O., Carerj M.L., Wieters I., Fahim M., Arendt C., Hoffmann J. et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265-1273. DOI: 10.1001/ja-macardio.2020.3557.
- Guo T., Fan Y., Chen M., Wu X., Zhang L., He T. et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811-818. DOI: 10.1001/jamacar-dio.2020.1017.
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395(10229):1054-1062. DOI: 10.1016/S0140-6736(20)30566-3.
- Goyal P., Choi J.J., Pinheiro L.C., Schenck E. J., Chen R., Jabri A. et al. Clinical characteristics of COVID-19 in New York City. N. Engl. J. Med. 2020;382(24):2372-2374. DOI: 10.1056/NEJMc2010419.
- Buckley B.J.R., Harrison S.L., Fazio-Eynullayeva E., Underhill P., Lane D.A., Lip G.Y.H. Prevalence and clinical outcomes of myocarditis and pericarditis in 718,365 COVID-19 patients. Eur. J. Clin. Invest. 2021;51(11):e13679. DOI: 10.1111/eci.13679.
- Pillarisetti J., Cheema M.S., Haloot J., Panday M., Badin A., Mehta A. et al. Cardiac complications of COVID-19: Incidence and outcomes. Indian. Heart J. 2022;74(3):170-177. DOI: 10.1016/j.ihj.2022.04.008.
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. DOI: 10.1001/jama.2020.1585.
- Deng Q., Hu B., Zhang Y., Wang H., Zhou X., Hu W. et al. Suspected myocardial injury in patients with COVID-19: Evidence from front-line clinical observation in Wuhan, China. Int. J. Cardiol. 2020;311:116-121. DOI: 10.1016/j.ijcard.2020.03.087.
- Malas M.B., Naazie I.N., Elsayed N., Mathlouthi A., Marmor R., Clary B. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: A systematic review and meta-analysis. EClinicalMedi-cine. 2020;29:100639. DOI: 10.1016/j.eclinm.2020.100639.
- Kollias A., Kyriakoulis K.G., Lagou S., Kontopantelis E., Stergiou G.S., Syrigos K. Venous thromboembolism in COVID-19: A systematic review and meta-analysis. Vasc. Med. 2021;26(4):415-425. DOI: 10.1177/1358863X21995566.
- Bristow M.R., Zisman L.S., Altman N.L., Gilbert E.M., Lowes B.D., Mi-nobe A. et al. Dynamic regulation of SARS-Cov-2 binding and cell entry mechanisms in remodeled human ventricular myocardium. JACC Basic. Transl. Sci. 2020;5(9):871-883. DOI: 10.1016/j.jacbts.2020.06.007.
- Sharma A., Garcia G. Jr., Wang Y., Plummer J. T., Morizono K., Arumu-gaswami V. et al. Human iPSC-derived cardiomyocytes are susceptible to SARS-CoV-2 infection. Cell Rep. Med. 2020;1(4):100052. DOI: 10.1016/j.xcrm.2020.100052.
- Lindner D., Fitzek A., Brauninger H., Aleshcheva G., Edler C., Meissner K. et al. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. 2020;5(11):1281-1285. DOI:10.1001/jamacardio.2020.3551.
- Kogan E., Berezovskiy Y., Blagova O., Kukleva A., Semyonova L., Gretsov E. et al. Morphologically, immunohistochemically and PCR proven lymphocytic viral peri-, endo-, myocarditis in patients with fatal COVID-19. Diagn. Pathol. 2022;17(1):31. DOI: 10.1186/s13000-022-01207-6.
- Basso C., Leone O., Rizzo S., De Gaspari M., van der Wal A.C., Aub-ry M.C. et al. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur. Heart J. 2020;41(39):3827-3835. DOI: 10.1093/eurheartj/ehaa664.
- Dolhnikoff M., Ferreira Ferranti J., de Almeida Monteiro R.A., Duarte-Neto A.N., Soares Gomes-Gouvea M., Viu Degaspare N. et al. SARS-CoV-2 in cardiac tissue of a child with COVID-19-related multisystem inflammatory syndrome. Lancet ChildAdolesc. Health. 2020;4(10):790-794. DOI: 10.1016/S2352-4642(20)30257-1.
- Prabhu S.D. Cytokine-induced modulation of cardiac function. Circ. Res. 2004;95(12):1140-1153. DOI: 10.1161/01.RES.0000150734.79804.92.
- McClenaghan C., Hanson A., Lee S.J., Nichols C.G. Coronavirus proteins as ion channels: Current and potential research. Front. Immunol. 2020;11:573339. DOI: 10.3389/fimmu.2020.573339.
- Kwong J.C., Schwartz K.L., Campitelli M.A., Chung H., Crowcroft N.S., Karnauchow T. et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N. Engl. J. Med. 2018;378(4):345-353. DOI: 10.1056/NEJMoa1702090.
- Nguyen J.L., Yang W., Ito K., Matte T.D., Shaman J., Kinney P.L. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. 2016;1(3):274-281. DOI: 10.1001/jamacardio.2016.0433.
- Reichert T.A., Simonsen L., Sharma A., Pardo S.A., Fedson D.S., Miller M.A. Influenza and the winter increase in mortality in the United States, 1959-1999. Am. J. Epidemiol. 2004;160(5):492-502. DOI:10.1093/aje/ kwh227.
- Qi L., Li Q., Ding X.B., Gao Y., Ling H., Liu T. et al. Mortality burden from seasonal influenza in Chongqing, China, 2012-2018. Hum. Vaccin. Immu-nother. 2020;16(7):1668-1674. DOI: 10.1080/21645515.2019.1693721.
- Kumar K., Guirgis M., Zieroth S., Lo E., Menkis A.H., Arora R.C. et al. Influenza myocarditis and myositis: case presentation and review of the literature. Can. J. Cardiol. 2011;27(4):514-522. DOI: 10.1016/j. cjca.2011.03.005.
- Ukimura A., Satomi H., Ooi Y., Kanzaki Y. Myocarditis Associated with Influenza A H1N1pdm2009. Influenza Res. Treat. 2012;2012:351979. DOI: 10.1155/2012/351979.
- Dolader P., Balcells J., Gran F. Influenza myocarditis in paediatric patients. Cardiol. Young. 2021;1-3. DOI: 10.1017/S1047951121004777.
- Purdy A., Ido F., Sterner S., Tesoriero E., Matthews T., Singh A. Myocarditis in COVID-19 presenting with cardiogenic shock: A case series. Eur. Heart J. Case Rep. 2021;5(2):ytab028. DOI: 10.1093/ehjcr/ytab028.
- Madjid M., Connolly A.T., Nabutovsky Y., Safavi-Naeini P., Razavi M., Miller C.C. Effect of high influenza activity on risk of ventricular arrhythmias requiring therapy in patients with implantable cardiac defibrillators and cardiac resynchronization therapy defibrillators. Am. J. Cardiol. 2019;124(1):44-50. DOI: 10.1016/j.amjcard.2019.04.011.
- Cheng W.L., Lin C.S. Transient atrioventricular block as a complication of influenza a virus: A case report. J. Acute Med. 2021;11(3):102-104. DOI: 10.6705/jjacme.202109_11(3).0004.
- Rivera-Guzmán N., Del Olmo-Arroyo F., Robles-Arías C.M., Rodrí-guez-Cintrón W. Transient AV block as a hemodynamic complication of the influenza a virus: A case report. P.R. Health Sci. J. 2016;35(3):173-175.
- Beinart R., Morganti K., Ruskin J., Mela T. H1N1 influenza A virus induced atrioventricular block. J. Cardiovasc. Electrophysiol. 2011;22(6):711-713. DOI: 10.1111/j.1540-8167.2010.01931.x.
- Estabragh Z.R., Mamas M.A. The cardiovascular manifestations of influenza: a systematic review. Int. J. Cardiol. 2013;167(6):2397-2403. DOI: 10.1016/j.ijcard.2013.01.274.
- Goshua G., Pine A.B., Meizlish M.L., Chang C.H., Zhang H., Bahel P. et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7(8):e575-e582. DOI: 10.1016/S2352-3026(20)30216-7.
- Van Wissen M., Keller T.T., van Gorp E.C., Gerdes V.E., Meijers J.C., van Doornum G.J. et al. Acute respiratory tract infection leads to procoagulant changes in human subjects. J. Thromb. Haemost. 2011;9(7):1432-1434. DOI: 10.1111/j.1538-7836.2011.04340.x
- Suo J., Zhao L., Wang J., Zhu Z., Zhang H., Gao R. Influenza virus aggravates the ox-LDL-induced apoptosis of human endothelial cells via promoting p53 signaling. J. Med. Virol. 2015;87(7):1113-1123. DOI: 10.1002/jmv.24166.
- Fang Y.A., Chen C.I., Liu J.C., Sung L.C. Influenza vaccination reduces hospitalization for heart failure in elderly patients with chronic kidney disease: A population-based cohort study. Acta Cardiol. Sin. 2016;32(3):290-298. DOI: 10.6515/acs20150424l.
- Sung L.C., Chen C.I., Fang Y.A., Lai C.H., Hsu Y.P., Cheng T.H. et al. Influenza vaccination reduces hospitalization for acute coronary syndrome in elderly patients with chronic obstructive pulmonary disease: A population-based cohort study. Vaccine. 2014;32(30):3843-3849. DOI: 10.1016/j.vaccine.2014.04.064.
- Yedlapati S.H., Khan S.U., Talluri S., Lone A.N., Khan M.Z., Khan M.S. et al. Effects of influenza vaccine on mortality and cardiovascular outcomes in patients with cardiovascular disease: A systematic review and meta-analysis. J. Am. Heart Assoc. 2021;10(6):e019636. DOI: 10.1161/ JAHA.120.019636.
- Volling C., Hassan K., Mazzulli T., Green K., Al-Den A., Hunter P. et al. Respiratory syncytial virus infection-associated hospitalization in adults: A retrospective cohort study. BMC Infect. Dis. 2014;14:665. DOI: 10.1186/s12879-014-0665-2.
- Walsh E.E., Peterson D.R., Falsey A.R. Risk factors for severe respiratory syncytial virus infection in elderly persons. J. Infect. Dis. 2004;189(2):233-238. DOI: 10.1086/380907.
- Dowell S.F., Anderson L.J., Gary H.E. Jr., Erdman D.D., Plouffe J.F., File T.M. et al. Respiratory syncytial virus is an important cause of community-acquired lower respiratory infection among hospitalized adults. J. Infect. Dis. 1996;174(3):456-462. DOI: 10.1093/infdis/174.3.456.
- Chuaychoo B., Ngamwongwan S., Kaewnaphan B., Athipanyasilp N., Horthongkham N., Kantakamalakul W. et al. Clinical manifestations and outcomes of respiratory syncytial virus infection in adult hospitalized patients. J. Clin. Virol. 2019;117:103-108. DOI: 10.1016/j.jcv.2019.07.001.
- Lee N., Lui G.C., Wong K.T., Li T.C., Tse E.C., Chan J.Y. et al. High morbidity and mortality in adults hospitalized for respiratory syncytial virus infections. Clin. Infect. Dis. 2013;57(8):1069-1077. DOI: 10.1093/cid/ cit471.
- Cebeci B., Oguz D., Ataoglu E., Elevli M., Yolcu C. Rhinovirus as a rare cause of acute onset dilated cardiomyopathy due to myocarditis in a newborn: case report and review of the literature. Turk. J. Pediatr. 2022;64(1):142-146. DOI: 10.24953/turkjped.2020.3664.
- Chow J., Murphy J., Subedi A., Jyothidasan A. Rhinovirus-associated dilated cardiomyopathy. IDCases. 2020;19:e00702. DOI: 10.1016/j. idcr.2020.e00702.
- Choi M.J., Song J.Y., Yang T.U., Jeon J.H., Noh J.Y., Hong K.W. et al. Acute myopericarditis caused by human Metapneumovirus. Infect. Chemother. 2016;48(1):36-40. DOI: 10.3947/ic.2016.48.1.36.
- Romero-Gómez M.P., Guereta L., Pareja-Grande J., Martínez-Alarcón J., Casas I., Ruiz-Carrascoso G. et al. Myocarditis caused by human parainfluenza virus in an immunocompetent child initially associated with 2009 influenza A (H1N1) virus. J. Clin. Microbiol. 2011;49(5):2072-2073. DOI: 10.1128/JCM.02638-10.


