Personal profile of systemic hemodynamics in solving global problems of public health.
Автор: Yakushin Mikhail А., Gorenkov Roman V., Dvorina Olga G., Yarotsky Sergey Yu., Shukurlaeva Guzal
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 16, 2020 года.
Бесплатный доступ
The study of systemic hemodynamics has been conducted in individuals who suffer from arterial hypertension. Regularities of formation of the personal profiles of the systemic hemodynamics have been determined in this category of patients. A fresh method of antihypertensive therapy is offered which is based on establishment of relationship between the personal profile of the systemic hemodynamics and the hemodynamic drug effect. The clinical effectiveness of the proposed method has been proven.
Arterial hypertension, metabolic syndrome, systemic hemodynamics, antihypertensive therapy, volume compression oscillometry
Короткий адрес: https://sciup.org/148311449
IDR: 148311449 | DOI: 10.12710/cardiometry.2020.16.3541
Текст научной статьи Personal profile of systemic hemodynamics in solving global problems of public health.
Imprint
Mikhail А. Yakushin, Roman V. Gorenkov, Olga G. Dvorina, Sergey Y. Yarotsky, Guzal Shukurlaeva. Personal profile of systemic hemodynamics in solving global problems of public health. Cardiometry; Issue 16; May 2020; р.35-41; DOI: 10.11576/cardiometry.2020.16.3541; Available from:
In 2018 the new guidelines of the European Society of Cardiology and the European Society “ESC/ ESH Clinical Practice Guidelines for the Management of Arterial Hypertension” (hereinafter referred to as the Guidelines) to govern the treatment of arterial hypertension (hereinafter: AH) came into force. The new revised edition of the document is substantially different from the previous one; proposed is a fundamentally new variant of the initial therapy of AH: instead of a single drug therapy it is recommended now to begin the treatment immediately with the use of a two-drug combination. Selection of the drug combination, as it has been the case before, is based on the presence of diseases associated with AH, as well as the state of the hypertension-mediated organs, i.e., the organs involved in pathophysiological processes caused by AH. The Guidelines’ developers present a variety of different strategies to initiate and escalate BP-lowering medication to improve BP control rates initiating treatment with different monotherapies and then sequentially adding other drugs until BP control is achieved almost as a fundamental solution of the AH problem, but at the same time they complain that "Despite this, BP control rates have remained poor worldwide”. The strategy developers believe that "bad" doctors should bear responsibilities for the stated inadequacy: they are those who are afraid of prescribing the proper dosage of the medical drugs and who are incapable of controlling BP medication; at the same time it is considered that patient adherence to treatment is low so that not all of them complete the course of their medication in full [1].
The effectiveness of the strategic approaches is treated in the Guidelines casually; in the opinion of the developers, there is a forceful argument in favor of the Guidelines’ correctness: “The evidence from RCTs demonstrating that BP control can be achieved in most recruited patients, and that no more than 5 - 10% of these patients exhibit resistance to the selected treatment regimen, suggests that ineffective drug therapy is not the source of the problem.”[1] (i.e. we, the strategy developers, escape our responsibility). In other words, if you have competent physicians and an eligible patient’s adherence, you can rise the efficacy of the AH treatment up to 90-95%!
Among the other things, the mere proposal to double the amount of the used drugs is an evidence for
Issue 16. May 2020 | Cardiometry | 35
an inefficacy of the conceptual approaches offered by them thereto. It is not the way to base the treatment strategies on taking into account comorbidities, when selecting the medication lines, since there are no accompanying diseases at the first stage of treatment; the target organs are not yet affected by the AH disease at the first stage; the presence of some associated clinical conditions points to a highly neglected disease case. In the meantime, in the scientific debates "hypertension remains the major preventable cause of cardiovascular disease (CVD) and all-cause death globally"; so that searching for fresh solutions to this problem is perhaps the most topical challenge for modern medicine [1].
Aims
The aims of our studies are systematization and applications of hemodynamic patterns in the diagnostics and treatment of AH.
Every medical student knows the following formula: AP = CO ■ TPVR, where AP is an arterial pressure; CO is cardiac output; TPVR is total peripheral vascular resistance [2].
Taking into account the fact that the CO is the product of the stroke volume (SV) by the heart rate (HR), i.e. CO = HR ■ SV, the AP value is directly dependent on three key factors: HR, SV and TPVR. By influencing these parameters, the level of AP can be controlled, both upwards and downwards. The only thing is to identify the relevant treating factors. This truth is so simple that it is really surprising why it has not been so far used as the primary conceptual approach to the treatment of AH, as well as arterial hypotension. But, unfortunately, there is even no attempt to discuss this conceptual assumption at all. This is much stranger, since the effect of antihypertensive drugs (AHD) on the systemic hemodynamics (SHD) is a well studied subject; the evidence data are directly available, including annotations to drugs (see Table 1 herein).
The only justification is that, until recently, the "gold standard” in SHD studies has been the Swan-Ganz pulmonary artery catheterization, which implies an insertion of a special catheter into one of the main branches in the pulmonary trunk. Such procedure is not safe; 2-3% of cases are complicated by serious disturbances in the heart rhythm and conduction that hinders the widespread use of the method, even under the in-hospital conditions [3].
At present, the above mentioned drawback has been removed; moreover, appeared are accessible and,
Table 1. Effects produced by AHD* on SHD
|
Group |
SAP |
DAP |
HR |
TPVR |
SV |
|
BB |
↓↓ |
↓ |
↓ |
↑↓ |
↓ |
|
CCB |
↓ |
↓ |
↓↑ |
↓ |
– |
|
TD |
↓ |
↓ |
– |
↓ |
↓ – |
|
ACEi |
↓ |
↓ |
– |
↓ |
↑ – |
|
ARB |
↓↓ |
↓ |
– |
↓ |
↑ – |
*Legend: BB - beta-blockers; CCB - calcium antagonists;
TD - thiazide diuretics, ACEi - ACE inhibitors, ARB - angiotensin receptor blockers; ↑ - increase, ↓ - decrease, – - no effect available.
most importantly, non-invasive techniques for investigating SHD, which reveal vast prospects for their use in general medical practice [4].
Materials and methods
The materials of our studies cover 1447 examinees aged from 18 to 89 (mean age 37.5 years), including 832 (57.5%) males and 615 (46.5%) females.
Our method of examination is the compression oscillometry: for this purpose, we have used device KAP TsG osm “GLOBUS" (Manufactured by Globus Ltd., Registration Certificate No. RZN2017/6582 dd. December 15, 2017), which allows non-invasively measuring 22 SHD parameters, including systolic arterial pressure (SAP), diastolic arterial pressure (DAP), HR, SV and TPVR. Since the values of SV and TPVR depend on the patient's height and weight and do not have clear standard boundaries, in our calculations we used their integral analogues: SI (stroke index), calculated as SV/T where T is a human body surface area (m2), and SPVR (specific peripheral vascular resistance) equal to TPVR/T. The standard SI value is 30-45 ml/m2, and the standard SPVR parameter is 32 ± 6% arbitrary units. It is assumed that the normal values of HR, SAP and DAP are as follows: HR 60-80 beats per min., SAP 120-130 mm Hg, DAP 70-80 mm Hg.
Results
Results obtained from our studies are given further below.
In the above examinees we have revealed various combinations of HR, SI and SPVR parameters; we have pooled them to form 15 SHD profiles. In this case, noteworthy is the detected dependence of each profile on the corresponding AP level (see Table 2 herein).
The following SHD profiles have not been detected in any examinee: 111, 131, 132, 133, 232, 233, 312, 313, 323, 331, 332 and 333. Besides, in patients with increased SAP and DAP we have never recorded the SHD profiles as listed below: 213, 223, and 322. The
Table 2. Dependence of SHD profile on AP level
|
SHD* profile (HR/ SPVR/SI) |
All |
AP<120 |
АP120-130 |
АP>140 |
АP>160 |
АP>170 |
DAP>90 |
|
112 |
10.9 |
3.9 |
4.8 |
17.6 |
3.6 |
0 |
23.2 |
|
113 |
3.1 |
9.1 |
0 |
5.2 |
0 |
0 |
4.7 |
|
121 |
0.3 |
0 |
0 |
0.7 |
4.5 |
2 |
0.2 |
|
122 |
9.4 |
11.7 |
9.6 |
15.3 |
0 |
0 |
2.7 |
|
123 |
0.7 |
0 |
1.2 |
1.1 |
0 |
0 |
0 |
|
211 |
8.5 |
0 |
3.6 |
11.8 |
12.5 |
10.4 |
18.4 |
|
212 |
19.5 |
14.3 |
25.3 |
4.5 |
32.1 |
37.6 |
24.3 |
|
213 |
1.3 |
10.4 |
0 |
0 |
0 |
0 |
0.9 |
|
221 |
16.4 |
6.5 |
19.3 |
18.1 |
14.3 |
8.3 |
4.8 |
|
222 |
14.3 |
39 |
22.9 |
7 |
0 |
0 |
0.9 |
|
223 |
0.1 |
1.2 |
0 |
0 |
0 |
0 |
0 |
|
231 |
0.4 |
0 |
0 |
0.2 |
0 |
0 |
0 |
|
311 |
4.7 |
0 |
7.3 |
7.1 |
18.7 |
22.9 |
13.9 |
|
321 |
10.2 |
1.3 |
6 |
11.2 |
14.3 |
18.8 |
6 |
|
322 |
0.3 |
2.6 |
0 |
0 |
0 |
0 |
0 |
*Notes: SHD profile is ratio HR / SPVR/ SI, where 1 - increased value of the parameter; 2 - normal value of the parameter; 3 -decreased value of the parameter.
Percentage shares (%) of SHD profiles in individuals with SAP <120
Percentage shares (%) of SHD profiles
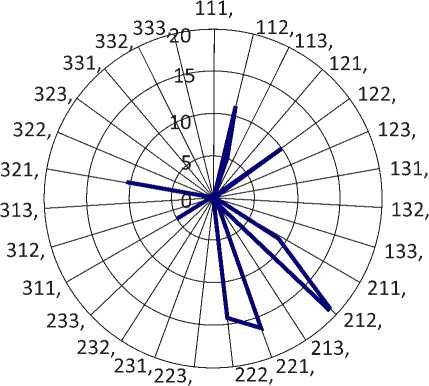
Figure 1
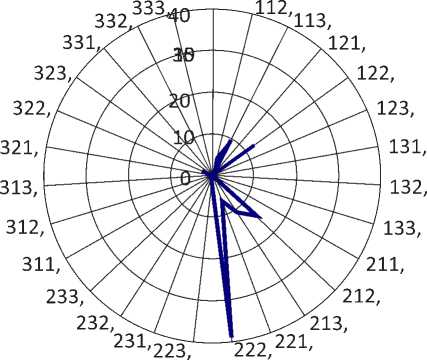
Figure 2
123 and 211SHD have not been found in the hypotension patients. The combination of the normal values of HR, SI and SPVR (SHD profile 222) occurred in 16.4% of the patients (see Figure 1 herein).
It would be logical to expect the prevalence of SHD profile 222 among the examinees with the normal levels of SAP and DAP. Indeed, in this category of examinees SHD, profile 222 occurs more often (22.9%), though not as often as one would expect. The above phenomenon may indicate only the following: AH is not only (and not as much as) an increase in AP. Early pathological manifestations of the AH disease in the form of impaired cardiac reflex activity and vascular tone imbalance for a long time are compensated by the redistribution of the hemodynamic constants. AP is the main hemodynamic parameter in the organism
Percentage shares (%) of SHD profiles in individuals with SAP of 120-130
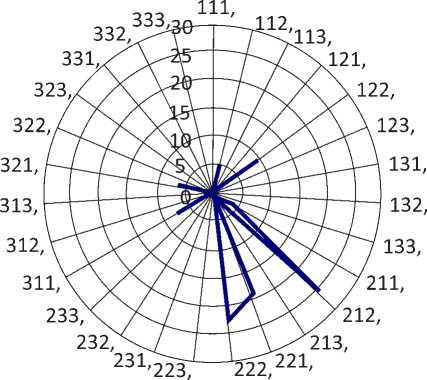
Figure 3
that provides normal perfusion; its stability guarantees an adequate blood supply to tissues; all compensatory hemodynamic responses are aimed at maintaining the normal AP level. The relatively rare occurrence of the normal hemodynamic profile is an indication of the completed compensatory hemodynamic responses at the early stages of AH.
The obtained data confirm the given concept: the normal SHD profile is almost absent in the patients with DAP> 90 mm Hg (0.9%); the profile has not been observed in the patients with SAP>152 mm Hg. All this clearly indicates that the exhaustion of the compensatory SHD mechanisms appears with grade 1 arterial hypertension.
In contrast thereto, in the patients with a decreased SAP (SAP <120) the normal SHD profile has been recorded 2 times more frequently (39%) than in those with the normal SAP. In our opinion, the logical explanation of this phenomenon is that a reduction in SAP is one of the earliest compensatory mechanisms of the response to an increase in the CO and TPVR parameters (see Figure 2 herein).
Among the examinees aged 18-25 years, a separate group is formed with healthy individuals according to their anamneses having the normal AP (n = 144). In the above category, only every fifth examinee (19.4%) has shown SHD profile 222 that is consistent with the previous results and gives us a reason to believe that hemodynamic disorders found prior to developing AH are formed well in advance before the first episodes of the abnormal AP increase [5].
The most frequently recorded case among the individuals with the normal SAP is SHD profile 212 (25.3%); less often found is SHD profile 221 (19.3%); every tenth (9.6%) has been reported to have SHD profile 122. The above distribution indirectly characterizes the polymorphism of the starting mechanisms in hemodynamic disorders preceding hypertension: in a third of patients (28.9%) the disorders start with increasing CO (SHD profile 221 and 122), and in every fifth individual (SHD profile 212) they begin with increasing TPVR (see Figure 3 herein).
A redistribution of the SHD profiles is a mandatory attribute of AH; at the same time, hemodynamics may change either according to the hyperkinetic type, which is characterized by an increase in the performance of the cardiac pumping activity (SV, HR), or in line with the hypokinetic type (distinguishing feature is the preferential growth of TPVR) or in accordance with the eukinetic type, when the values of all three parameters are in the middle of the oscillation range. At the onset of the disease, as a rule, the hyperkinetic hemodynamics prevails, while at its later stages the hypokinetic type is dominant [6, 7].
The obtained evidence data support the specified pattern regularity: in the patients with higher SAP observed is a tendency towards CO decreasing, while the share of individuals with an increased TPVR is directly proportional to the level of SAP (see Figure 4 herein).
Depending on the ratio between CO and TPVR, the SHD profiles are integrated by us in 3 groups: the hyperkinetic group (122, 221), the eukinetic group (222, 211, 321, 112, 113, 121, 123) and the hypokinetic group (311, 212). The relationship between the different SHD forms and SAP is shown in Figures 5, 6 and 7 herein.
Among the most common hyperkinetic SHD profiles, recorded has been profile 122; among the euki-netic profile types we have detected SHD profile 123; and among the hypokinetic profiles we have identified SHD profile 311.
Conclusions
The obtained results show that even in a healthy individual with the normal AP levels recording of a SHD physiological profile, which is characterized by the normal levels of CO and TPVR, is the exception rather than the rule. The share of individuals with impaired performance parameters CO and TPVR aged 18-25 years (80.6%) approximately correlates with the prevalence of AH among the individuals older than 60 years (80.7%). This correlation allows us suggesting that the AH onset should be related not to the age 40-50, as it is generally accepted, but much earlier life spans. It can be supposed that the hemodynamic disorder of this sort at the age of 25 may predict the onset of arterial hypertension with 60!
Latest research shows a close relationship between hypertension and the metabolic syndrome. It is believed that hyperinsulinemia and hyperleptinemia developing against the background of visceral obesity, associated with metabolic syndrome, contribute to an increase in CO and TPVR, thereby triggering the pathophysiological mechanisms of AH [8].
Knowing the SHD personal profile, we can select the proper AHD, taking into account its targeted effect on each component of the hemodynamics profile (see Table 3 herein).
Dynamics of different SHD profiles depending on SAP level
|
£ 60 ro -S 40 § 20 0 OJ CC |
||||
|
♦ |
||||
|
SAP 120 130 |
SAP>140 |
SAP>160 |
SAP>170 |
|
|
Hyperkinetic SHD profile |
28,9 |
33,8 |
14,3 |
8,3 |
|
Eukinetic SHD profile |
38,5 |
54,6 |
34,9 |
31,2 |
|
Hypokinetic SHD profile |
32,6 |
11,6 |
50,8 |
60,5 |
|
40 |
|
|
35 |
|
|
CD |
30 |
|
03 |
25 |
|
CD |
20 |
|
■43 |
15 |
|
го |
10 |
|
OJ CH |
5 |
Dynamics of hyperkinetic SHD profiles depending on SAP level
122,
221,
|
♦ ♦——^^^^ |
|||
|
SAP120-130 |
SAP>140 |
SAP>160 |
SAP>170 |
|
9,6 |
15,3 |
0 |
0 |
|
19,3 |
18,1 |
14,3 |
8,3 |
Figure 4
Figure 5
Dynamics of eukinetic SHD profiles depending on SAP level
|
2 60 |
||||
|
И 40 |
||||
|
> 7П |
||||
|
OJ n |
||||
|
or 0 |
SAP120-130 |
SAP>140 |
SAP>160 |
SAPS170 |
|
-•—123, |
1,2 |
1,1 |
0 |
0 |
|
*-121, |
0 |
0,7 |
4,5 |
2 |
|
-*-113, |
0 |
5,2 |
0 |
0 |
|
^eii2, |
4,8 |
17,6 |
3,6 |
0 |
|
—*—321, |
6 |
11,2 |
14,3 |
18,8 |
|
-■-211, |
3,6 |
11,8 |
12,5 |
10,4 |
|
—♦—222, |
22,9 |
7 |
0 |
0 |
Figure 6
Dynamics of hypokinetic SHD profiles depending on SAP level
|
to 70 2- 60 £ 50 ro 40 ф 30 5 20 5 10 0 |
||||
|
SAP120-130 |
SAP>140 |
SAP>160 |
SAP>170 |
|
|
-■-311, |
7,3 |
7,1 |
18,7 |
22,9 |
|
-♦-212, |
25,3 |
4,5 |
32,1 |
37,6 |
Figure 7
Table 3. Effects produced by AHD on SHD
|
AHP |
Registration No. (SRMP) |
HR |
TPVR 1 |
TPVR 2 |
SV |
|
Atenolol |
ЛП002294-051113 |
decrease |
increase |
decrease |
decrease |
|
Bisoprolol |
ЛП-004617-251117 |
decrease |
increase |
decrease |
decrease |
|
Betaxolol |
ЛП-002502-160614 |
decrease |
decrease |
decrease |
decrease |
|
Nevibilol |
П N011417/01-100809 |
decrease |
decrease |
decrease |
decrease |
|
Metoprolol |
ЛП-001760-020712 |
decrease |
increase |
decrease |
decrease |
|
Amlodipine |
ЛС-001987 |
no change |
decrease |
decrease |
no change |
|
Diltiazem |
ЛС-001987-261211 |
decrease |
decrease |
decrease |
no change |
|
Nifedipine |
ЛС-001381-190911 |
increase |
decrease |
decrease |
increase |
|
Nitrendipine |
ЛП-003289-051115 |
increase |
decrease |
decrease |
no change |
|
Moxonidine |
ЛП-003255-151015 |
no change |
decrease |
decrease |
no change |
|
Kaptopril |
ЛП-002918-170315 |
no change |
decrease |
decrease |
no change |
|
Chinapril |
П N014329/01-010411 |
no change |
decrease |
decrease |
no change |
|
Lizinopril |
ЛП-003753-260716 |
no change |
decrease |
decrease |
no change |
|
Perindopril |
ЛП-003712-290616 |
no change |
decrease |
decrease |
increase |
|
Ramipril |
ЛП-003235-081015 |
no change |
decrease |
decrease |
no change |
|
Fosinopril |
ЛП-003603-040516 |
no change |
decrease |
decrease |
no change |
|
Enalapril |
ЛП-002572-080814 |
no change |
decrease |
decrease |
increase |
|
Candesartan |
ЛП-002525-080714 |
no change |
decrease |
decrease |
no change |
|
Eprosartan |
П N012018/01-110310 |
no change |
decrease |
decrease |
no change |
|
Irbesartan |
ЛП-003987-011216 |
no change |
decrease |
decrease |
no change |
|
Losartan |
ЛСР-010617/08-261208 |
decrease |
decrease |
decrease |
increase |
|
Telmisartan |
ЛП-004442-010917 |
no change |
decrease |
decrease |
no change |
|
Valsartan |
ЛП-004219-300317 |
no change |
decrease |
decrease |
no change |
|
Indapamide |
ЛП-003095-170715 |
no change |
decrease |
decrease |
no change |
Legend: HR - heart rate; TPVR1 - total peripheral vascular resistance in the first month of starting treatment; TPVR2 - total peripheral vascular resistance after a month of starting treatment; SI - stroke index.
Table 4. AHD effects made on SHD
|
AHD group |
AHD |
Effect by AHD* on SHD (Code) |
|
Calcium antagonists |
Nitrendipine |
312 |
|
Nifedipine |
313 |
|
|
Diltiazem |
112 |
|
|
Amlodipine |
212 |
|
|
ACE inhibitors |
Perindopril, Enalapril |
213 |
|
Zofenopril, Kaptopril, Chinopril, Lizinopril, Ramipril, Fosinopril |
212 |
|
|
Betaxolol |
111 |
|
|
Beta-blockers |
Nevibilol |
112 |
|
Atenolol, Bisoprolol, Metoprolol |
141 |
|
|
Losartan |
113 |
|
|
Angiotensin receptor blockers |
Valsartan, Candesartan, Eprosartan, Irbesartan, Telmisartan |
212 |
|
Selective imidazoline receptor agonist |
Moxonidin |
212 |
|
Diuretics |
Dichlotiazide, Indapamide |
212 |
Table 5. AHD selection priority
|
Order of priority in AHD selection |
Characteristic |
|
1 |
Normalizing improperly changed (increased or decreased) parameters, not affecting the normal levels |
|
2 |
Normalizing improperly increased parameters, but decreasing the normal parameter |
|
3 |
Normalizing improperly increased parameters, not affecting the decreased parameter |
|
4 |
Normalizing improperly decreased parameters; not affecting the normal parameter |
|
5 |
Normalizing improperly decreased parameters, decreasing the normal parameter |
|
6 |
Normalizing one of the parameters, not affecting the other two |
|
7 |
Normalizing one of the parameters, not affecting the other one and decreasing the normal value of one more parameter |
|
8 |
Normalizing one of the parameters, not affecting the other one and increasing the normal value of one more parameter |
Table 6. AHD rating corresponding to individual SHD profiles
|
SHD* profile HR/SPVR/SI |
АP>140 |
АP>160 |
АP>170 |
Code and rating for AHD administration** |
|
112 |
17.6 |
3.6 |
0 |
112, 111, 141, 212, 113 |
|
113 |
5.2 |
0 |
0 |
113, 112, 213, 212 |
|
121 |
0.7 |
4.5 |
2 |
111, 141, 212, 112 |
|
122 |
15.3 |
0 |
0 |
112, 141, 111, 212, 113, 213 |
|
123 |
1.1 |
0 |
0 |
113, 112, 213, 212 |
|
211 |
11.8 |
12.5 |
10.4 |
111, 212, 112 |
|
212 |
4.5 |
32.1 |
37.6 |
212, 112, 111, 141, 213 |
|
221 |
18.1 |
14.3 |
8.3 |
111, 212, 112 |
|
222 |
7 |
0 |
0 |
212, 112, 111, 141, 213, 312 |
|
311 |
7.1 |
18.7 |
22.9 |
212, 312 |
|
321 |
11.2 |
14.3 |
18.8 |
312, 212 |
*The SHD profile is ratio HR / SPVR/ SI, where 1 - increased value of the parameter; 2 - normal value of the parameter; 3 - decreased value of the parameter.
** AHD Code - effect produced by AHD on HR/SPVR/SI, where 1 - decreasing the parameter; 2 - not affecting the parameter;
3 - increasing the parameter.
The mapping between the SHD profile and the AHD actions and effects on SHD is implemented by assigning a three-digit code (Code) to each drug; the first item of the Code exhibits the effect of AHD on HR (1- HR decrease, 2 - no effect, 3 – HR increase); the second item of the Code indicates the effect made by AHD on TPVR (1- TPVR decrease, 2 - no effect, 3 – TPVR increase 4 – increase of the parameter in the first month, and decrease therein after a month, etc.); the third Code item marks the effect produced by AHD on SV (1- SV decrease, 2 - no effect, 3 – SV increase) (see Table 4 herein).
The priority in selection of AHD definitely depends on the degree of its modulating effect produced on an individual SHD profile. Selected should be such a medical drug which is capable of normalizing improperly changed (increased or decreased) parameters of HR, SV and TPVR, but not affecting the SHD values remaining within the normal range. Characteristics of medical drugs of the second and next order of the priority are summarized by Table 5 herein.
Having identified the correlation between the individual SHD profile and the respective AHD, we can determine the rating modulating effect of the drugs on each SHD profile (see Table 6 herein).
Conclusions
-
1. Hemodynamic disorders appear at the preclinical stage of AH, well in advance (perhaps several decades) before the first recorded AH episodes.
-
2. In patients with increased AP, 15 variations of the SHD profiles are identified.
-
3. A hemodynamic effect of each AHD is determined by its pharmacodynamics as well as the patient’s individual SHD profile.
-
4. Taking into account of an individual SHD profile is an additional criterion for the AHD selection to increase the efficacy of the treatment based on the above mentioned Guidelines. The given conclusion is based on the evidence data, which have been obtained by us
earlier and which have demonstrated the effectiveness of this technology in nine times out of ten cases [9].
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Personal profile of systemic hemodynamics in solving global problems of public health.
- The 2018 ESC / ESH Guidelines for the treatment of patients with hypertension.
- Zayko NN, Byts YV, Ataman AV, et al. Pathological Physiology [Textbook for med. universities]. K.: "Logos", 1996. [in Russian]
- Intensive therapy. Guidelines for doctors. Ed. by Malyshev VD. Moscow: Medicine, 2002. [in Russian]
- Yakushin MA, Dasaev LA, Matyukhina EB. Algorithm of drug treatment of hypertension in middle and old age. Uspekhi Gerontologii. 2011;24(4):674-80. [in Russian]
- Gnedov DV. To a question on the status of systemic hemodynamics in today's youth. Bulletin of Medical Institute Reaviz. 2018;6(36):36-7. [in Russian]
- Horoshinina LP. Geriatrics. Guidance for doctors-GEOTAR Media, 2019. 698 p. [in Russian]
- Zidek V. Hypertension. GEOTAR Media, 2009. 206 с. [in Russian]
- Roitberg GE. Metabolic syndrome. Moscow: MED-press-inform, 2007. 224 p. [in Russian]
- Yakushin MA, Aleksandrova O, Yakushina TI, Vasilieva TP. Expert system for monitoring and correction of hemodynamic system in solving the strategic problems of public health. Practical medicine. 2019;17(5):241-9. [in Russian]


