Plasmalyte and ringer lactate as priming solutions in pediatric cardiopulmonary bypass: a comparative study
Автор: Abdellatif A.E., Alassa M.A., Ul-haq R., Abdelsabour M.M.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 28, 2023 года.
Бесплатный доступ
Background: Pediatric heart surgery, particularly for cyanotic congenital heart conditions, commonly requires the utilization of cardiopulmonary bypass(CPB)to assist with surgical interventions. The choice of priming solution for the CPB circuit can influence postoperative outcomes. This study aimed to assess the impact of two different priming solutions, Plasmalyte and Ringer’s Lactate, on postoperative outcomes, blood biochemistry, pulmonary and renal function, bleeding, and hemostasis in children undergoing open cardiac surgery with CPB. Methods: This randomized prospective study was conducted on 80 pediatric patients aged 1 to 10 years, undergoing elective cardiac surgery with CPB. Patients were randomly assigned to receive either Plasmalyte (Group A) or Ringer’s Lactate (Group B) as their CPB circuit priming solution. Standardized protocols for anesthesia, CPB circuit components, and surgical techniques were maintained. Postoperative parameters including blood chemistry, perfusion indicators, and physiological measurements were recorded and analyzed. Results: After CPB initiation, lactate levels were significantly higher in Group B (Ringer’s Lactate) compared to Group A (Plasmalyte)(P-value function show_abstract() { $('#abstract1').hide(); $('#abstract2').show(); $('#abstract_expand').hide(); }
Pediatric cardiac surgery, cardiopulmonary bypass, priming solutions, plasmalyte, ringer's lactate, postoperative outcomes
Короткий адрес: https://sciup.org/148327107
IDR: 148327107 | DOI: 10.18137/cardiometry.2023.28.3442
Текст научной статьи Plasmalyte and ringer lactate as priming solutions in pediatric cardiopulmonary bypass: a comparative study
Anhar Elsayed Abdellatif, Mohamed A Alassal, Raihan-Ul-Haq, Mohamed Meselhy Abdelsabour. Plasmalyte and Ringer Lactate as Priming Solutions in Pediatric Cardiopulmonary Bypass: A Comparative Study. Cardiometry; Issue No. 28; August 2023; p. 34-42; DOI: 10.18137/cardiometry.2023.28.3442; Available from: plasmalyte-and-ringer-lactate-priming-solutions
Pediatric cardiac surgery, especially in cases of cyanotic congenital heart diseases, often necessitates the use of cardiopulmonary bypass (CPB) to facilitate surgical interventions. CPB serves as a vital tool to maintain cardiocirculatory stability during the delicate procedures required to correct these complex cardiac anomalies [1, 2]. One of the critical components of the CPB system is the priming solution, which not only replaces the patient’s blood but also serves to optimize the CPB circuit’s function. The choice of priming solution can potentially exert a profound impact on various physiological parameters and postoperative outcomes [3, 4].
The selection of the appropriate priming solution for the CPB circuit is a multifaceted decision. Ringer’s lactate, a commonly employed fluid, possesses properties conducive to maintaining electrolyte balance and replenishing fluid losses [5]. On the other hand, the Balanced crystalloid, plasmalyte, containing gluconate as an organic anion, offers the advantage of maintaining a physiological electrolyte composition while potentially mitigating the metabolic derangements associated with lactate accumulation. As the intricate interplay of electrolytes, acid-base balance, and metabolic homeostasis significantly influences postoperative recovery, a careful examination of the effects of these priming solutions is imperative [6, 7].
Pediatric patients undergoing cardiac surgery are particularly vulnerable to perturbations in electrolyte balance and acid-base equilibrium. The choice of priming solution can impact these delicate physiological mechanisms, potentially influencing postoperative blood biochemistry. Metabolic acidosis, a common concern in cardiac surgery, can be exacerbated by lactate accumulation from Ringer’s lactate use. Plasma-lyte’s gluconate component, which metabolizes to bicarbonate, may offer a more balanced alternative [8, 9].
Beyond metabolic considerations, the influence of priming solutions on pulmonary function and renal outcomes warrants investigation. Pediatric patients with cyanotic congenital heart diseases often experience compromised pulmonary function [10]. The priming solution’s osmolarity and composition could affect lung mechanics and gas exchange postopera-tively. Similarly, renal function, often jeopardized in cardiac surgery due to perfusion-related factors, may be influenced by the priming solution’s impact on hemodynamics and electrolyte balance [11].
Postoperative bleeding and hemostasis are critical determinants of patient recovery. The interaction between the priming solution and the patient’s coagulation system can potentially modulate bleeding tendencies. Variations in hemostasis could be attributed to the priming solution’s impact on platelet function, clotting factors, and fibrinolysis [12].
Ultimately, the collective impact of these physiological variables converges into the overarching outcomes of mortality and morbidity. While both priming solutions aim to facilitate successful surgical interventions, disparities in their effects on various parameters could potentially translate into divergent clinical trajectories.
Therefore, we aimed to assess the impact of priming the CPB circuit with different fluids in children with cyanotic congenital heart diseases undergoing open cardiac surgery using CPB. The effects of two fluid types, Ringer’s lactate and a balanced crystalloid containing gluconate (plasmalyte), on postoperative blood biochemistry, pulmonary function, renal function, postoperative bleeding, and hemostasis are examined. Additionally, the study investigated potential differences in mortality or morbidity associated with the two crystalloid options.
Materials and Methods
Study Population and Randomization:
In this randomized prospective study, a total of 80 pediatric patients, ranging in age from 1 year to 10 years, with weights between 6 kgs and 25 kgs, were included. The study was conducted at Prince Abdullah Bin Musaed Cardiac Centre (PAMCC), Saudi Arabia during the period from January 2022 to January 2023 after being approved from the Research Ethics Committee. These patients underwent elective cardiac surgery with the utilization of cardiopulmonary bypass. They were randomly divided into two groups: group A (n=40) and group B (n=40).
Group A received a crystalloid prime solution containing Gluconate (Plasmalyte) for priming the cardiopulmonary bypass circuit, while group B received Ringer’s Lactate as their priming solution. Comparative analysis of age, sex, body weight, clinical diagnosis, operative procedure, and approximate bypass time was conducted between the two groups.
Table 1
Difference in composition in each 100 ml of the two priming solutions
|
Composition |
Plasmalyte |
Ringer lactate |
|
pH |
7.4 |
6.5 |
|
Sodium(mmol/L) |
140 mmol/l |
131 mmol/L |
|
Potassium(mmol/L) |
5 mEq/l |
5 mEq/L |
|
Calcium(mmol/L) |
- |
2 mEq/L |
|
Magnesium(mmol/L) |
3 mmol/l |
|
|
Chloride(mmol/L) |
98 mmol/l |
111 mmol/L |
|
Bicarbonate(mmol/L) |
- |
(as lactate) |
|
Lactate(mmol/L) |
- |
29 mmol/L |
|
Acetate (mmol/L) |
27 mmol/l |
- |
|
Osmolarity |
294 mOsmol/L |
273 mOsm/L. |
|
Gluconate |
23 mmol/l |
- |
|
Caloric content |
21 kcal/L |
9 kcal/L |
The study adhered to a standardized protocol for CPB circuit component selection, which encompassed a heat exchanger, reservoir, oxygenator, arterial line filter, and blood cardioplegia delivery system. The surgical and anesthetic techniques, pump flows, conduct of bypass, and hypothermia were consistent in both groups, differing only in the choice of priming solution used in the CPB circuit.
Inclusion Criteria:
Children aged 1 to 10 years, weighing between 6 and 25 kg, who have been diagnosed with congenital or acquired heart conditions necessitating surgical intervention employing CPB. Additionally, stable preoperative hemodynamics and no known allergies to the constituents of Plasmalyte or Ringer’s Lactate solutions.
Exclusion Criteria:
The study excluded patients with acyanotic congenital heart diseases, those with weight below 6 kgs or above 25 kgs, and individuals above 10 years of age. Patients with renal failure, liver failure, known allergy to the interventions’ components, and bleeding disorders were also excluded.
Cardiopulmonary Bypass:
All patients underwent anesthesia in accordance with the institutional protocol, with standardized induction and maintenance procedures. The same general anesthesia protocol was applied to both groups. Intravenous fluid administration was tailored to each group. Cardiopulmonary bypass was carried out using a membrane oxygenator and non-pulsatile flow maintained between 100 ml/kg/min and 150 ml/kg/min via a twin roller pump. A priming volume of 700-1100 ml was employed for de-airing the circuit. The heart-lung machine circuit was primed with specific prime fluids: 20ml/kg body weight of Plasmalyte for group A, and Ringer’s Lactate for group B, along with Mannitol, Heparin, and NaHCO3 in standardized quantities.
Anticoagulation and Myocardial Preservation:
Before initiating CPB, anticoagulation was achieved through the administration of 400 U/kg heparin sodium, aiming to maintain an activated clotting time (ACT) above 480 seconds throughout the procedure. Myocardial preservation involved cold blood cardioplegia and hypothermia using a Del Nido-based cardioplegia solution prepared in-house.
Postoperative Care and Analysis:
Upon completing the corrective surgery, patients were rewarmed to an esophageal temperature of 35°C. Surgical hemostasis was established before administering protamine sulfate. Anticoagulation was reversed at the termination of CPB using protamine sulfate, infused at a dose of 1.3 mg per 100 U of total administered heparin. Subsequently, patients were transferred to the intensive care unit (ICU).
Comprehensive data analysis included recording and examination of parameters such as hemoglobin, 36 | Cardiometry | Issue 28. August 2023
hematocrit, blood pressure, saturation levels, blood gases, urine output, blood glucose, serum creatinine, perfusion pressures, blood flows, gas flows, temperature, pH, electrolyte concentrations, and various other indicators throughout different phases of the bypass procedure.
Statistical analysis
SPSS software, version 25 (SPSS Inc., PASW statistics for windows version 25. Chicago: SPSS Inc.), was used for data analysis. Qualitative data were presented using numbers and percentages. For quantitative data, non-normally distributed data were described using median (minimum and maximum), while normally distributed data were described using mean ± standard deviation. Normality of the data was tested using the Kolmogrov-Smirnov test. To compare qualitative data between groups, Chi-Square and Monte Carlo tests were used as appropriate. For non-normally distributed data, the Wilcoxon signed rank test was used to compare two studied periods. Student t-test was used to compare two independent groups for normally distributed data. Paired t-test was used to compare two paired readings of distributed data. Within-group comparisons of the parameters over the duration were conducted using the Friedman test. The significance of the results was determined at the level of ≤0.05.
Results
Eighty cases were recruited randomly into two groups of equal size. All cases were then followed and statistically analyzed. They were randomly divided into two equal groups: Group A received a crystalloid prime solution containing Gluconate (Plasmalyte) for priming the cardiopulmonary bypass circuit, while group B received Ringer’s Lactate as their priming solution. Figure 1
The demographic data showed no statistically significant differences regarding body surface area, bypass time, cross clamp time and priming volume between the group A (Plasmalyte) and group B (Ringer’s Lactate). Table 2
The preoperative data were insignificantly different between both studied groups. In group A (Plasm-alyte), mean value of lactate was 1.04 mmol/L whereas in group B (Ringer Lactate), mean value of lactate was 0.98 mmol/L. Mean value of calcium was 0.89 mmol/L in group A and 0.9 mmol/L in group B, no significant difference was seen preoperatively. Table 3
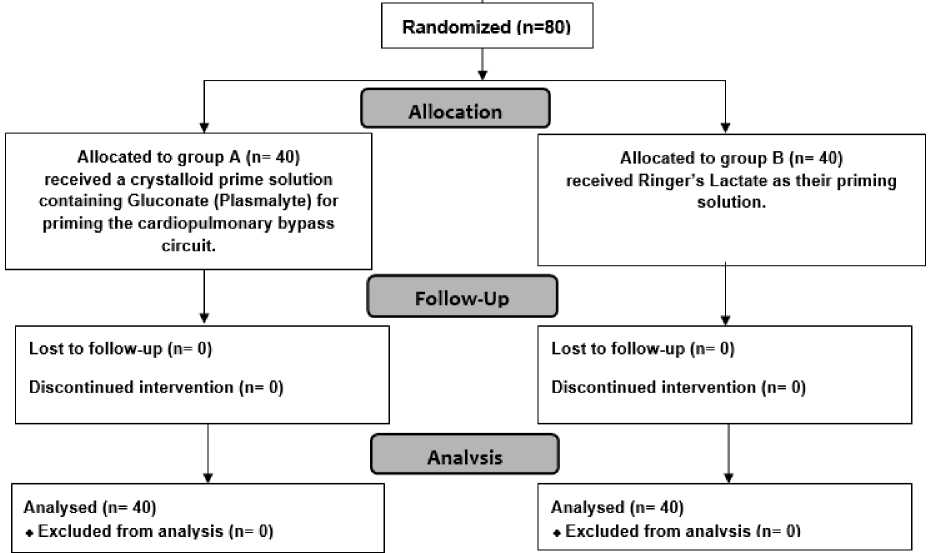
Figure 1: CONSORT flowchart of the studied patients.
Table 2
Demographic data of all patients
|
Parameters |
Group A (Plasmalyte) |
Group B (Ringer’s Lactate) |
P-value |
|
BSA(m2) |
0.462 ± 0.18 |
0.5245 ± 0.176562 |
0.123 |
|
BYPT (min) |
97.325 ± 42.97 |
123.525 ± 42.38468 |
0.089 |
|
CCT (min) |
59.55 ± 28.84003 |
69.03 ± 20.87 |
0.089 |
|
Priming vol (ml) |
671.25 ± 156.48 |
725 ± 133.49 |
0.104 |
*Mean ± standard deviation values are taken for analysis, BSA – Body Surface Area, BYPT – Bypass time, CCT – Cross Clamp time.
Table 3
Preoperative data
|
Parameters |
Group A (Plasmalyte) |
Group B (Ringer’s Lactate) |
P-value |
|
Hct (%) |
50.55±9.62 |
49.425±10.56 |
0.2716 |
|
pH |
7.37 ± 0.076 |
7.33±0.09 |
0.320 |
|
pO2 (mmHg) |
117.22 ± 73.84 |
157.97 ± 57.52 |
0.170 |
|
HCO3-(mmol/L) |
21.31 ± 2.72 |
21.96 ± 5.82 |
0.525 |
|
BE (mmol/L) |
2.05 ± 0.75 |
-0.35 ± 0.56 |
0.884 |
|
Lactate (mmol/L) |
1.04 ± 0.38 |
0.98 ± 0.46 |
0.551 |
|
Sugar(mg/dl) |
95 ± 20.45 |
98.6 ± 29.59 |
0.530 |
|
K+(mmol/L) |
3.59 ± 0.46 |
3.74 ± 0.46 |
0.152 |
|
Na+(mmol/L) |
134.1 ± 3.71 |
130.49 ± 20.82 |
0.283 |
|
Ca2+(mmol/L) |
0.89 ± 0.195 |
0.903 ± 0.283 |
0.321 |
|
SpO 2 (%) |
90.97 ± 10.27 |
90.35 ± 18.50 |
0.852 |
|
Perfusion pressure(mmHg) |
49.37 ± 19.60 |
50.42 ± 11.40 |
0.352 |
|
Urine Output(ml) |
51.32 ± 30.46 |
59.12 ± 28.31 |
0.222 |
|
Urea(mg%) |
31.5 ± 10.51 |
25.76 ± 11.24 |
0.304 |
|
Creatinine(mg%) |
0.47 ± 0.27 |
0.43 ± 0.23 |
0.458 |
|
BIL (mg%) |
0.48 ± 0.17 |
0.42 ± 0.6 |
0.601 |
*Mean ± standard deviation values are taken for analysis, HCT – Hematocrit, pO2 – Partial Pressure of Oxygen, HCO3 – Bicarbonate, BE – Base Excess, K+ – Potassium, Na+ – Sodium, Ca2+ – Calcium, SpO2 – Saturation of Peripheral Oxygen, BIL – Bilirubin.
Data for all the parameters was compared in both groups after onset of ischemic time. Lactate (P-value <0.001), and calcium (P-value <0.001), values were found statistically significant. In contrast to data obtained preoperatively, lactate and calcium levels increased in group B (Ringer lactate). Lactate was higher in group B 3.46 mmol/L (±1.47) compared to group A 1.64 mmol/L (±0.99), while calcium level was lower in group A 0.821 mmol/L (±0.181) compared to group B children 1.03mmol/L (±0.24). Table 4
Mean of lactate and calcium values were compared in the two groups. In contrast to data obtained after cross clamp removal, lactate and calcium levels increased in group B (Ringer lactate). Lactate was higher in group B 2.71 mmol/L (±1.38) compared to group A 1.70 mmol/L (±0.67), while calcium level was lower in group
A 0.88 mmol/L (±0.146) compared to group B children 1.10mmol/L (±0.16). Mean values of lactate and calcium increased further in group B (Ringer lactate) whereas base excess values were higher in group A. Table 5
Post operatively lactate levels were higher in group B 2.33mmol/L (±1.43) as compared to group A 1.69mmol/L (±0.61). The mean values of all other parameters were within normal ranges, and there was no statistically significant difference between the two groups. Table 6
Values of lactate (p=0.00041) was statistically significant postoperatively in group B. Table 7
The value of bicarbonate (P-value= 0.048), lactate (P-value <0.001), calcium (P-value= 0.013), urine output (P-value <0.001), urea (P-value= 0.0056) and creatinine (P-value= 0.049) were statistically significant at 6th hour postoperatively. Table 8
Table 4
Operative data on cross clamp application
|
Parameters |
Group A (Plasmalyte) |
Group B (Ringer’s Lactate) |
P value |
|
Hct (%) |
32.84±10.03 |
29.07±6.98 |
0.057 |
|
pH |
7.30±0.63 |
7.43±0.06 |
0.057 |
|
pO2(mmHg) |
230.12±45.11 |
239.87±57.66 |
0.404 |
|
HCO3-(mmol/L) |
24.54±3.60 |
25.07 ± 3.08 |
0.316 |
|
BE (mmol/L) |
0.76± 0.64 |
1.20±0.43 |
0.578 |
|
Lactate (mmol/L) |
1.64±0.99 |
3.46±1.47 |
0.00001 |
|
Sugar(mg/dl) |
112.64±38.38 |
120.27±45.27 |
0.421 |
|
K+(mmol/L) |
4.13±0.80 |
4.24±0.84 |
0.544 |
|
Na+(mmol/L) |
134.07±3.97 |
135.32±3.83 |
0.159 |
|
Ca2+(mmol/L) |
0.821±0.181 |
1.03±0.24 |
0.000028 |
|
SpO 2 (%) |
99.85±0.42 |
99.95±0.31 |
0.237 |
|
Perfusion pressure(mmHg) |
49.37±19.60 |
50.42±11.40 |
0.772 |
*Mean ± standard deviation values are taken for analysis, *P value <0.05 is statistically significant, HCT- Hematocrit, pO2 – Partial Pressure of Oxygen, HCO3 – Bicarbonate, BE – Base Excess, K+ – Potassium, Na+ – Sodium, Ca2+ – Calcium, SpO2 – Saturation of Peripheral Oxygen, BIL – Bilirubin.
Table 5
Operative data on Cross Clamp removal.
|
Parameters |
Group A (Plasmalyte) |
Group B (Ringer’s Lactate) |
P value |
|
Hct (%) |
34.17 ± 7.07 |
32.03 ± 6.16 |
0.681 |
|
pH |
7.43±0.05 |
7.439 ± 0.059 |
0.326 |
|
pO2(mmHg) |
199.22±52.41 |
202.37±57.03 |
0.798 |
|
HCO3-(mmol/L) |
25.75±2.53 |
25.09±2.88 |
0.284 |
|
BE (mmol/L) |
2.03±0.67 |
0.44±0.12 |
0.020 |
|
Lactate (mmol/L) |
1.705±0.67 |
2.71±1.38 |
0.000086 |
|
Sugar(mg/dl) |
147.12±44.90 |
153.27±43.54 |
0.538 |
|
K+(mmol/L) |
4.05±0.62 |
4.42±0.62 |
0.105 |
|
Na+(mmol/L) |
137.52±3.67 |
137.6±4.38 |
0.934 |
|
Ca2+(mmol/L) |
0.88±0.146 |
1.10±0.16 |
0.00001 |
|
SpO 2 (%) |
99.87±0.33 |
100 ± 0 |
1 |
|
Perfusion pressure (mmHg) |
53.15 ± 21.91 |
51.1±9.95 |
0.595 |
|
Urine Output (ml) |
175.05±122.87 |
432.62±321.85 |
0.00001 |
Table 6
Operative Data after weaning off.
|
Parameters |
Group A (Plasmalyte) |
Group B (Ringer’s Lactate) |
P value |
|
Hct (%) |
36.58±7.16 |
35.47±6.49 |
0.471 |
|
pH |
7.39±0.04 |
7.37±0.07 |
0.104 |
|
pO2(mmHg) |
169.75±95.41 |
167.82±93.36 |
0.927 |
|
HCO3-(mmol/L) |
23.83±3.14 |
23.26±3.09 |
0.417 |
|
BE (mmol/L) |
0.915±0.52 |
-1.04±0.14 |
0.009 |
|
Lactate (mmol/L) |
1.69±0.615 |
2.33±1.43 |
0.011 |
|
Sugar(mg/dl) |
160.72±41.99 |
167.67±65.75 |
0.576 |
|
K+(mmol/L) |
3.78±0.423 |
3.73±0.59 |
0.688 |
|
Na+(mmol/L) |
135.54±17.03 |
137.9±4.32 |
0.403 |
|
Ca2+(mmol/L) |
1.19±0.85 |
1.21±0.61 |
0.942 |
|
SpO 2 (%) |
99.38±1.48 |
98.37±6.03 |
0.309 |
|
Perfusion pressure (mmHg) |
70.97±16.73 |
69.6±17.27 |
0.720 |
-
*Mean + standard deviation values are taken for analysis, *P value <0.05 is statistically significant, HCT- Hematocrit, pO2 – Partial Pressure of Oxygen, HCO3 – Bicarbonate, BE – Base Excess, K+ – Potassium, Na+ – Sodium, Ca2+ – Calcium, SpO2 – Saturation of Peripheral Oxygen, BIL – Bilirubin.
Table 7
Postoperative data after 1hour of ICU stay.
|
Parameters |
Group A (Plasmalyte) |
Group B (Ringer’s Lactate) |
P value |
|
Hct (%) |
37.69±5.75 |
37.37±5.06 |
0.793 |
|
pH |
7.39±0.03 |
7.39±0.05 |
0.883 |
|
pO2(mmHg) |
155.75±57.22 |
158.77±56.83 |
0.780 |
|
HCO 3 -(mmol/L) |
23±2.80 |
22.65±2.35 |
0.558 |
|
BE (mmol/L) |
0.68±0.40 |
-0.29±0.83 |
0.044 |
|
Lactate (mmol/L) |
1.64±1.04 |
2.69±1.10 |
0.000041 |
|
Sugar(mg/dl) |
159.07±37.30 |
159.27±51.24 |
0.984 |
|
K+(mmol/L) |
3.72±0.35 |
3.63±0.36 |
0.322 |
|
Na+(mmol/L) |
139.125±4.13 |
136.6±15.59 |
0.334 |
|
Ca2+(mmol/L) |
0.94±0.20 |
1.01±0.27 |
0.177 |
|
SpO 2 (%) |
99.28±2.99 |
99.5±3.16 |
0.751 |
|
Perfusion pressure (mmHg) |
74.62±14.43 |
75.2±13.08 |
0.853 |
-
*Mean + standard deviation values are taken for analysis, *P value <0.05 is statistically significant, HCT- Hematocrit, pO2 – Partial Pressure of Oxygen, HCO3 – Bicarbonate, BE – Base Excess, K+ – Potassium, Na+ – Sodium, Ca2+ – Calcium, SpO2 – Saturation of Peripheral Oxygen, BIL – Bilirubin.
Table 8
Postoperative data after 6 hours of ICU stay.
|
Parameters |
Group A (Plasmalyte) |
Group B (Ringer’s Lactate) |
P value |
|
Hct (%) |
37.48±4.01 |
37.98±4.17 |
0.586 |
|
pH |
7.39±0.02 |
7.38±0.04 |
0.131 |
|
pO2(mmHg) |
161.08±45.53 |
161.65±56.74 |
0.960 |
|
HCO3-(mmol/L) |
23.53±2.80 |
22.34±2.47 |
0.048 |
|
BE (mmol/L) |
0.25±0.05 |
0.22±0.47 |
0.643 |
|
Lactate (mmol/L) |
1.51±0.53 |
2.47±1.54 |
0.0004 |
|
Sugar(mg/dl) |
155.37±36.68 |
139.07±41.45 |
0.067 |
|
K+(mmol/L) |
3.70±0.23 |
6.92±20.28 |
0.318 |
|
Na+(mmol/L) |
139.86±4.07 |
139.53±4.64 |
0.737 |
|
Ca2+(mmol/L) |
0.98±0.17 |
1.09±0.20 |
0.013 |
|
SpO 2 (%) |
99.62±1.18 |
99.97±0.15 |
0.070 |
|
Perfusion pressure (mmHg) |
76.95±17.09 |
78.7±13.00 |
0.609 |
|
Urine Output (ml) |
185±126.72 |
340.37±226.17 |
0.0013 |
|
Urea (mg%) |
26.92±7.89 |
20.83±10.93 |
0.0056 |
|
Creatinine (mg%) |
0.39±0.20 |
0.31±0.13 |
0.049 |
|
BIL (mg%) |
0.38±0.36 |
0.28±0.20 |
0.132 |
Discussion
Pediatric patients with cyanotic congenital heart diseases undergoing open cardiac surgery with cardiopulmonary bypass (CPB) require careful consideration of priming solutions for the CPB circuit [13, 14].
This study aimed to compare the effects of Plasm-alyte and Ringer Lactate as priming solutions on postoperative outcomes in these patients.
This randomized prospective study was conducted at Prince Abdullah Bin Musaed Cardiac Centre (PAMCC), Saudi Arabia on eighty pediatric patients (1-10 years old, weight 6-25 kgs) undergoing elective cardiac surgery with CPB who were divided into two groups: Plasmalyte (Group A) and Ringer Lactate (Group B). The CPB circuit was primed with either Plasmalyte or Ringer Lactate, with standardized protocols for CPB components, surgical techniques, and anesthetic management.
The selection of Plasmalyte and Ringer Lactate as priming solutions for the CPB circuit in this study was based on established medical literature and clinical rationale. Both Plasmalyte and Ringer Lactate are commonly utilized crystalloid solutions with distinct compositions and properties that make them suitable for use in CPB procedures [15].
Plasmalyte, a balanced crystalloid solution containing gluconate, has been gaining attention for its potential advantages in maintaining electrolyte balance and minimizing metabolic disturbances during CPB [6, 16]. Studies have suggested that Plasmalyte may help mitigate acid-base imbalances and reduce the risk of hyperchloremic acidosis, which can occur with other crystalloid solutions. This is of particular importance in CPB procedures, where shifts in electrolyte and acid-base equilibrium can impact patient outcomes. The inclusion of gluconate in Plasmalyte may also contribute to improved cellular hydration and decreased inflammatory response, factors that could influence postoperative recovery [17, 18].
Ringer Lactate, another commonly used crystalloid solution, contains sodium chloride, potassium chloride, calcium chloride, and sodium lactate. Its composition makes it suitable for maintaining fluid balance and addressing metabolic acidosis. Ringer Lactate has been traditionally utilized in various clinical settings, including CPB procedures, due to its ability to restore electrolyte levels and correct acid-base disturbances [19, 20].
The choice between Plasmalyte and Ringer Lactate as priming solutions for CPB circuits is an area of 40 | Cardiometry | Issue 28. August 2023
ongoing research and clinical consideration. Existing literature has demonstrated the potential benefits of Plasmalyte in reducing metabolic derangements and inflammation compared to other crystalloid solutions [15, 21].
Regarding the study findings, demographic data showed no significant differences between the groups. Postoperative analysis revealed that lactate levels were significantly lower in Group A compared to Group B at various time points after CPB initiation (p < 0.05). Calcium levels displayed significant variation between the two groups postoperatively, with higher levels in Group B (p < 0.05). Other parameters, including blood biochemistry, pulmonary function, renal function, bleeding, and hemostasis, did not exhibit statistically significant differences between the groups.
Surabhi and Kumar compared the metabolic effects of Ringer Lactate and Plasmalyte-A as cardiopulmonary bypass (CPB) primes in valve replacement surgeries. They observed that the patients who received Plasma-lyte-A as CPB prime developed less metabolic acidosis compared to those who received Ringer Lactate. The Ringer Lactate group showed reductions in pH, bicarbonates, and strong ion difference during CPB, along with a significant surge in blood lactate levels. These changes suggested the development of metabolic acidosis in the Ringer Lactate group. Additionally, the Ringer Lactate group had a higher number of patients experiencing hypotension and arrhythmias, indicating a higher degree of acidosis and potential adverse effects [15]. In contrast, based on our results, as we found that lactate levels were significantly higher in the Ringer Lactate group, other parameters such as blood biochemistry, pulmonary function, renal function, bleeding, hemostasis, and other postoperative outcomes did not exhibit statistically significant differences between the Plasmalyte and Ringer Lactate groups.
Liskaser et al. [21] conducted a study comparing Ringer’s solution and Plasmalyte-A as a bypass prime and concluded that the acidosis appeared to be iatrogenic in nature and derived from the effect of the pump-prime fluid based on the acid-base balance. The extent of such acidosis and its duration varied depending on the type of pump prime.
In line with the current study, Weinberg et al. [17] observed the development of metabolic acidosis in relation to the use of different priming solutions during cardiac surgeries. In both studies, the choice of priming solution had an impact on acid-base balance.
However, In Weinberg et al.’s study [17], there was significant hyperchloremia with Hartmann’s solution compared to Plasmalyte-A. In our study, while lactate levels were significantly higher in the Ringer Lactate group, no significant differences in hyperchloremia were reported between the Plasmalyte and Ringer Lactate groups.
The mechanisms of acidosis observed with different priming solutions in Weinberg et al.’s [17] study differ from those implied in our study. In their study, the acidosis observed with Hartmann’s solution was attributed to both iatrogenic hyperlactatemia and hyperchloremia. In contrast, Plasmalyte-A was associated with the production of unmeasured anions (acetate and gluconate). In our study, while lactate levels were higher with Ringer Lactate, the specific mechanism for acidosis was not discussed in the preliminary results provided.
Moreover, Weinberg et al. [17] noted significant hyperlactatemia with Hartmann’s solution but not with Plasmalyte-A. In our results, the Ringer Lactate group exhibited higher blood lactate levels compared to the Plasmalyte group.
This result is in accordance with Surabhi et al. wherein both groups developed metabolic acidosis on the delivery of pump prime. There was significant hyperlactatemia with Ringer’s lactate compared to Plasmalyte-A. The SID decreased during the CPB in the Ringer’s lactate group (41.102 mEq/L at T1to 35.66 mEq/L [P = 0.033] at T2) in comparison to Plas-malyte-A group [15].
In a study conducted by Teloh et al. [22] 25 patients undergoing elective isolated CABG with CPB revealed the existence of transitional dilutional acidosis during CPB. Patients, however, did not show overt lactic acidosis.
Moreover, the findings from previous studies and our study are consistent with the identified advantages of Plasmalyte-A over Ringer’s lactate in terms of improved acid-base status and the lactate level.
Finally, this study had some limitations; firstly, the relatively small sample size and single-center design may restrict the generalizability of findings. Secondly, the exclusion criteria could impact the representation of patients with certain comorbidities. Thirdly, the absence of blinding may introduce potential biases. Finally, the study’s focus on short-term outcomes and specific time points may limit the understanding of longer-term effects.
Conclusion
Priming the CPB circuit with Plasmalyte may be associated with favorable outcomes in terms of lactate and calcium levels compared to Ringer Lactate in pediatric patients undergoing cardiac surgery. Further research is needed to elucidate the clinical implications of these findings and to determine potential long-term effects on postoperative recovery and morbidity.
Список литературы Plasmalyte and ringer lactate as priming solutions in pediatric cardiopulmonary bypass: a comparative study
- Kumar TKS. Practical conduct of open heart procedures for congenital heart lesions. J Thorac Dis. 2020; 12:1235-59.
- Gibbison B, Villalobos Lizardi JC, Avilés Martínez KI, Fudulu DP, Medina Andrade MA, Pérez-Gaxiola G, et al. Prophylactic corticosteroids for paediatric heart surgery with cardiopulmonary bypass. Cochrane Database Syst Rev. 2020;10:Cd013101.
- Vercaemst L. Hemolysis in cardiac surgery patients undergoing cardiopulmonary bypass: a review in search of a treatment algorithm. J Extra Corpor Technol. 2008;40:257-67.
- Sarkar M, Prabhu V. Basics of cardiopulmonary bypass. Indian J Anaesth. 2017;61:760-7.
- Gu YJ, Boonstra PW. Selection of priming solutions for cardiopulmonary bypass in adults. Multimed Man Cardiothorac Surg. 2006;2006:mmcts.2005.001198.
- Semler MW, Kellum JA. Balanced Crystalloid Solutions. Am J Respir Crit Care Med. 2019;199:952-60.
- Curran JD, Major P, Tang K, Bagshaw SM, Dionne JC, Menon K, et al. Comparison of Balanced Crystalloid Solutions: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Crit Care Explor. 2021; 3:e0398.
- Vaska PL. Fluid and electrolyte imbalances after cardiac surgery. AACN Clin Issues Crit Care Nurs. 1992; 3:664-71.
- Kilic O, Gultekin Y, Yazici S. The Impact of Intravenous Fluid Therapy on Acid-Base Status of Critically Ill Adults: A Stewart Approach-Based Perspective. Int J Nephrol Renovasc Dis. 2020;13:219-30.
- Patra S, Rama Sastry UM, Mahimaiha J, Subramanian AP, Shankarappa RK, Nanjappa MC. Spectrum of cyanotic congenital heart disease diagnosed by echocardiographic evaluation in patients attending paediatric cardiology clinic of a tertiary cardiac care centre. Cardiol Young. 2015;25:861-7.
- Young RW. Prevention of lung injury in cardiac surgery: a review. J Extra Corpor Technol. 2014;46:130-41.
- Caballo C, Escolar G, Diaz-Ricart M, Lopez-Vílchez I, Lozano M, Cid J, et al. Impact of experimental haemodilution on platelet function, thrombin generation and clot firmness: effects of different coagulation factor concentrates. Blood Transfus. 2013;11:391-9.
- Ranucci M, Di Dedda U, Isgrò G, Giamberti A, Cotza M, Cornara N, et al. Plasma-Free Strategy for Cardiac Surgery with Cardiopulmonary Bypass in Infants < 10 kg: A Retrospective, Propensity-Matched Study. J Clin Med. 2023;12.
- Lee JW, Yoo YC, Park HK, Bang SO, Lee KY, Bai SJ. Fresh frozen plasma in pump priming for congenital heart surgery: evaluation of effects on postoperative coagulation profiles using a fibrinogen assay and rotational thromboelastometry. Yonsei Med J. 2013;54:752-62.
- Surabhi S, Kumar M. Comparison of ringer’s lactate and plasmalyt-a as cardiopulmonary bypass prime for bypass associated acidosis in valve replacement surgeries. Ann Card Anaesth. 2021;24:36-41.
- Rudloff E, Hopper K. Crystalloid and Colloid Compositions and Their Impact. Front Vet Sci. 2021;8:639848.
- Weinberg L, Collins N, Van Mourik K, Tan C, Bellomo R. Plasma-Lyte 148: A clinical review. World J Crit Care Med. 2016;5:235-50.
- Noritomi DT, Pereira AJ, Bugano DD, Rehder PS, Silva E. Impact of Plasma-Lyte pH 7.4 on acid-base status and hemodynamics in a model of controlled hemorrhagic shock. Clinics (Sao Paulo). 2011;66:1969-74.
- Wu BU, Hwang JQ, Gardner TH, Repas K, Delee R, Yu S, et al. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:710-7.e1.
- Dai WB, Chen LK, Qi SY, Pan ZY, Zhang X, Huang LL, et al. Lactated Ringer’s solution versus normal saline in pediatric living-donor liver transplantation: A matched retrospective cohort study. Paediatr Anaesth. 2021;31:702-12.
- Liskaser FJ, Bellomo R, Hayhoe M, Story D, Poustie S, Smith B, et al. Role of pump prime in the etiology and pathogenesis of cardiopulmonary bypass-associated acidosis. Anesthesiology. 2000;93:1170-3.
- Teloh JK, Dohle DS, Sönmez S, Tsagakis K, Verhaegh R, Petersen M, et al. Transient dilutional acidosis but no lactic acidosis upon cardiopulmonary bypass in patients undergoing coronary artery bypass grafting. Arch Med Sci. 2017;13:585-90.


