Поражение сердца и роль ультразвукового исследования в условиях пандемии COVID-19
Автор: Павлюкова Е.Н., Скидан В.И., Россейкин Е.В., Нарциссова Г.П., Карпов Р.С.
Журнал: Сибирский журнал клинической и экспериментальной медицины @cardiotomsk
Рубрика: Обзоры и лекции
Статья в выпуске: 1 т.36, 2021 года.
Бесплатный доступ
Обзор литературы касается поражения сердца при COVID-19. Представлен протокол ультразвукового исследования «point-of-care ultrasound (POCUS)» для пациентов с COVID-19. Показана целесообразность оценки механики левого (ЛЖ) и правого желудочков (ПЖ) у больных COVID-19.
Covid-19, поражение сердца, миокардит, эхокардиография, правый желудочек, глобальная деформация правого желудочка, глобальная деформация левого желудочка, протокол ультразвукового исследования
Короткий адрес: https://sciup.org/149136638
IDR: 149136638 | УДК: 616.12-073.432.1:[616.98:578.834.1-036.21] | DOI: 10.29001/2073-8552-2021-36-1-38-48
Текст обзорной статьи Поражение сердца и роль ультразвукового исследования в условиях пандемии COVID-19
УДК 616.12-073.432.1:[616.98:578.834.1-036.21]
Всемирное медицинское сообщество в конце 2019 г. было поставлено перед фактом начала пандемии новой инфекции, обусловленной выявленным штаммом коронавирусов SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2), который вызывает опасное инфекционное заболевание COronaVIrus Disease 2019 (COVID-19). Согласно глобальной статистике, на 20 октября 2020 г. в мире выявлено 40 млн 649 тыс. 793 больных COVID-19, летальность составила 1 млн 125 тыс. 538 случаев [1].
Мишенью при инфицировании клетки хозяина становится ангиотензинпревращающий фермент 2 (АПФ2). Механизм связан с фиксацией SARS-CoV-2 на поверхности клетки с помощью белка-«шип» (spike, S-белок) и взаимодействием с экзопептидазой рецептора АПФ2. Фермент отщепляет аминокислоту от ангиотензина II типа и тем самым меняет его свойства, при этом получившаяся молекула оказывает сосудосуживающий эффект, патогномоничный при остром респираторном дистресс-син-дроме (РДС). Высокая экспрессия АПФ2 характерна для легочной ткани на уровне альвеолоцитов II типа, эндотелия сосудов, эндокарда и миокарда сердца, клубочковой и выделительной систем почек, эпителия кишечника, при этом высока вероятность полиорганного поражения и ассоциированного риска неблагоприятных исходов. Вместе с тем отмечено, что SARS-CoV-2 в основном поражает альвеолярные эпителиальные клетки, что приводит к проявлению респираторных симптомов [2–5].
Для клинической картины COVID-19 характерны фебрильная температура – 88%, утомляемость – 38–40%, продуктивный кашель – 33%, одышка – 19%, миалгия – 11– 15%, головная боль – 14%, боли в горле – 13%, слабость – 11%, диарея – 4–11%, выделения из носа – 5%, тошнота и рвота – 5%, аносмия – 33,9–68% с преобладанием у женщин [3, 4, 6, 7].
Заболевание имеет легкое (80%), среднетяжелое (15%) и критически тяжелое течение (5% пациентов). Особенностью COVID-19 является быстрое утяжеление клинической картины, сопровождающееся лихорадкой и развитием двусторонней пневмонии со снижением индекса оксигенации (paO2/FiO2) менее 300 мм рт. ст. или сатурации крови кислородом (SpO2) менее 93% в сочетании c полиорганным поражением, что обусловливает высокий показатель по шкале SOFA (Sequential Organ Failure Assessment) и летальность от 1 до 5% в условиях общемировой статистики смертности от COVID-19 [5, 8–14].
Основными причинами смерти при COVID-19 являются в 53% случаев дыхательная недостаточность, в 33% – сочетание дыхательной и сердечной недостаточности
(СН), у 7% пациентов – острая декомпенсированная СН. Неблагоприятные исходы заболевания зависят от возраста, течения заболевания и вовлечения в процесс поражения инфекцией сердца, печени и почек [3–6, 8–14].
Цель данного обзора: раскрыть и сосредоточить внимание на поражении сердца при COVID-19, показать роль эхокардиографии (ЭхоКГ) у данной категории пациентов.
Повреждение сердца, обусловленное COVID-19, отмечается у 14–30% больных [8, 15, 16]. В регрессионной модели Кокса у пациентов (n = 416) c COVID-19 и признаками поражения сердца в сравнении с больными, не имевшими поражения сердца, был выявлен более высокий риск смерти как в течение времени с момента появления симптомов (отношение рисков 4,26 [95% ДИ 1,92–9,49]), так и от поступления до конечной точки (отношение рисков 3,41 [95% ДИ 1,62–7,16]) [15].
Поражение сердца обусловливается рядом факторов. Во-первых, это прямое вирусное повреждение миокарда, о наличии которого свидетельствуют повышенные уровни Тропонина T или I. По данным D. Wang с соавт. [16], при наблюдении за 138 пациентами, заболевшими COVID-19, у 36 (7,2%) больных было диагностировано острое повреждение миокарда с повышением уровня высокочувствительного Tропонина I. В наблюдении Т. Guo и соавт. [17] за 187 больными COVID-19 было выявлено повреждение миокарда с повышением уровня Тропонина Т у 52 (27,8%) пациентов, при этом смертность была выше в группе лиц с высоким уровнем Тропонина T и с коморбидными состояниями по сравнению с группой пациентов с нормальным уровнем Тропонина T (59,6 против 8,9%). По мнению ряда исследователей [18, 19], в 7% случаев миокардит, обусловленный COVID-19, явился причиной смерти. Острое повреждение миокарда при COVID-19 ассоциировано со снижением функции левого (ЛЖ) и правого желудочков (ПЖ), жизнеугрожающими аритмиями и высоким уровнем Тропонина [17].
Хотя ряд публикаций, касающихся наличия миокардита при COVID-19, предоставляют доказательства присутствия воспаления в сердечной мышце, не раскрывается механизм его возникновения [20]. Данные аутопсии продемонстрировали воспалительные инфильтраты, состоящие из макрофагов и в меньшей степени CD4+ Т-клеток [13, 21]. Эти мононуклеарные инфильтраты были связаны с участками некроза кардиомиоцитов, что, согласно критериям Далласа, укладывалось в клинику миокардита [22, 23]. Однако нет данных, показавших присутствие SARS-CoV-2 в ткани миокарда. Посмертный анализ полимеразной цепной реакции сердечной ткани обнаружил вирусный геном только у 35% пациентов (у 7 из 20 больных), умерших от атипичной пневмонии. Следует отметить, что в ткани сердечной мышцы этих больных были снижены уровни АПФ2, наблюдалась гипертрофия миокарда [24].
Во-вторых, патологический системный воспалительный ответ, который проявляется «цитокиновым штормом», реализуется через дисбаланс ответа Т-хелперов 1-го и 2-го типа, а снижение экспрессии АПФ2 и дисрегу-ляция ренин-ангиотензиновой системы (РАС) запускают каскад механизмов повреждения миокарда и проводящей системы сердца [24]. Высказана гипотеза о наличии «брадикининового шторма». Хотя учитывая индукцию интерлейкина 2 с помощью брадикинина, эти два явления («цитокиновый» и «брадикининовый шторм») могут быть тесно связаны [25]. Избыток брадикинина может привести к гипокалиемии и обусловить развитие аритмий. Согласно публикации [25], гипокалиемия возникает в тяжелых случаях COVID-19.
Вместе с тем окислительный стресс, внутриклеточный ацидоз и повреждение митохондрий приводят к дыхательной дисфункции и гипоксии клетки, что реализуется повреждением кардиомиоцитов. В свою очередь прямое повреждающее действие вируса на эндотелий малых артерий связано с микроваскулярным повреждением, в результате чего возникают гипоперфузия, повышенная сосудистая проницаемость и манифестный ангиоспазм. В отдаленном периоде после перенесенной инфекции SARS-CoV можно ожидать метаболических изменений в миокарде [5, 6, 8, 15, 18]. Согласно данным C. Huang и соавт. [15], высокие уровни интерлейкина1-бета, интерферона гамма (IFN-gamma), моноцитарного хемотаксического белка 1 (MCP-1) и интерферона-гамма индуци-бельного протеина 10 (IP-10) наблюдались у пациентов, находившихся в отделении интенсивной терапии. Персистирующий воспалительный статус у пациентов с тяжелой и критической степенью тяжести COVID-19 действует как важный триггер для каскада коагуляции, в частности интерлейкин-6, с активированием свертывания крови и подавлением фибринолитической системы. Нельзя исключить, что вследствие прямого воздействия вируса происходит повреждение эндотелия сосудов легких и периферических сосудов, что также является важным индуктором гиперкоагуляции, как и агрессивный иммунный ответ. Появление антифосфолипидных антител может усиливать коагулопатию.
У больных COVID-19 может развиться острый инфаркт миокарда (ОИМ). Истинная частота развития инфаркта миокарда пока не ясна. Нельзя исключить, что у больных ишемической болезнью сердца (ИБС) инфекция может вызвать как инфаркт миокарда 1-го типа, так и инфаркт миокарда 2-го типа. Согласно данным О.В. Зайратьянц и соавт. [26], среди умерших от COVID-19 в г. Москве с 20 марта по 22 мая 2020 г. ( n = 2000) частота инфаркта миокарда составила 1,1%. По данным патологоанатомических исследований, тромбоз коронарных артерий при отсутствии нестабильных атеросклеротических бляшек был выявлен в 1,8% случаев, у части больных мелкоочаговый или трансмуральный инфаркт миокарда вследствие вирусного повреждения стенки коронарной артерии [8, 9, 11, 26]. Не редкость обнаружение пристеночных тромбов в полостях сердца (рис. 1), чаще в ПЖ и предсердиях [26, 27]. На основании результатов проведенных вскрытий больных COVID-19 О.В. Зайратьянц и соавт.
предложили выделять «сердечную маску» COVID-19 [26].
Предполагается, что эмоциональный стресс, высокий уровень катехоламинов, усиленный воспалительный ответ и прямая вирусная цитотоксичность могут быть механизмами развития синдрома Такоцубо при COVID-19 [28, 29]. Заболевание в семье, госпитализация члена семьи по поводу пневмонии могут представлять собой дополнительный фактор, способный значительно увеличить активацию симпатикотонии и развитие синдрома Такоцу-бо. На сегодняшний день описано 16 клинических случаев синдрома Такоцубо на фоне заболевания COVID-19. У одного пациента гипокинез верхушки развился только после интубации и перикардиоцентеза [28, 30]. Выпот в перикард мог быть следствием системного воспаления и прямого вирусного воздействия [28, 29]. Смертность среди пациентов с синдромом Такоцубо составила 56% [27]. Согласно публикациям [28–31], у больных COVID-19 и имевших синдром Такоцубо не обнаружено лимфоцитарного миокардита по данным биопсии эндомиокарда. Только в сообщении S. Sala и соавт. [31] в биоптатах эндомиокарда были отмечены диффузные воспалительные инфильтраты Т-лимфоцитов (CD3+ > 7/мм2) с выраженным интерстициальным отеком и ограниченными очагами некроза у пациентки в возрасте 63 лет на 7-е сут заболевания. Заместительного фиброза не было выявлено, и это свидетельствовало об остром воспалительном процессе. Молекулярный анализ показал отсутствие генома SARS-CoV-2 в миокарде.
Гипоксемия вследствие тяжелой пневмонии может привести к повреждению миокарда, анаэробиозу, ацидозу, повышению свободных радикалов, реактивного кислорода и разрушению фосфолипидного слоя мембран кардиомиоцитов. Необходимо отметить и тот факт, что повышение уровней катехоламинов, вызванное тревогой пациента, и побочные действия лекарственных препаратов, назначенных при COVID-19, могут обусловить повреждение миокарда [32, 33].
Больные с коморбидными заболеваниями, в частности ранее установленной ИБС, артериальной гипертонией (АГ), врожденными и приобретенными пороками сердца на момент заражения COVID-19, наиболее восприимчивы к повреждению миокарда, вызванного воспалением, снижением контрактильного резерва. Метаанализ 1527 пациентов показал, что АГ, ИБС и сахарный диабет имели место у 17,1; 16,4 и 9,7% больных COVID-19 соответственно [32]. Cогласно данным литературы [32–34], у больных с ранее доказанной ИБС риск развития смерти значительно выше по сравнению с пациентами, не имевшими патологии коронарных артерий. Среди пациентов, находившихся в реанимационном отделении, коморбидные заболевания отмечались у 16,7% больных [34]. Коморбидное заболевание и повышенный уровень Тропонина Т были связаны с высокой смертностью (69,4%) по сравнению со смертностью среди лиц с повышенным уровнем Tропонина Т и без коморбидного состояния (37,5%). Смертность при наличии сопутствующих сердечно-сосудистых заболеваний без повышения Тропонина T составила 13,3% по сравнению со смертностью (7,6%) среди пациентов, не имевших сопутствующих сердечно-сосудистых заболеваний и повышения Tропонина T при поступлении в стационар по поводу COVID-19 [17]. Важно отметить, что у больных с комор-бидными состояниями значительно чаще отмечалось повышение уровня Тропонина T.
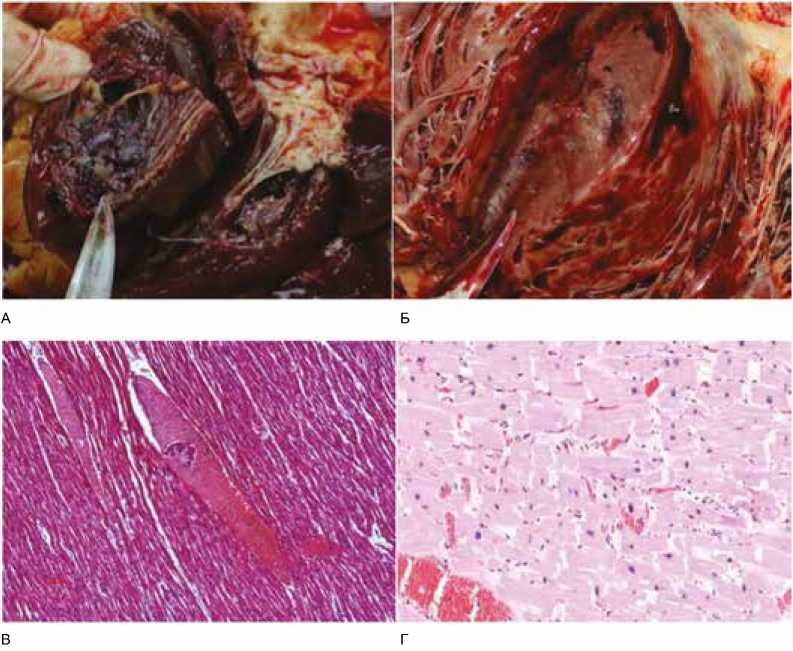
Рис. 1. А – крупный пристеночный тромб в правом желудочке, Б – интрамуральные кровоизлияния в миокарде и очаги некроза миокарда левого желудочка, В – гипертрофия, дистрофические изменения, фрагментация и некроз отдельных кардиомиоцитов (гипоксические, ишемические, метаболические нарушения), полнокровие сосудистого микроциркуляторного русла, Г – гипертрофия, дистрофические изменения, волнообразный ход и некроз отдельных кардиомиоцитов, фибрин, эритроциты в просвете и набухание эндотелия венулы. Окраска гематоксилином и эозином, увеличение х100 [заимствовано из 24]
Fig. 1. A – large parietal thrombus in the right ventricle; Б – intramural hemorrhages in the myocardium and foci of necrosis in the left ventricular myocardium; B – hypertrophy, dystrophic changes, fragmentation and necrosis of individual cardiomyocytes (hypoxic, ischemic, metabolic disorders), and plethora of the vascular microvasculature; Г – hypertrophy, dystrophic changes, undulating course and necrosis of individual cardiomyocytes, fibrin, erythrocytes in the lumen and swelling of the venule endothelium. Hematoxylin and eosin staining, x100 magnification [borrowed from 24]
В ряде публикаций [32, 35–37] были высказаны опасения по поводу повышенного риска заболеваемости и смертности от COVID-19 у больных, принимавших ингибиторы ренин-ангиотензин-альдостероновой системы. Предполагалось, что у пациентов с АГ взаимосвязь между ферментом АПФ2 и COVID-19 усиливает тяжесть заболевания [32, 35–37], поскольку проводимая терапия АГ ингибиторами АПФ (иАПФ) могла оказывать влияние на связывание SARS-CoV-2 с АПФ2, способствуя развитию заболевания [37]. Это было основано на экспериментальных данных, показавших, что ингибиторы РАС вызывают компенсаторное повышение уровней АПФ2 в тканях [38]. Высказывалось предположение, что назначение иАПФ может быть нецелесообразным при COVID-19 [39]. Однако важно подчеркнуть тот факт, что на сегодняшний день нет четких доказательств того, что использование иАПФ или блокаторов рецепторов ангиотензина (БРА) приводит к усилению регуляции АПФ2 в тканях человека. В эксперименте показано потенциально защитное влияние БРА [39, 40]. В соответствии с отечественными рекомендациями пациенты, принимающие иАПФ или БРА, не должны прекращать свое лечение [41–43]. На сайте Европейского общества кардиологов от 20 ноября 2020 г. были опубликованы данные Шведского национального регистра пациентов с АГ, СН, сахарным диабетом, заболеваниями почек и ИБС о связи приема препаратов ингибиторов ренин-ангиотензин-альдостероновой системы с риском госпитализации/смерти от COVID-19 в общей популяции и смертности от всех причин в случаях COVID-19. Установлено, что в когорте, включавшей 1,4 млн человек, использование препаратов ингибиторов ренин-ангиотен-зин-альдостероновой системы не связано с повышенным риском госпитализаций или смерти от COVID-19 [].
Больные с приобретенными пороками клапанов сердца подвергаются большему риску осложнений по сравнению с пациентами, не имевшими клапанного порока [33]. При определении приоритетности хирургических вмешательств необходимо оценивать краткосрочный клинический прогноз с риском заражения внутрибольничной инфекцией. Мы полагаем, что в данной ситуации лучше отдавать предпочтение транскатетерной имплантации аортального клапана или клипированию митрального клапана, поскольку данные технологии лечения сокращают пребывание пациентов в стационаре [33, 44].
К сожалению, нами не найдено публикаций, касающихся состояния пациентов с врожденными пороками сердца (ВПС) при COVID-19. Не вызывает сомнения тот факт, что эта категория пациентов подвержена большему риску осложнений. На основании классификации анатомии и физиологической стадии ВПС больные с анатомической стадией III или физиологической стадией B, C или D должны рассматриваться как группы высокого риска осложнений COVID-19 из-за пониженного функционального резерва [33, 45]. Проблема, созданная пандемией COVID-19, заключается в лечении пациентов с СН, находящихся в списке ожидания трансплантации сердца, что обязывает врачей учитывать риски отсрочки трансплантации по сравнению с ранним хирургическим вмешательством и пытаться сохранить безопасность пациентов после трансплантации сердца.
На основании вышеизложенного можно указать варианты повреждения миокарда:
– миокардит, включая развитие фульминантного миокардита;
– инфаркт миокарда 1-го и 2-го типа;
– синдром Такоцубо;
– неишемическое повреждение миокарда, обусловленное микрососудистой дисфункцией в результате диффузного микротромбоза и повреждения малых сосудов.
У пациентов с COVID-19 могут развиваться аритмии, от тахикардии и брадикардии до асистолии. Согласно эпидемиологическим данным, сердцебиение присутствует у 7,3% пациентов [46]. Аритмии у этой группы пациентов могут возникать вследствие гипоксемии, метаболических нарушений и миокардита [20].
Острая декомпенсация хронической СН (ХСН), связанная с повышением давления в левом предсердии и развитием выраженной легочной гипертензии, обусловливает развитие отека легких на фоне COVID-19. Этому способствуют перегрузка объемом при нарушении контроля за приемом жидкости на фоне лихорадки, пароксизмы суправентрикулярной тахиаритмии. Снижение сократительной способности миокарда с повышением конечного диастолического давления в ЛЖ, давления заклинивания в легочных капиллярах и давления в левом предсердии приводит к увеличению объема левого предсердия, повышению систолического давления в легочной артерии (ЛА) и усугублению тяжести относительной митральной недостаточности [5, 17].
Пациенты с СН составляют многочисленную группу риска тяжелого течения и летальности при COVID-19. СН наблюдалась у 23% пациентов с COVID-19 и встречалась чаще у умерших больных по сравнению с выжившими (51,9 против 11,7%) [17, 47]. У больных COVID-19, находившихся в реанимации или отделении интенсивной терапии, СН наблюдалась в 42% случаев. При этом у 67% пациентов в дальнейшем появилась потребность в вазопрессорной поддержке, у 72% в среднем через 1,5 дня от госпитализации – потребность в искусственной вентиляции легких [47–50].
Нарушения функции ПЖ при COVID-19 наблюдаются при миокардите, РДС, синдроме Такоцубо, тромбоэмболии легочной артерии (ТЭЛА) и декомпенсации ХСН с развитием острой декомпенсации СН [12]. Дисфункция ПЖ может встречаться при сохраненной фракции выброса (ФВ) ЛЖ у больных COVID-19, имевших повышенный уровень Тропонина [50]. Наряду с ТЭЛА, гипоксическая вазоконстрикция и уменьшение объема легких, чрезмерно положительное давление в конце выдоха, гиперкапния, применение α-агонистов, повышенное давление в левом предсердии обусловливают развитие высокого легочного сопротивления и, как следствие, острой правожелудочковой декомпенсации [51]. Низкий уровень насыщения кислородом, высокое давление наполнения в ЛЖ и повышенные уровни биомаркеров (D-димера, натрийуретического пептида, Тропонина и C-реактивного белка) позволяют думать о высоком легочном сопротивлении, обусловленном паренхиматозными изменениями легких, повышенном давлении в левом предсердии [51]. В этих случаях выявляются более высокие уровни натрийуретических пептидов, интерлейкина 6, D-димеров, лактатдегидрогеназы, ферритина, фибриногена, высокочувствительного С-реактивного белка [52]. Ряд исследователей [52] предлагают использовать вышеуказанные изменения показателей в качестве маркеров стратификации риска и прогноза течения инфекции. Маркерами неблагоприятного исхода служат лимфопения, повышенные уровни ферритина, интерлейкина 6, D-димера [32]. Клиника нарастающей острой декомпенсации СН предполагает определение мозгового натрийуретического пептида (NT-proBNP) [16, 47, 52]. Значение NT-proBNP более 2000 пг/мл свидетельствует о наивысшем риске и необходимости госпитализации в отделение интенсивной терапии. При уровне NT-proBNP от 400 до 2000 пг/мл пациенты оцениваются как имеющие промежуточный риск, и этой категории больных показано выполнение эхокардиографии (ЭхоКГ). У пациентов с уровнями NT-proBNP от 400 до 2000 пг/мл отмечен гипокинетический тип гемодинамики с исходным значительным снижением производительности сердца. Сердечный индекс не превышал 2,2 л/мин/м2 у многих больных ХСН, имевших III функциональный класс СН до развития декомпенсации [53].
Проведение ЭхоКГ у пациентов с COVID-19 следует ограничить случаями, когда результаты исследования предположительно могут повлиять на исход заболевания и установить механизм повреждения сердца [54]. Выполнение исследования целесообразно только по показаниям при условии, что результаты исследования обеспечат клиническую пользу и не приведут к ухудшению состояния пациента. ЭхоКГ назначается при значительном повышении уровней Тропонина (Т или I) и натрийуретического пептида, нарушениях ритма сердца или проводимости, шоковом состоянии или острой СН, а также в случае стойкой гемодинамически значимой аритмии [8, 32, 53]. Не рекомендовано рутинное выполнение ЭхоКГ в условиях пандемии COVID-19. Трансторакальная ЭхоКГ должна выполняться только по клиническим показаниям, чтобы свести к минимуму риск распространения инфекции COVID-19.
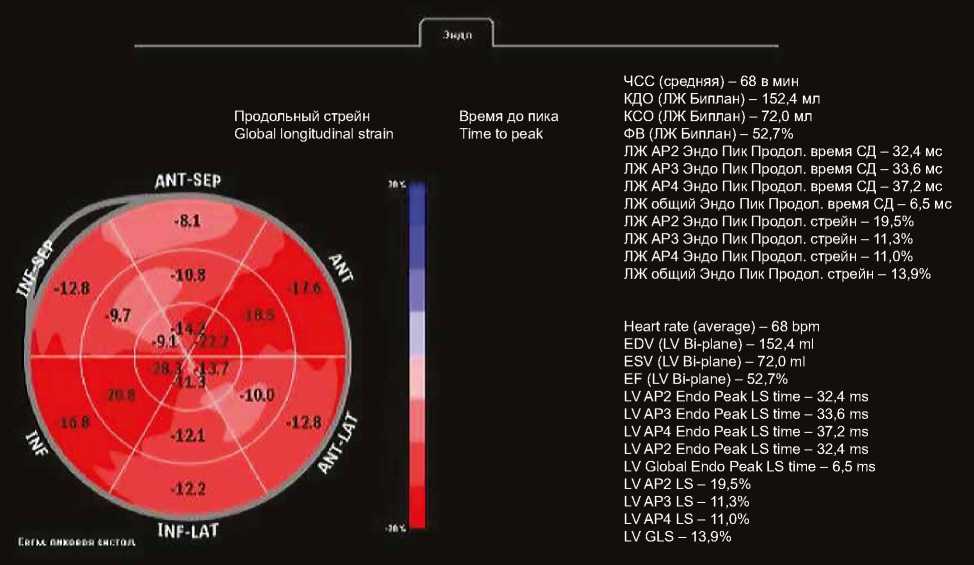
По данным Y.C. Szekely и соавт. [51], систолическая дисфункция ЛЖ выявляется в 10% случаев среди пациентов с COVID-19. У 32% больных значения параметров стандартной ЭхоКГ не имеют отклонений. Диастолическая дисфункция ЛЖ зарегистрирована в 16% случаев [51]. Выпот в перикард выявляется у 23% больных с тяжелым течением заболевания [55]. Критерием повреждения миокарда может быть не только снижение ФВ, но и снижение глобальной либо сегментарной деформации ЛЖ и ПЖ в продольном направлении (Global Longitudinal Strain – GLS) [56]. Несмотря на нормальные значения ФВ ЛЖ у больных с COVID-19 наблюдается снижение глобальной и сегментарной деформации ЛЖ в продольном направлении [56–59]. Значение глобальной деформации ЛЖ в продольном направлении менее –15% (в абсолютном значении) является независимым. предиктором смерт- ности с чувствительностью и специфичностью этого показателя 77 и 75% соответственно [57]. В исследовании S. Stöbe и соавт. нарушение контрактильности ЛЖ в виде снижения деформации в продольном, радиальном направлениях и по окружности наблюдалось в базальных сегментах нижней и переднебоковой стенки ЛЖ в 71, 36
и 43% случаев соответственно [57]. В данной публикации мы показываем «мозаичное» изменение деформации ЛЖ в продольном направлении у пациента с COVID-19 и острым РДС, имевшего повышенные уровни креатинки-назы МB, с ФВ ЛЖ 50% на раннем сроке течения инфекционного процесса (рис. 2).
ANT-SEP
Время до пика Time to peak
Продольный стрейн
Global longitudinal strain
ЧСС (средняя) – 68 в мин
КДО (ЛЖ Биплан) – 152,4 мл
КСО (ЛЖ Биплан) – 72,0 мл
ФВ (ЛЖ Биплан) – 52,7%
ЛЖ АР2 Эндо Пик Продол. время СД – 32,4 мс
ЛЖ АР3 Эндо Пик Продол. время СД – 33,6 мс
ЛЖ АР4 Эндо Пик Продол. время СД – 37,2 мс
ЛЖ общий Эндо Пик Продол. время СД – 6,5 мс
ЛЖ АР2 Эндо Пик Продол. стрейн – 19,5%
ЛЖ АР3 Эндо Пик Продол. стрейн – 11,3%
ЛЖ АР4 Эндо Пик Продол. стрейн – 11,0%
ЛЖ общий Эндо Пик Продол. стрейн – 13,9%
Heart rate (average) – 68 bpm EDV (LV Bi-plane) – 152,4 ml ESV (LV Bi-plane) – 72,0 ml EF (LV Bi-plane) – 52,7%
LV AP2 Endo Peak LS time – 32,4 ms
LV AP3 Endo Peak LS time – 33,6 ms
LV AP4 Endo Peak LS time – 37,2 ms
LV AP2 Endo Peak LS time – 32,4 ms
LV Global Endo Peak LS time – 6,5 ms
LV AP2 LS – 19,5%
LV AP3 LS – 11,3%
LV AP4 LS – 11,0%
LV GLS – 13,9%
INF-LAT
Сйол пиковьи «исток
Рис. 2. Пациент с COVID-19 на 10-е сут заболевания, среднетяжелое течение. ФВ ЛЖ = 49%. Снижение глобальной деформации левого желудочка в продольном направлении (GLS = –14%), «мозаичный» характер снижения деформации по сегментам
Fig. 2. A patient with COVID-19 on day 10 of the disease, moderate-severe course. LVEF = 49%. Decrease in the LV Global Longitudinal Strain
(GLS = –14%), mosaic strain reduction in segments
Описано снижение вращения ЛЖ на уровне базальных сегментов вплоть до его отсутствия у 43% больных COVID-19. В 57% случаев кривая скручивания была двухфазной с максимумом в период ранней диастолы [58].
Согласно имеющимся публикациям, у пациентов с COVID-19 наблюдается увеличение размеров ПЖ, систолического и среднего давления в ЛА, степени трикуспидальной регургитации и снижение экскурсии движения фиброзного кольца (ФК) трикуспидального клапана (ТК) на стороне свободной стенки ПЖ (TAPSE) [59, 60]. Дилатация полости ПЖ ассоциирована с повышением уровней D-димера и Тропонина I [61]. В ответ на РДС, который был диагностирован у 29–67% больных СOVID-19 [61], отмечалось увеличение выходного тракта и снижение контрактильности ПЖ. Множественный линейный регрессионный анализ показал, что ФВ ЛЖ, диаметр правого предсердия, уровень Тропонина I, D-димер и систолическое давление в ЛА были независимыми предикторами дилатации ПЖ [55].
Для оценки систолической функции ПЖ используются показатели TAPSE, скорость движения ФК ТК на стороне свободной стенки ПЖ или скорость движения базального сегмента свободной стенки ПЖ (St) при наличии режима тканевого допплеровского режима процент изменения площади полости ПЖ (FAC). Вместе с тем показатель FAC зависим от качества серошкального изображения эндокарда и недостаточно хорошо воспроизводим при внутри- и межоператорском исследовании. Глобальная деформация ПЖ в продольном направлении более целесообразна в оценке функции ПЖ, поскольку ее значения воспроизводимы, а ее снижение свидетельствует о субклинической систолической дисфункции ПЖ. Согласно данным Y. Li и соавт. [61], показатели глобальной деформации ПЖ в продольном направлении, TAPSE и процент изменения площади полости ПЖ (FAC) были прогностическими критериями выживаемости больных COVID-19. Однако площадь под кривой для глобальной деформации ПЖ в продольном направлении (0,87) была большей по сравнению с FAC (0,72; p = 0,028) и TAPSE (0,67; p = 0,002). Предикторами высокой смертности являлись пороговые значения показателей для FAC 43,5% и TAPSE 23 мм. Пороговое значение глобальной деформации ПЖ в продольном направлении как прогностического маркера повышенной смертности составило –23% и ниже (в абсолютных значениях) с чувствительностью и специфичностью этого критерия 94,4 и 64,7% соответственно. Y. Li и соавт. [61] продемонстрировали, что смертность среди пациентов при значениях глобальной деформации ПЖ менее –20,5% была выше по сравнению с лицами, имевшими нормальные значения деформации ПЖ. Согласно O.F. Baycan и соавт. [56], значение глобальной деформации ПЖ –18,45% и ниже (в абсолютных значениях) является независимым предиктором внутрибольничной смертности у пациентов с COVID-19.
При проведении ЭхоКГ целесообразно применение коротких протоколов, фокусированных на проблемную зону [62], которые основаны на использовании следующих модальностей:
-
1. Модифицированная и фокусированная парастернальная позиция по короткой (SAX) и длинной оси (LAX):
– длинник и поперечник полости ПЖ на уровне 4 камер, апикальная позиция.
– систолическая функция ПЖ – визуально, оценка TAPSE.
– движение межжелудочковой перегородки и межжелудочковое взаимодействие.
-
2. Допплеровские режимы в стандартных позициях:
– тяжесть трикуспидальной регургитации (TR severity);
– расчет систолического давления в ЛА (PASP);
– ограничения визуализации ЛА на фоне изменений в легких.
-
3. Оценка коллабирования нижней полой вены (НПВ): – расчет давления в правом предсердии (RAP).
-
4. Наличие признака (McConnell’s sings) регионарной картины острой дисфункции ПЖ, проявляющейся в акинезии среднего сегмента свободной стенки ПЖ с сохраненной апикальной сократимостью.
-
5. Оценка наличия тромбоза правых камер сердца (пристеночный, транзитный), функционирующее овальное окно.
-
6. Наличие выпота в полости перикарда.
-
7. Постобработка изображений с определением изменения площади ПЖ (FAC), глобальной деформации ПЖ в продольном направлении (LGS RV) и свободной стенки ПЖ (GLS Wall RV).
Американской ассоциацией специалистов по эхокардиографии (ASE) предложено использовать протокол Point-of-Care Ultrasound (POCUS) у больных COVID-19, который позволяет получить быструю оценку поражения легких, вовлечения сердца и сосудов в патологический процесс. У пациентов с SARS-CoV-2, где манифестирует тяжелый острый респираторный синдром, выполнение исследования по протоколу POCUS помогает определить целесообразность проведения компьютерной томографии легких и магнитно-резонансной томографии сердца. Протокол POCUS включает три основные позиции сердца, включая субкостальный доступ для оценки коллабирования НПВ, оценку выпота в полость перикард; стандартные зоны локации легких для выявления А и В линий, плеврального выпота и признаков консолидации легочной ткани (рис. 3).
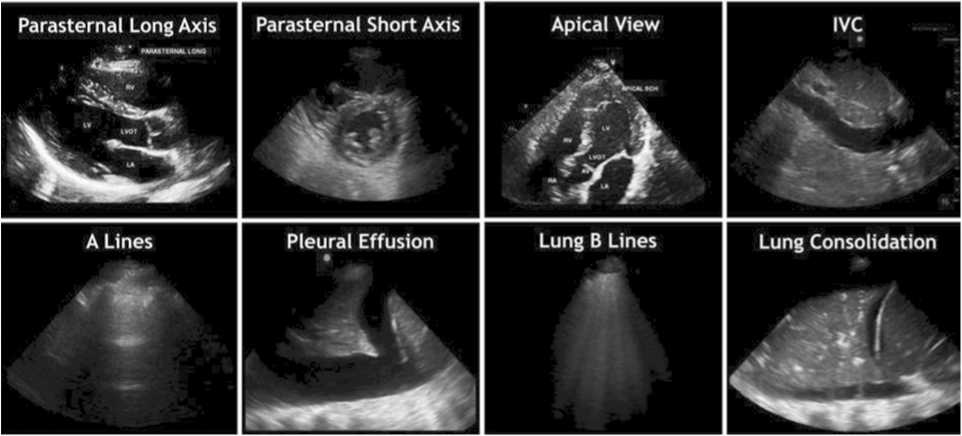
Рис. 3. Доступы визуализации при подозрении или подтвержденном COVID-19, согласно протоколу POCUS
Fig. 3. Visualization accesses in case of suspected or confirmed COVID-19 according to the POCUS protocol
Показания для использования протокола Cardiac POCUS:
-
1. Выявление и определение предшествующей кардиоваскулярной патологии.
-
2. Ранняя идентификация снижения сократительной функции миокарда, несмотря на ранее диагностированное заболевание.
-
3. Мониторинг и обследование: POCUS может использоваться при подозрении на нарушение кардиопульмональной функции во время рутинного обследования сердца и легких с помощью аускультации.
-
4. Определение нарушений сердечно-сосудистой системы потенциально ассоциируется с COVID-19: ранние работы демонстрируют, что у некоторых пациентов появление а) перикардиального выпота и/или миокардита может прогрессировать до шока; б) гиперкоагуляция может быть ассоциирована с тромбозом вен нижних конечностей и ТЭЛА, что сопровождается нарушением функции ПЖ и легочной гипертензией; с) систолическая дисфункция ЛЖ (глобальная и регионарная) может ассоциироваться с миокардитом, стресс-индуцированной кардиомиопатией, эпикардиальным или микроваскулярным коронарным тромбозом.
Таблица. Протокол АSE POCUS при подозрении или подтвержденном COVID-19. Модифицированный протокол POCUS для оценки больных COVID-19, включающий визуализацию сердца, легких и сосудов [63, 64]
Table. АSE POCUS Protocol for suspected or confirmed COVID-19. Modified POCUS Protocol for the examination of COVID-19 patients, including imaging of the heart, lungs, and blood vessels [63, 64]
|
POCUS СOVID 19 |
Визуализация структуры Structure imaging |
Оценка Assessments |
Заболевание Disease |
|
Левый желудочек Left ventricle |
Размеры, глобальная и региональная функция Dimensions, global and regional function |
Миокардит ОИМ Кардиогенный шок Кадиомиопатия Myocarditis AMI Cardiogenic shock Cadiomyopathy |
|
|
Правый желудочек Right ventricle |
Размеры и функция, градиент ТР, расчетное систолическое давление в ЛА Dimensions and function, TR gradient, calculated systolic pressure in the PA |
ТЭЛА Кардиомиопатия PATE Cardiomyopathy |
|
|
Перикард Pericardium |
Объем выпота Effusion volume |
Тампонада Tamponade |
|
|
Сосуды Blood vessels |
Степень регургитации и стеноза Degree of regurgitation and stenosis |
Существующие ранее кардиоваскулярные заболевания Preexisting cardiovascular disease |
|
|
В-линии, скольжение плевры в норме B-lines; pleural slip is normal |
|||
|
Отек или пневмония Odema or pneumonia |
|||
|
Субплевральная консолидация, утолщение плевры Subpleural consolidation, pleural thickening |
Пневмония РДС Pneumonia RDS |
||
|
8 или 12 позиций |
Долевая консолидация с воздушной бронхограммой Lobar consolidation with air bronchogram |
Пневмония РДС Pneumonia RDS |
|
|
для визуализации 8 or 12 positions for visualization |
Выпот Effusion |
ХСН HF |
|
|
Пульсация ЯВ и субкостальный доступ к НПВ Pulsation of the ulcer and subcostal access to the IVC |
|||
|
Статус волемии Volemia status |
ХСН, гиповолемия CHF, hypovolemia |
||
|
+/- нижние конечности +/- lower limbs |
2 точки доступа 2 access points |
Тромбоз вен нижних конечностей Vein thrombosis of the lower extremities |
Протокол Lung Pocus необходимо использовать в случае, когда проведение мультиспиральной компьютерной томографии легких лимитировано:
-
1. Lung POCUS при ультразвуковом исследовании легких может использоваться для определения тяжести пневмонии при COVID-19 как дополнение к оксиметрии и физикальному осмотру. Основные характеристики вирусной пневмонии включают в себя: при нетяжелом течении заболевания; а) утолщение и неравномерность плевральной линии; б) В-линии (фокусные, многофокусные и слияние); при тяжелом течении заболевания с) В-линии сливаются с участками консолидации, включая бронхограммы (мультифокальной малой, нелобарной, лобарной с подвижными воздушными бронхограммами).
-
2. Lung POCUS полезен для исключения сопутствующей патологии грудной клетки и легких у тяжелых больных, в случае пневмоторакса или клинически значимого плеврального выпота.
Протокол Vascular POCUS рекомендуют использовать в рамках рекомендаций неотложных состояний:
а) локация НПВ и яремных вен (ЯВ) играет важную роль в оценке гемодинамики критических пациентов. Риск венозных тромбозов увеличивается у пациентов с ограниченной подвижностью. Кроме того, ранние работы отражают связь между протромботическим статусом и COVID-19 [63].
Таким образом, можно констатировать, что системный воспалительный ответ при COVID-19 вызывает повреждение миокарда (миокардит, инфаркт миокарда 1-го и 2-го типов, синдром Такоцубо, микрососудистую дисфункцию), проявляющееся дисфункцией ЛЖ и ПЖ. Использование в практике протоколов визуализации сердца, легких и магистральных сосудов позволяет своевременно определить степень тяжести инфекционного процесса, вовлечение сердца и возможные осложнения. Несмотря на рекомендованные протоколы исследования сердца, мы считаем, что использование оценки деформации ЛЖ и ПЖ является наиболее целесообразным у данной категории пациентов, и это исследование необходимо дополнить во все протоколы POCUS.
Список литературы Поражение сердца и роль ультразвукового исследования в условиях пандемии COVID-19
- Коронавирус. Статистика коронавируса. URL: https://coronavirus-sta-ta.ru/statistika-koronavirusa-v-mire-na-20-oktyabrya-2020-goda/. Coronavirus. Coronavirus statistics (In Russ.). URL: https://coronavi-rus-stata.ru/statistika-koronavirusa-v-mire-na-20-oktyabrya-2020-goda/.
- Yan R., Zhang Y., Li Y., Xia L., Guo Y., Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367(6485):1444-1448. DOI: 10.1126/science.abb2762.
- Временные методические рекомендации. Профилактика, диагностика и лечение новой коронавирусной инфекции (COVID-19)»; версия 8.1 от 01.10.2020. М.: Министерство здравоохранения Российской Федерации; 2020:226.
- Шляхто Е.В., Конради А.О., Виллевальде С.В., Звартау Н., Яковлев А.Н., Соловьева А.Е. и др. Руководство по диагностике и лечению болезней системы кровообращения (БСК) в контексте пандемии COVID-19 (краткая версия). М.; 2020:36.
- Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020;17(5):259-260. DOI: 10.1038/s41569-020-0360-5.
- Clerkin K.J., Fried J.A., Raikhelkar J., Sayer G., Griffin J.M., Ma-soumi A. et al. COVID-19 and cardiovascular disease. Circulation. 2020;141(20):1648-1655. DOI: 10.1161/CIRCULATIONA-HA.120.046941.
- Meng X., Deng Y., Dai Z., Meng Z. COVID-19 and anosmia: A review based on up-to-date knowledge. Am. J. Otolaryngol. 2020;41(5):102581. DOI: 10.1016/j.amjoto.2020.102581.
- Siddiqi H.K., Mehra M.R. COVID-19 illness in native and immunosup-pressed states: A clinical-therapeutic staging proposal. J. Heart Lung Transplant. 2020;39(5):405-407. DOI: 10.1016/j.healun.2020.03.012.
- Grasselli G., Pesenti A., Cecconi M. Critical сare rtilization for the COVID-19 оutbreak in Lombardy, Italy: Early еxperience and forecast during an emergency response. JAMA. 2020;323(16):1545-1546. DOI: 10.1001/jama.2020.4031.
- Bonow R.O., Fonarow G.C., O'Gara P.T., Yancy C.W. Association of сoronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020;5(7):751-753. DOI: 10.1001/jamacar-dio.2020.1105.
- Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. et al.; China Medical Treatment Expert Group for Covid-19. Clinical сЬ^та^^^ of ^ronavirus disease 2019 in China. N. Engl. J. Med. 2020;382(18):1708-1720. DOI: 10.1056/NEJMoa2002032.
- Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C. et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8(4):420-422. DOI: 10.1016/S2213-2600(20)30076-X.
- Alhogbani T. Acute myocarditis associated with novel Middle east respiratory syndrome coronavirus. Ann. Saudi Med. 2016;36(1):78-80. DOI: 10.5144/0256-4947.2016.78.
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. DOI: 10.1016/S0140-6736(20)30183-5.
- Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F. et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802-810. DOI: 10.1001/jamac-ardio.2020.0950.
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. DOI: 10.1001/jama.2020.1585.
- Guo T., Fan Y., Chen M., Wu X., Zhang L., He T. et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811-818. DOI: 10.1001/jamacar-dio.2020.1017.
- Long B., Brady W.J., Koyfman A., Gottlieb M. Cardiovascular complications in COVID-19. Am. J. Emerg. Med. 2020;38(7):1504-1507. DOI: 10.1016/j.ajem.2020.04.048.
- Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846-848. DOI: 10.1007/ s00134-020-05991-x.
- Akhmerov A., Marban E. COVID-19 and the heart. Circ. Res. 2020;126(10):1443-1455. DOI: 10.1161/CIRCRESAHA.120.31.
- Yao X.H., Li T.Y., He Z.C., Ping Y.F., Liu H.W., Yu S.C. et al. A pathological report of three COVID-19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi. 2020;49(5):411-417. DOI: 10.3760/ cma.j.cn112151-20200312-00193.
- Aretz H.T. Myocarditis: The Dallas criteria. Hum. Pathol. 1987;18(6):619-624. DOI: 10.1016/s0046-8177(87)80363-5.
- Fung G., Luo H., Qiu Y., Yang D., McManus B. Myocarditis. Circ. Res. 2016;118(3):496-514. DOI: 10.1161/CIRCRESAHA.115.306573.
- Oudit G.Y., Kassiri Z., Jiang C., Liu P.P., Poutanen S.M., Penninger J.M. et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur. J. Clin. Invest. 2009;39(7):618-625. DOI: 10.1111/j.1365-2362.2009.02153.x.
- Garvin M.R., Alvarez C., Miller J.I., Prates E.T., Walker A.M., Amos B.K. et al. A mechanistic model and therapeutic interventions for COVID-19 involving a RAS-mediated bradykinin storm. Elife. 2020;9:e59177. DOI: 10.7554/eLife.59177.
- Зайратьянц О.В., Самсонова О.В., Михайлева Л.М., Черняев А.Л., Мишнев О.Д., Крупнов Н.М. и др.; под общ ред. О.В. Зайратьянца. Патологическая анатомия COVID-19: атлас. М.; 2020:120. Zairatiants O.V., Samsonova O.V., Mikhailova L.M., Chernyaev A.L., Mishnev O.D., Krupnov N.M. et al.; edit. by O.V. Zayratyants. Pathological anatomy of COVID 19: Atlas. Moscow; 2020:120 (In Russ.).
- Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D., Kant K.M. et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb. Res. 2020;191:148-150. DOI: 10.1016/j. thromres.2020.04.041.
- Desai H.D., Jadeja D.M., Sharma K. Takotsubo syndrome a rare entity in patients with COVID-19: An updated review of case-reports and case-series. Int. J. Cardiol. Heart Wasc. 2020;29:100604. DOI: 10.1016/j. ijcha.2020.100604.
- Faqihi F., Alharthy A., Alshaya R., Papanikolaou J., Kutsogiannis D.J., Brindley P.G. et al. Reverse takotsubo cardiomyopathy in fulminant COVID-19 associated with cytokine release syndrome and resolution following therapeutic plasma exchange: a case-report. BMC Cardiovasc. Disord. 2020;20(1):389. DOI: 10.1186/s12872-020-01665-0.
- Dabbagh M.F., Aurora L., D'Souza P., Weinmann A.J., Bhargava P., Ba-sir M.B. et al. Cardiac tamponade secondary to COVID-19. JACC Case Rep. 2020;2(9):1326-1330. DOI: 10.1016/j.jaccas.2020.04.009.
- Sala S., Peretto G., Gramegna M., Palmisano A., Villatore A., Vignale D. et al. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur. Heart J. 2020;41(19):1861-1862. DOI: 10.1093/eurheartj/ehaa286.
- Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L. et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. Cardiol. 2020;109(5):531-538. DOI: 10.1007/s00392-020-01626-9.
- Capotosto L., Nguyen B.L., Ciardi M.R., Mastroianni C., Vitarel-li A. Heart, COVID-19, and echocardiography. Echocardiography. 2020;37(9):1454-1464. DOI: 10.1111/echo.14834.
- Babapoor-Farrokhran S., Gill D., Walker J., Rasekhi R.T., Bozorgnia B., Amanullah A. Myocardial injury and COVID-19: Possible mechanisms. Life Sci. 2020;253:117723. DOI: 10.1016/j.lfs.2020.117723.
- Lippi G., Lavie C.J., Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog. Cardiovasc. Dis. 2020;63(3):390-391. DOI: 10.1016/j. pcad.2020.03.001.
- Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020;8(4):e21. DOI: 10.1016/S2213-2600(20)30116-8.
- Kuster G.M., Pfister O., Burkard T., Zhou Q., Twerenbold R., Haaf P. et al. SARS-CoV2: Should inhibitors of the renin-angiotensin system be withdrawn in patients with COVID-19? Eur. Heart J. 2020;41(19):1801-1803. DOI: 10.1093/eurheartj/ehaa235.
- Ferrario C.M., Jessup J., Chappell M.C., Averill D.B., Brosnihan K.B., Tallant E.A. et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111(20):2605-2610. DOI: 10.1161/CIRCULA-TIONAHA.104.510461.
- Sun M.L., Yang J.M., Sun Y.P., Su G.H. Inhibitors of RAS might be a good choice for the therapy of COVID-19 pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(3):219-222. DOI: 10.3760/cma.j.is sn.1001-0939.2020.03.016.
- Danser A.H.J., Epstein M., Batlle D. Renin-angiotensin system blockers and the COVID-19 pandemic: At present there is no evidence to abandon renin-angiotensin system blockers. Hypertension. 2020;75(6):1382-1385. DOI: 10.1161/HYPERTENSIONAHA.120.15082.
- Vaduganathan M., Vardeny O., Michel T., McMurray J.J.V., Pfeffer M.A., Solomon S.D. Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19. N. Engl. J. Med. 2020;382(17):1653-1659. DOI: 10.1056/NEJMsr2005760.
- Inciardi R.M., Lupi L., Zaccone G., Italia L., Raffo M., Tomasoni D. et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):819-824. DOI: 10.1001/jamacar-dio.2020.1096.
- Deshotels M.R., Xia H., Sriramula S., Lazartigues E., Filipeanu C.M. Angiotensin II mediates an-giotensin converting enzyme type 2 internal-ization and degradation through an angiotensin II type I receptor-dependent mechanism. Hypertension. 2014;64(6):1368-1375. DOI: 10.1161/ HYPERTENSIONAHA.114.03743.
- Shah P.B., Welt F.G.P., Mahmud E. Triage considerations for patients referred for structural heart disease intervention during the coronavi-rus disease 2019 (COVID-19) pandemic: An ACC /SCAI Consensus Statement. JACC Cardiovasc. Interv. 2020;13(12):1484-1488. DOI: 10.1016/j.jcin.2020.04.001.
- Tan W., Aboulhosn J. The cardiovascular burden of coronavirus disease 2019 (COVID-19) with a focus on congenital heart disease. Int. J. Cardiol. 2020;309:70-77. DOI: 10.1016/j.ijcard.2020.03.063.
- Liu K., Fang Y.Y., Deng Y., Liu W., Wang M.F., Ma J.P. et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei province. Chin. Med. J. (Engl.). 2020;133(9):1025-1031. DOI: 10.1097/ CM9.0000000000000744.
- Chen C., Chen C., Yan J.T., Zhou N., Zhao J.P., Wang D.W. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48(7):567-571. DOI: 10.3760/ cma.j.cn112148-20200225-00123.
- Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020;8(5):475-481. DOI: 10.1016/S2213-2600(20)30079-5.
- Alon D., Stein G.Y., Korenfeld R., Fuchs S. Predictors and outcomes of infection-related hospital admissions of heart failure patients. PLoS One. 2013;8(8):e72476. DOI: 10.1371/journal.pone.0072476.
- Arentz M., Yim E., Klaff L., Lokhandwala S., Riedo F.X., Chong M. et al. Characteristics and outcomes of 21 critically Ill patients with COVID-19 in Washington State. JAMA. 2020;323(16):1612-1614. DOI: 10.1001/ jama.2020.4326.
- Szekely Y., Lichter Y., Taieb P., Banai A., Hochstadt A., Merdler I. et al. Spectrum of Cardiac Manifestations in COVID-19: A Systematic Echocardiography Study. Circulation. 2020;142(4):342-353. DOI: 10.1161/ CIRCULATIONAHA.120.047971.
- Mehra M.R., Ruschitzka F. COVID-19 Illness and heart failure: A missing link? JACC Heart Fail. 2020;48(6):512-514. DOI: 10.1016/j. jchf.2020.03.004.
- Gao L., Jiang D., Wen X.S., Cheng X.C., Sun M., He B. et al. Prognostic value of NT-proBNP in patients with severe COVID-19. Respir. Res. 2020;21(1):83. DOI: 10.1186/s12931-020-01352-w.
- D'Andrea A., Scarafile R., Riegler L., Liccardo B., Crescibene F., Coc-chia R. et al. Right ventricular function and pulmonary pressures as independent predictors of survival in patients with COVID-19 pneumonia. JACC Cardiovasc. Imaging. 2020;13(1):2467-2468. DOI: 10.1016/j. jcmg.2020.06.004.
- Barman H.A., Atici A., Tekin E.A., Baycan O.F., Alici G., Meric B.K. et al. Echocardiographic features of patients with COVID-19 infection: A cross-sectional study. Int. J. Cardiovasc. Imaging. 2020;8:1-10. DOI: 10.1007/s10554-020-02051-9.
- Baycan O.F., Barman H.A., Atici A., Tatlisu A., Bolen F., Ergen P. et al. Evaluation of biventricular function in patients with COVID-19 using speckle tracking echocardiography. Int. J. Cardiovasc. Imaging. 2020;15:1-10. DOI: 10.1007/s10554-020-01968-5.
- Stöbe S., Richter S., Seige M., Stehr S., Laufs U., Hagendorff A. Echocardiographic characteristics of patients with SARS-CoV-2 infection. Clin. Res. Cardiol. 2020;109(12):1549-1566. DOI: 10.1007/s00392-020-01727-5.
- Croft L.B., Krishnamoorthy P., Ro R., Anastasius M., Zhao W., Buckley S. et al. Abnormal left ventricular global longitudinal strain by speckle tracking echocardiography in COVID-19 patients. Future Cardiol. 2020;9:10.2217/fca-2020-0121. DOI: 10.2217/fca-2020-0121.
- Mahmoud-Elsayed H.M., Moody W.E., Bradlow W.M., Khan-Kheil A.M., Senior J., Hudsmith L.E. et al. Echocardiographic findings in patients with COVID-19 pneumonia. Can. J. Cardiol. 2020;36(8):1203-1207. DOI: 10.1016/j.cjca.2020.05.030.
- Fayssoil A., Mustafic H., Mansencal N. The right ventricle in COVID-19 patients. Am. J. Cardiol. 2020;130:166-167. DOI: 10.1016/j.amj-card.2020.06.007.
- Li Y., Li H., Zhu S., Xie Y., Wang B., He L. et al. Prognostic value of right ventricular longitudinal strain in patients with COVID-19. JACC Cardiovasc. Imaging. 2020;13(11):2287-2299. DOI: 10.1016/j. jcmg.2020.04.014.
- Xiong T.Y., Redwood S., Prendergast B., Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur. Heart J. 2020;41(19):1798-1800. DOI: 10.1093/eurheartj/ehaa231.
- Johri A.M., Galen B., Kirkpatrick J.N., Lanspa M., Mulvagh S., Thamman R. ASE statement on point-of-care ultrasound during the 2019 novel coronavirus pandemic. J. Am. Soc. Echocardiogr. 2020;33(6):670-673. DOI: 10.1016/j.echo.2020.04.017.
- Cardiovascular point-of-care imaging for the medical student and novice user. American Society of Echocardiography. URL: https://aseuniversity. org/ase/lessons/47 (available from March 25, 2020).


