Potentially fatal cerebral venous sinus thrombosis followed by a hemorrhagic stroke in a vaccinated patient: do not rule out COVID-19 as a reason
Автор: Mishra M.K., Sahu A.
Журнал: Juvenis scientia @jscientia
Рубрика: Клинические случаи
Статья в выпуске: 5 т.9, 2023 года.
Бесплатный доступ
Stroke is amongst the leading causes of morbidity and mortality globally. Majority of strokes are ischemic and up to 1/3rd ischemic strokes have infective etiology. In this post-pandemic era, SARS-CoV-2 is an established infectious agent which can precipitate it by various mechanisms. Though post-vaccination incidence of COVID-19 has dropped drastically, still new cases get reported with typical or atypical presentations. Irrespective of causation, malignant cerebral edema in stroke necessitates salvage neurosurgery. Hereby authors present an interesting diagnostic chase in a young female who presented in altered sensorium, underwent emergency decompressive craniectomy and neurologically recovered over subsequent days. Despite being double vaccinated, she developed potentially fatal COVID-encephalitis, cerebral venous sinus thrombosis (CVST), ischemic infarcts and hemorrhagic transformation. Suprisingly, there were cross reacting antibodies against antigens of herpes simplex virus (HSV), leptospira and cytomegalovirus (CMV) yielding false positivity on serology screening test, which spoofed us while carrying out infectious disease work up of stroke.
Covid-19, sars-cov-2, decompressive craniectomy, cerebral venous sinus thrombosis, cross reacting antibody, stroke, hemorrhagic infarct
Короткий адрес: https://sciup.org/14128750
IDR: 14128750 | DOI: 10.32415/jscientia_2023_9_5_45-52
Текст научной статьи Potentially fatal cerebral venous sinus thrombosis followed by a hemorrhagic stroke in a vaccinated patient: do not rule out COVID-19 as a reason
The pandemic of Coronavirus Disease (COVID-19) has crippled humanity thrice since its inception in December 2019. Surviving amidst fear of its future waves has been new normal. Apart from pneumonia, other sequelae of its spectrum are getting added to literature. The neurological manifestations of COVID-19 span from headache to convulsions, coma and death. Hereby authors present their experience of managing a young patient, who was referred to the neurosurgical unit in unconsciousness state secondary to malignant hemorrhagic venous infarction, earning emergency decompressive craniectomy (DC). Interestingly she had COVID-19 antibodies which cross reacted with antigens of other diseases on serological testing and mislead us while establishing the etiopathology of cerebral venous sinus thrombosis (CVST) and infarct.
CASE REPORT
A 20-year-old unmarried girl was admitted to our center in August 2022. The patient had a history of fever and headache for 10 days, and after onset of convulsions, parents presented her to the hospital. Baseline non-contrast computed tomography (NCCT) head had features of vasculitis and hemorrhage in the left medial temporal lobe with effacement of sulci (Fig. 1).
The patient’s consciousness on Glasgow coma scale (GCS) was E2V2M4. Magnetic resonance imaging (MRI) brain showed left temporal edema with parieto-occipital hemorrhage with significant midline shift to right (Fig. 2a, 2b).
Magnetic resonance spectroscopy (MRS) had N-acetylaspartate (NAA) peak (Fig. 3) suggestive of bleed from benign pathology.
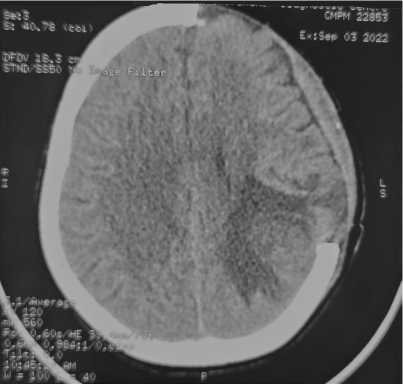
There was non-visualization of left transverse sinus in the venogram phase (Fig. 4).
Laboratory parameters of patient’s blood and cerebro-spinal fluid (CSF) were as of Table 1.
In view of clinical deterioration and imaging suggestive of hemorrhagic infarct with significant mass-effect, the patient was taken up for left decompressive craniectomy (DC). She regained consciousness on post-operative day 3. Hemorrhage and cerebral edema had resolution in subsequent scan (Fig. 5).
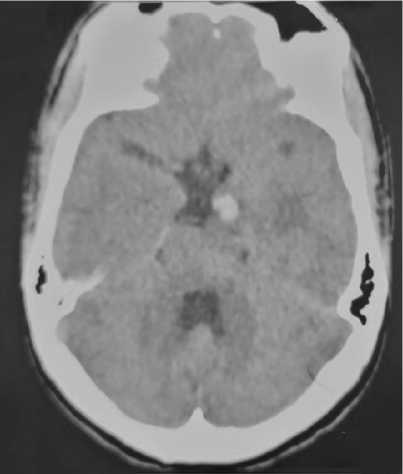
Figure 1: Axial section of NCCT Head showing left temporal hypo-densities (suggestive of infarct) with effaced sulci and medial temporal hyper- density (suggestive of acute hemorrhage).
Presence of cerebral venous sinus thrombosis (CVST) and hemorrhagic infarct in conjunction with triple positive serology (Ig M) against Herpes Simplex Virus (HSV), Leptospira & Cytomegalovirus (CMV) rendered us for retrograde history taking and further investigations. Literature was looked into, but none of the articles showed cross-reaction amongst HSV, CMV & Leptospira antibodies yielding positive Ig M serology. PCR (Polymerase Chain Reaction) for HSV and CMV were negative. Patient had no history of COVID-19 positivity and she had received 2 doses of COVID-19 vaccine: COVISHIELD ® (Recombinant ChAdOx1 nCoV-19 Corona Virus Vaccine, Serum Institute of India) in June 2021 and September 2021. Her nasopharyngeal and oropharyngeal swab specimens were sent for COVID-19 RT-PCR during the afebrile phase of convalescence (23rd day from first symptoms). Both tested negative. Blood and CSF (lumbar puncture) samples were sent afterward for COVID-19 antibody titer (24th day from onset of symptoms). Blood and CSF IgG antibody values (chemiluminescent microparticle immune assay) were
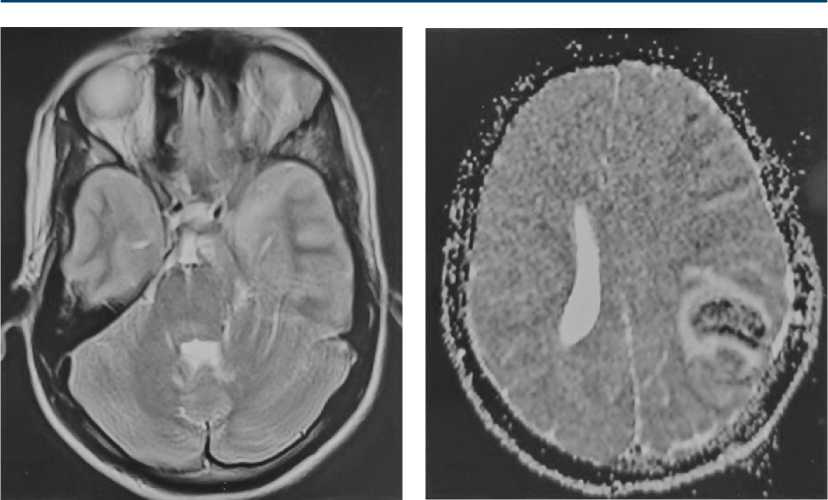
Figure 2a: T2 weighted MRI brain showing left temporal hyper intensity (edema).
>4000 AU/ml (AU: Arbitrary Unit). ≥50.0 AU/ml biological reference value signified a ‘positive’ result (post-exposure to COVID-19 or, post-vaccination in 2–3 weeks’ time frame). In this semi-quantitative test antibody (Ig G) level was measurable up to 4000 AU/ml in our laboratory. Patient was managed as per the standard post-operative neurosurgical case protocol. Convalescence was uneventful. She was discharged in satisfactory condition (Glasgow Outcome Scale: 5, GCS: E4V5M6).
DISCUSSION
With a global incidence of 13.7 million new cases, stroke is the 2nd leading cause of morbidity and mortality. Approximately 87 % of these are ischemic strokesand hemorrhagic transformation is not uncommon. Up to 1/3rd of these ischemic strokes are infective [1]. Hepatitis C virus, Hepatitis B, HIV, HSV, Chicken pox virus, Toxocara, Toxoplasma, Dengue virus are common infective agents causing infective stroke [2].
CVST is a rare variant of stroke with an annual incidence of 2–5 cases/million population. Female gender, inherited coagulopathy, trauma, malignancy,
Figure 2b: T2 weighted gradient echo MRI brain showing left parieto- occipital blooming (suggestive of hemorrhage) with ipsilateral effaced sulci, chinked left lateral ventricle and mid-line shift to right.
hormonal contraceptives, bacterial meningitis and facial infections are known risk factors [3]. By inducing hypercoaguable state, COVID-19 virus has established itself as an infective risk factor for CVST [3, 4].
Till December 2022, human race has successfully defied 3 soaring waves of COVID-19. The intrinsic property of mutation and genetic drift in Corona-varidae has empowered this virus to cast its curse onto us for long in future. Following development of effective vaccines and subsequent decline in cases, stringent lockdown and other restrictions have been lifted in phase wise manner globally.
Apart from typical Influenza like illness (ILI) symptoms, patients may present with isolated neurological complaints, spanning from headache/ seizure to coma [4]. In a recent meta-analysis over 108,571 diagnosed patients, Nannoni et al. (October, 2020) concluded that 1.4 % of individuals with COVID-19 suffered acute cerebrovascular disease (acute ischemic stroke or intracerebral hemorrhage). Ischemic stroke was more common, patients with COVID-19 and stroke were younger than patients
Table 1
Laboratory parameters of the patient
with stroke without infection, female sex was less frequently affected and stroke rate was the highest in Asian population [5].
Aaron S et al. (2022) in their single center study from India on 97 CVST patients during first and second waves of this pandemic, observed that 81 % COVID-associated CVST cases presented with similar semiology, as of our case. Headache (100 %) and seizures (90 %)
without respiratory ILI symptoms, were the presenting complaints. COVID association was established only due to pre-hospitalization virus testing policy, as made mandatory by the Union Government at that time. 90 % of COVID-associated CVST had transverse sinus involvement and hemorrhagic venous infarct. 30 % needed DC. All such patients survived with excellent outcome at 6 months follow up [4].
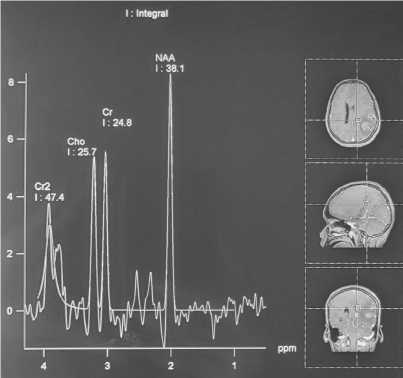
Figure 3: Magnetic resonance spectroscopy (MRS) brain showing NAA peak.
Though the vaccine has been highly effective in curbing the pandemic, still it doesn’t carry 100 % protective efficacy (PE) against all strains of this disease. Pramod S et al. (2022) in their case-control study have reported the PE of COVISHIELD ® between 57 %-74 % in preventing symptomatic/ laboratory-proven COVID-19 and 72 %-100 % in preventing hospitalization and severe infection [9]. In a community based study at UK, Ayoubkhani D et al. (2022) have found that receiving 2 COVID-19 vaccinations was associated with a 41 % decrease in the odds of developing long COVID symptoms. However, double vaccination couldn’t prevent the population from getting infected with Omicron variant [10].

Figure 4: Magnetic resonance venogram (MRV) brain showing non-visualization of left transverse sinus.
Post-vaccination antibody titer tends to decrease significantly within 90 days [11]. Even immunity acquired by booster vaccination tends to fade fast over next 30 days. An elevated titer indicates recent infection [12].
Table 2
|
Confirmed |
SARS-CoV-2 detected in CSF or brain tissue † or evidence of SARS-CoV-2-specific intrathecal antibody; and (2) no other explanatory pathogen or cause found |
|
Probable |
SARS-CoV-2 detected in respiratory or other non-CNS sample, or evidence of SARS-CoV-2-specific antibody in serum indicating acute infection; and (2) no other explanatory pathogen or cause found |
|
Possible |
Patient meets suspected case definition of COVID-19 according to national or WHO guidance on the basis of clinical symptoms and epidemiological risk factors; in the context of known community SARS-CoV-2 transmission, supportive features include the following: the new onset of at least one of cough, fever, muscle aches, loss of smell, or loss of taste; lymphopenia or raised D-dimer level; and radiological evidence of abnormalities consistent with infection or inflammation (e.g., ground glass changes) |
WHO = World Health Organization, SARS-CoV-2 = Severe acute respiratory syndrome coronavirus- 2.
WHO SARS-CoV-2 meningitis, encephalitis, myelitis, or CNS vasculitis case definition
Our case was diagnosed as confirmed case of “SARS-CoV-2 with neurological disease”, as per “WHO COVID-19 case definitions” (Table 2) on the basis of clinical features and COVID-19 antibody positivity in CSF/blood [13].
CONCLUSION
CVST/stroke patients for COVID-19, even if they are vaccinated or lack prodromal symptoms.
Funding: The authors declare no funding.
Conflict of interest: The authors declare no conflict of interest.
Compliance with ethical principles: Study was in compliance with the ethical standards developed in accordance with the World Medical Association Declaration of Helsinki «Ethical Principles for Medical Research Involving Human Subjects», as amended in 2000.
Author contributions: All authors confirm the authorship according to the international criteria of ICMJE (all authors have made substantial contributions to the conception, design, conduct of the study, and preparation of the manuscript, have read and ap-proved the final version for publication).
Список литературы Potentially fatal cerebral venous sinus thrombosis followed by a hemorrhagic stroke in a vaccinated patient: do not rule out COVID-19 as a reason
- Saini V, Guada L, Yavagal DR. Global Epidemiology of Stroke and Access to Acute Ischemic Stroke Interventions. Neurology. 2021;97(20 Suppl 2):S6-S16. DOI: 10.1212/WNL.0000000000012781.
- Saberi A, Akhondzadeh S, Kazemi S, Kazemi S. Infectious Agents and Stroke: A Systematic Review. Basic Clin Neurosci. 2021;12(4):427-440. DOI: 10.32598/bcn.2021.1324.2.
- Dakay K, Cooper J, Bloomfield J, et al. Cerebral Venous Sinus Thrombosis in COVID-19 Infection: A Case Series and Review of The Literature. J Stroke Cerebrovasc Dis. 2021;30(1):105434. DOI: 10.1016/j.jstrokecerebrovasdis.2020.105434.
- Miraclin T A, Aaron DS, Sivadasan A, et al. Management and Outcomes of COVID-19 Associated Cerebral Venous Sinus Thrombosis. J Stroke Cerebrovasc Dis. 2022;31(4):106306. DOI: 10.1016/j.jstrokecerebrovasdis.2022.106306.
- Nannoni S, de Groot R, Bell S, Markus HS. Stroke in COVID-19: A systematic review and meta-analysis. Int J Stroke. 2021;16(2):137-149. DOI: 10.1177/1747493020972922.
- Ehret J, Al Safi A, Akabusi C, et al. A Case Report of Herpes Simplex-1 Viral Encephalitis Complicated by Hemorrhagic Conversion. Cureus. 2022;14(4):e24255. DOI: 10.7759/cureus.24255.
- Vandervore L, Van Mieghem E, Nowé V, et al. False positive Herpes Simplex IgM serology in COVID-19 patients correlates with SARS-CoV-2 IgM/IgG seropositivity. Diagn Microbiol Infect Dis. 2022;103(1):115653. DOI: 10.1016/j.diagmicrobio.2022.115653.
- Luvira V, Leaungwutiwong P, Thippornchai N, et al. False Positivity of Anti-SARS-CoV-2 Antibodies in Patients with Acute Tropical Diseases in Thailand. Trop Med Infect Dis. 2022;7(7):132. DOI: 10.3390/tropicalmed7070132.
- Pramod S, Govindan D, Ramasubramani P, et al. Effectiveness of Covishield vaccine in preventing Covid-19 — A test-negative case-control study. Vaccine. 2022;40(24):3294-3297. DOI: 10.1016/j.vaccine.2022.02.014.
- Ayoubkhani D, Bosworth ML, King S, et al. Risk of Long COVID in People Infected With Severe Acute Respiratory Syndrome Coronavirus 2 After 2 Doses of a Coronavirus Disease 2019 Vaccine: Community-Based, Matched Cohort Study. Open Forum Infect Dis. 2022;9(9):ofac464. DOI: 10.1093/ofid/ofac464.
- Favresse J, Bayart JL, Mullier F, et al. Antibody titres decline 3-month post-vaccination with BNT162b2. Emerg Microbes Infect. 2021;10(1):1495-1498. DOI: 10.1080/22221751.2021.1953403.
- Kusunoki H, Ekawa K, Ekawa M, et al. Trends in Antibody Titers after SARS-CoV-2 Vaccination-Insights from Self-Paid Tests at a General Internal Medicine Clinic. Medicines (Basel). 2023;10(4):27. DOI: 10.3390/medicines10040027.
- Ellul MA, Benjamin L, Singh B, et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19(9):767-783. DOI: 10.1016/S1474-4422(20)30221-0.


