Prospective comparative study of medial parapatellar and medial subvastus approaches in total knee arthroplasty
Автор: Badawi I.A., Ismail A.S., Waly A.H., Khalkaf M.A.N.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 4 т.30, 2024 года.
Бесплатный доступ
Introduction Total knee arthroplasty (TKA) is the treatment of end-stage osteoarthritis in patients who failed to respond to conservative treatment in providing significant pain relief and improving joint function. The medial parapatellar approach (MPP) allows adequate patellar eversion and sufficient knee flexion to expose the knee joint, but the incision through the quadriceps tendon may impair the extensor mechanism of the knee post-operatively. The subvastus approach (SV) completely spares both the quadriceps tendon and muscle and provides adequate exposure of the knee joint for the replacement procedure, SV maintains integrity of the patellar blood supply and reduces post-operative pain resulting in shorter hospital stay.The aim of this prospective study was to compare the results of the medial parapatellar and subvastus approaches in primary total knee arthroplasty (TKA) regarding postoperative pain, recovery of muscle strength, range of knee motion and return to regular daily activities.Materials and Methods Sixty patients underwent TKA at El-Hadara university hospital in Alexandria. The medial parapatellar apphroach (MPP) was performed in 30 patients while the subvastus approach (SV) was used for the other 30 patients. The choice of approach was randomly assigned.Results The statistical analysis of the results at the end of a 6-month follow-up showed that there were no significant differences between the patients in group 1 (MPP) and group 2 (SV) with respect to age, gender, comorbidity, side operated or body mass index (BMI). Regarding the functional knee scores (IKDC, WOMAC), there were no differences at 4 weeks, 3 months and 6 months postoperatively between the two groups. However, we found better outcomes in the SV group regarding the VAS score during the first five postoperative days, earlier quadriceps recovery by assessment of Straight Leg Raising test (SLR), while the operative time was longer in the SV group with less blood collected postoperatively in hemovac drain in the same group.Discussion In our study during the operation via the MPP approach, the index suture positioned at the superomedial border of the patella and the opposite suture on the medial retinacular flap had enabled the surgeon to avoid patellar maltracking during closure of the wound. In the SV group, the L-shaped incision of the medial capsule was considered an efficient landmark for accurate soft tissue closure avoiding the patellar maltracking.Conclusion The subvastus approach offers the advantage of keeping the integrity of quadriceps muscle and the extensor mechanism remains intact post-surgery. It causes less pain and less blood loss postoperatively than the regular parapatellar approach. The patient could recover the knee function in a shorter time with fewer complications, which is greatly in line with the concept of ERAS (Enhanced Recovery After Surgery).
Arthroplasty, knee joint, medial parapatellar approach, subvastus approach
Короткий адрес: https://sciup.org/142242617
IDR: 142242617 | УДК: 616.728.3-77-089.844-089.168 | DOI: 10.18019/1028-4427-2024-30-4-511-521
Текст научной статьи Prospective comparative study of medial parapatellar and medial subvastus approaches in total knee arthroplasty
Total knee arthroplasty (TKA) is the treatment of end-stage osteoarthritis in patients who failed to respond to conservative treatment in providing significant pain relief and improving joint function [1]. The medial parapatellar approach (MPP) is the most common approach performed by orthopaedic surgeons [2]. This approach allows adequate patellar eversion and sufficient knee flexion to expose the knee joint [3], but unfortunately the incision through the quadriceps tendon may impair the extensor mechanism of the knee post-operatively [4]. The subvastus approach (SV) completely spares both the quadriceps tendon and muscle and provides adequate exposure of the knee joint for the replacement procedure [5]. This procedure theoretically maintains integrity of the patellar blood supply and reduces post-operative pain resulting in shorter hospital stay [6].
Other approaches have been documented in the literature, with the majority, if not all, aiming to maintain the quadriceps mechanism in order to have fast postoperative recovery and quadriceps function. The midvastus technique, which differs from the subvastus technique in that the vastus medialis muscle is split in line with its fibres rather than being subluxated laterally in its whole, is another strategy to access the joint. The quadriceps tendon and the superior genicular artery to the patella are preserved with this technique [7].
While the lateral parapatellar approach is performed mainly in valgus knees, other techniques as tibial tubercle osteotomy (TTO), rectus snip and quadriceps turndown are preserved for stiff knee and revision total knee arthroplasty [2].
The goal of this prospective study is to compare the results of the medial parapatellar and subvastus approaches in primary total knee arthroplasty regarding postoperative pain, recovery of muscle strength, range of knee motion and return to regular daily activities.
MATERIALS AND METHODS
Sixty patients scheduled for primary total knee arthroplasty were included in this study.
All patients underwent TKA at El-Hadara university hospital in Alexandria during the period from October 2021 till May 2022.
The study was conducted after approval from the ethical committee and patients’ consent.
Characteristics of the study patients :
-
• The MPP approach was performed in 30 patients (group 1) while the SV approach was performed in the other 30 patients (group 2).
-
• The choice of approach was randomly assigned.
-
• The diagnosis leading to total knee replacement was primary degenerative osteoarthritis in all patients.
-
• All patients had the same preoperative preparation as well as the postoperative protocol of treatment.
-
• We have unified the preoperative quadriceps muscle power fin all patients included in this study to be grade 3.
-
• The implant used in all patients was PCS (posterior cruciate scarifying) Total Knee Arthroplasty. All patients were operated under inflated tourniquet.
-
• Time of operative interference was monitored starting from skin incision till skin stapler application.
-
• In all patients, hemovac drain was used to monitor blood loss postoperatively.
-
• Patients suffering from pre-existing muscular or neurologic disease, previous operations on the knee or history of previous injury involving any portion of the quadriceps mechanism were excluded from our study.
Preoperative evaluation
Each patient had his/her affected knee assessed regarding pain, swelling , giving way, stiffness, difficulty with and catching / pseudolocking.
Our clinical examination included BMI calculation (Body Mass Index), gait, medial joint line tenderness and range of motion.
Radiological evaluation included standing AP and lateral plain radiographs as well as stitch long lower limb films of the affected side.
Visual analogue scale (VAS), International Knee Documentation Committee Subjective Knee Score (IKDCS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) were the scores recorded preoperatively.
Operative procedure
Surgery was performed either under general or spinal anaesthesia.

Fig. 1. Index suture marking the superomedial patella and the superomedial capsule
Prophylactic antibiotics were given one hour pre-operatively.
-
— In group 1, patients were operated via MPP approach. A standard anterior midline skin incision proximally around 5–7 cm proximal to upper patella pole and distally to the tibial tubercle. Subcutaneous tissue was dissected to develop a full thickness flap. The capsule was incised through a medial parapatellar approach approximately 1 cm from the medial border of the patella. Incision of the quadriceps mechanism longitudinally allowed adequate patellar eversion and sufficient knee flexion. An index suture was taken on the superomedial border of the patella and another corresponding suture on the superomedial portion of the tendon considering a landmark for later closure after prosthesis implantation to avoid patellar maltracking. The patella was everted laterally, the knee flexed to expose the knee joint.
-
— In group 2, patients were operated via the SV approach. A straight anterior midline skin incision extended proximally around 5-7 cm proximal to upper patella pole and distally to the tibial tubercle.
Subcutaneous tissue was dissected to develop a full thickness flap. Both the quadriceps tendon and muscle was spared. An L-shaped capsulotomy was performed; first, the vertical line of the incision was made along the medial edge of the patellar tendon from the tibial tubercle until crossing the inferior margin of the vastus medialis obliquus, and second, the horizontal line of the incision was made along the inferior margin of the vastus medialis obliquus. After insertion of the implant, the capsule was closed and the muscle remained completely intact.

Fig. 2. L-shaped incision capsulotomy
Post-operative period
-
— Postoperatively, Teicoplanin 400 mg (Targocid) intravenous injection was given once daily and Amikacin 500 mg intravenous injection every 12 hours for 3 days.
-
— Upon home discharge, oral Levofloxacin 500 mg once daily (Tavanic) for 5 days and Oxazolidinone 600 mg (lenozolid) twice daily for 7 days were prescribed for every patient.
-
— Ketorolac Tromethamine (Ketolac) infusion was given every 12 hours and Paracetamol intravenous infusion (Perfalgan) was given every 8 hours as analgesic for 3 days.
-
— At home, Paracetamol 100 mg orally was prescribed for all patients.
-
— Deep vein thrombosis (DVT) prophylaxis started by Enoxaparin Sodium (Clexane) 40 mg subcutaneous injection prescribed for both groups for 14 days then oral Rivaroxaban once daily for 4 weeks.
-
— Postoperatively, knee range of motion was started on the first postoperative day as well as weight bearing as tolerated with aids.
-
— Clinical integrity of the extensor mechanism by the ability of each patient to perform Straight leg raising test (SLR)as soon as possible after the operation.
Method of assessment of results
-
• Visual analogue scale (for the first 5 days daily postoperatively).
-
• The International Knee Documentation Committee Subjective Knee score (IKDCS) and The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) at 4 weeks, 3 months and 6 months post operatively.
Statistical analysis of the data
The data were uploaded in the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using number and percent. The Shapiro – Wilk test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation, median and interquartile range (IQR). Significance of the obtained results was judged at the 5 % level. The used tests were: 1) Chi-square test; 2) Fisher’s Exact test or Monte – Carlo correction; 3) Student t-test; 4) Mann – Whitney test.
RESULTS
All 60 patients included in the study had completed the follow-up period till the end of 6 month.
Demographic data of study patients
Gender There were no statistical differences between the groups regarding gender.
Table 1
Comparison between the two studied groups according to sex
Age The age difference was statistically insignificant.
Table 2
Comparison between the two studied groups according to age
|
Age (years) |
Group 1 ( n = 30) |
Group 2 ( n = 30) |
Student t-test |
p |
|
Min – Max |
55.0 – 73.0 |
55.0 – 67.0 |
0.936 |
0.354 |
|
Mean ± SD |
63.30 ± 4.96 |
62.30 ± 3.10 |
||
|
Median (IQR) |
62.0 (60.0 – 67.0) |
62.0 (60.0 – 65.0) |
SD — Standard deviation; IQR — Interquartile range; p — p value for comparing between the two studied groups.
Side Operated The difference between both groups regarding the affected side was not statistically significant.
Table 3
Comparison between the two studied groups according to affected side
Co-morbidity In group 1, 31 patients had mainly hypertension (53.3 %) and diabetes m ellitus (30 %).In group 2, 26 patients were suffering from only hypertension (76.7 %) and diabetes mellitus (43.3 %).The difference between two groups in terms of co-morbidity was statistically insignificant.
Table 4
Comparison between the two studied groups according to co- morbidity
Body Mass Index (BMI) Average BMI in group 1 ranged from 29.04 ± 2.91 while in group 2 ranged from 28.66 ± 2.76.
Table 5
Comparison between the two studied groups according to BMI
|
BMI (kg/m2) |
Group 1 ( n = 30) |
Group 2 ( n = 30) |
Test of sig. |
p |
||
|
No. |
% |
No. |
% |
|||
|
Normal |
3 |
10.0 |
5 |
16.7 |
χ 2 = 0.921 |
MCp = 0.600 |
|
Overweight |
13 |
43.3 |
14 |
46.7 |
||
|
Obese class I |
14 |
46.7 |
11 |
36.7 |
||
|
Min – Max |
23.30 – 34.30 |
24.00 – 33.10 |
t = 0.519 |
0.606 |
||
|
Mean ± SD |
29.04 ± 2.91 |
28.66 ± 2.76 |
||||
|
Median (IQR) |
30.15 (26.70 – 31.0) |
28.6 (26.50 – 30.70) |
||||
2 — Chi square test; MC — Monte – Carlo; t — Student t-test; SD — Standard deviation; IQR — Interquartile range; p — p value for comparing etween the two studied groups.
Operative time Patients in group 2 (SV) had more operative time than those in group 1 (MPP) and this was statistically significant ( p < 0.001).
Table 6
Comparison between the two studied groups according to operative time
|
Time |
Group 1 ( n = 30) |
Group 2 ( n = 30) |
Mann – Whitney test |
p |
|
Min – Max |
1.75 – 2.0 |
1.83 – 2.25 |
196.0* |
< 0.001* |
|
Mean ± SD |
1.93 ± 0.08 |
2.07 ± 0.13 |
||
|
Median (IQR) |
1.92 (1.83 – 2.0) |
2.08 (1.92 – 2.17) |
SD — Standard deviation; IQR — Interquartile range; p — p value for comparing between the two studied groups; * — Statistically significant at p ≤ 0.05.
Hemovac Drain In group 1, the median blood loss calculated in redevac suction was 500 cc while for group 2 it was 350 cc; this difference was statistically significant (p < 0.001).
Table 7
Comparison between the two studied groups according to drain
|
Drain |
Group 1 ( n = 30) |
Group 2 ( n = 30) |
Mann – Whitney test |
p |
|
Min – Max |
450.0 – 600.0 |
300.0 – 450.0 |
12.0* |
< 0.001* |
|
Mean ± SD |
513.3 ± 49.01 |
366.7 ± 40.11 |
||
|
Median (IQR) |
500.0 (450.0 – 550.0) |
350.0 (350.0 – 400.0) |
SD — Standard deviation; IQR — Inter quartile range; p — p value for comparing between the two studied groups; * — Statistically significant at p ≤ 0.05.
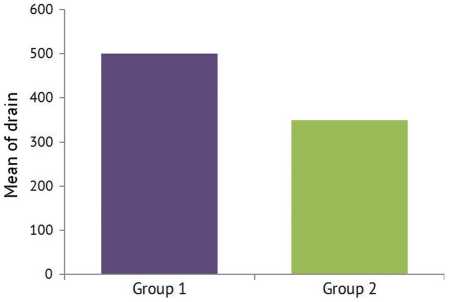
Fig. 3 Comparison between the two studied groups according to drain
Visual Analogue Scale (VAS) On postoperative day 1 and 2, the average in group 1 was 7.80 ± 0.96, while in group 2 it was 4.87 ± 1.01. Starting from postoperative day 3, the difference was more obvious as the average in group 1 was 6.27 ± 1.26 while in group 2 was 2.80 ± 1.35. There were obvious decline in pain sensation and increase in the degree of patient satisfaction, especially in group 2, and this was statistically significant ( p ≤ 0.001) for daily assessment of Visual Analogue Scale.
Table 8
Comparison between the two studied groups according to VAS
|
Day |
VAS |
Group 1 ( n = 30) |
Group 2 ( n = 30) |
Mann – Whitney test |
p |
|
Preoperative |
Min – Max |
8.0 – 10.0 |
8.0 – 10.0 |
405.0 |
0.351 |
|
Mean ± SD |
9.67 ± 0.76 |
9.47 ± 0.90 |
|||
|
Median (IQR) |
10.0 (10.0 – 10.0) |
10.0 (8.0 – 10.0) |
|||
|
1st |
Min – Max |
6.0 – 10.0 |
4.0 – 6.0 |
32.50* |
< 0.001* |
|
Mean ± SD |
7.80 ± 0.96 |
4.87 ± 1.01 |
|||
|
Median (IQR) |
8.0 (8.0 – 8.0) |
4.0 (4.0 – 6.0) |
|||
|
2 nd |
Min – Max |
6.0 – 10.0 |
4.0 – 6.0 |
36.0* |
< 0.001* |
|
Mean ± SD |
7.80 ± 0.96 |
4.87 ± 1.01 |
|||
|
Median (IQR) |
8.0 (6.0 – 8.0) |
4.0 (2.0 – 6.0) |
|||
|
3rd |
Min – Max |
4.0 – 8.0 |
0.0 – 6.0 |
37.0* |
< 0.001* |
|
Mean ± SD |
6.27 ± 1.26 |
2.80 ± 1.35 |
|||
|
Median (IQR) |
6.0 (6.0 – 8.0) |
2.0 (2.0 – 4.0) |
|||
|
4 th |
Min – Max |
2.0 – 6.0 |
0.0 – 4.0 |
48.0* |
< 0.001* |
|
Mean ± SD |
5.40 ± 1.07 |
2.20 ± 1.42 |
|||
|
Median (IQR) |
6.0 (4.0 – 6.0) |
2.0 (2.0 – 4.0) |
|||
|
5 th |
Min – Max |
2.0 – 6.0 |
0.0 – 4.0 |
45.0* |
< 0.001* |
|
Mean ± SD |
4.53 ± 1.38 |
1.27 ± 1.11 |
|||
|
Median (IQR) |
4.0 (4.0 – 6.0) |
2.0 (0.0 – 2.0) |
SD — Standard deviation; IQR — Inter quartile range; p — p value for comparing between the two studied groups; * — Statistically significant at p ≤ 0.05.
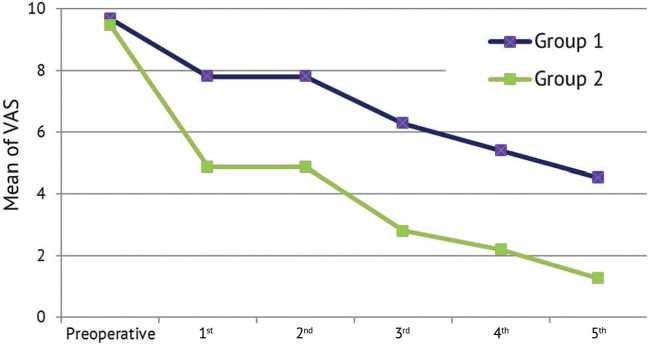
Fig. 4. Comparison between the two studied groups according to VAS
IKDC AND WOMAC scores There were no statistical differences between both groups regarding the IKDC and WOMAC indices.
Table 9
Comparison between the two studied groups according to IKDC
|
VAS |
Group 1 ( n = 30) |
Group 2 ( n = 30) |
Student t-test |
p |
|
|
Preoperative |
Min – Max |
20.0 – 30.0 |
22.0 – 29.0 |
0.805 |
0.424 |
|
Mean ± SD |
25.67 ± 2.44 |
26.13 ± 2.03 |
|||
|
Median (IQR) |
26.0 (24.0 – 28.0) |
26.0 (25.0 – 28.0) |
|||
|
4 weeks |
Min – Max |
30.0 – 43.0 |
30.0 – 43.0 |
0.696 |
0.489 |
|
Mean ± SD |
36.80 ± 3.42 |
37.43 ± 3.63 |
|||
|
Median (IQR) |
36.50 (35.0 – 39.0) |
37.50 (35.0 – 40.0) |
|||
|
3 months |
Min – Max |
38.0 – 57.0 |
40.0 – 56.0 |
1.914 |
0.061 |
|
Mean ± SD |
45.87 ± 4.58 |
48.03 ± 4.18 |
|||
|
Median (IQR) |
46.0 (43.0 – 47.0) |
48.0 (45.0 – 51.0) |
|||
|
6 months |
Min – Max |
35.0 – 64.0 |
39.0 – 66.0 |
1.648 |
0.105 |
|
Mean ± SD |
53.70 ± 5.95 |
56.13 ± 5.48 |
|||
|
Median (IQR) |
54.0 (52.0 – 56.0) |
56.0 (53.0 – 59.0) |
SD — Standard deviation; IQR — Inter quartile range; p — p value for comparing between the two studied groups.
Table 10
|
VAS |
Group 1 ( n = 30) |
Group 2 ( n = 30) |
Mann – Whitney test |
p |
|
|
Preoperative |
Min – Max |
69.0 – 81.0 |
67.0 – 80.0 |
377.0 |
0.277 |
|
Mean ± SD |
74.97 ± 3.18 |
73.90 ± 2.77 |
|||
|
Median (IQR) |
75.0 (73.0 – 77.0) |
74.0 (72.0 – 76.0) |
|||
|
4 weeks |
Min – Max |
40.0 – 75.0 |
42.0 – 70.0 |
385.0 |
0.335 |
|
Mean ± SD |
52.83 ± 7.57 |
51.13 ± 5.76 |
|||
|
Median (IQR) |
53.0 (50.0 – 56.0) |
52.0 (46.0 – 55.0) |
|||
|
3 months |
Min – Max |
27.0 – 70.0 |
23.0 – 66.0 |
361.0 |
0.187 |
|
Mean ± SD |
40.67 ± 9.56 |
37.53 ± 7.68 |
|||
|
Median (IQR) |
40.0 (35.0 – 43.0) |
37.0 (32.0 – 41.0) |
|||
|
6 months |
Min – Max |
20.0 – 68.0 |
22.0 – 60.0 |
336.0 |
0.091 |
|
Mean ± SD |
32.77 ± 10.84 |
28.83 ± 6.52 |
|||
|
Median (IQR) |
30.0 (26.0 – 35.0) |
28.0 (26.0 – 30.0) |
SD — Standard deviation; IQR — Inter quartile range; p — p value for comparing between the two studied groups.
Comparison between the two studied groups according to WOMAC
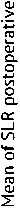
Straight Leg Raising test (SLR) The time lapsed after operation to restore the quadriceps function to perform SLR test was statistically significant between the groups. Patients in group 2 needed shorter time to perform SLR postoperatively than patients in group 1.
Comparison between the two studied groups according to postoperative SLR
Group 2
Fig. 5. Comparison between the two studied groups according to postoperative SLR
Table 11
|
VAS |
Group 1 ( n = 30) |
Group 2 ( n = 30) |
Mann – Whitney test |
p |
|
Min – Max |
7.0 – 45.0 |
7.0 – 21.0 |
184.50* |
< 0.001* |
|
Mean ± SD |
18.83 ± 7.18 |
11.43 ± 5.35 |
||
|
Median (IQR) |
21.0 (14.0 – 21.0) |
7.0 (7.0 – 14.0) |
SD — Standard deviation; IQR — Inter quartile range; p — p value for comparing between the two studied groups; * — Statistically significant at p ≤ 0.05.
Complications One female in group 1 (MPP) had paralytic ileus on the 2nd postoperative day and was treated intensively by parentral nutrition and prokinetics. That complication did not affect our results. Two infected cases in group 1 (MPP) at 7 month and 6 month respectively. One infected case in group 2 (SV) 6 month after the end of the follow-up. Those cases underwent two-stage revision using mobile-bearing antibiotic impregnated cemented spacer in the first stage followed by more constrained knee arthroplasty (CCK) 6 weeks later. Two patients suffered femoral component malrotation, one patient in each group which was not related to the approach selected. Those two cases did not need or did not accept revision at the end of the follow-up.
Comparison between the two studied groups according to complications
Table 12
|
Complications |
Group 1 ( n = 30) |
Group 2 ( n = 30) |
χ 2 test |
FE p |
||
|
No. |
% |
No. |
% |
|||
|
No |
25 |
83.3 |
26 |
86.7 |
0.131 |
1.000 |
|
Yes |
5 |
16.7 |
4 |
13.3 |
||
|
Paralytic Ileus |
1 |
3.3 |
0 |
0.0 |
||
|
Femoral component malrotation |
1 |
3.3 |
1 |
3.3 |
||
|
Infected, 7 months |
1 |
3.3 |
0 |
0.0 |
||
|
Infected, 6 months |
1 |
3.3 |
0 |
0.0 |
||
|
Patient did not apply Physiotherapy settings |
1 |
3.3 |
0 |
0.0 |
||
|
Wound dehiscence |
0 |
0.0 |
2 |
6.7 |
||
|
Infected case |
0 |
0.0 |
1 |
3.3 |
||
FE — Fisher exact test; p — p value for comparing between the two studied groups.
DISCUSSION
Although the subvastus (SV) approach was described in 1929 [5], it is still a debate regarding the efficacy of performing such approach when compared to the popular medial parapatellar (MPP) approach.
In our study, we found better pain tolerance and pain subsidence in the SV group which was evident during the first 5 days post-surgery by recording the Visual Analogue Scale (VAS) scale.
-
P. Dileep et al., in their study of 54 patients during the postoperative period found that pain scores accessed using VAS showed significant lower values in SV group from postoperative day 1 onward [8].
-
M. Hafez concluded in his study that subvastus patients recovered early considering knee pain and motion, which was verified in his series by lower use of painkillers within the first 48 hours and the ability to SLR in a significantly lesser time [9].
According to J.K. Seon et al., the scores on postoperative day 3 were significantly higher on a 10-point visual analogue pain scale for patients who had been randomly assigned to SV approach than in the patients who underwent the standard MPP approach [10].
In our cases, the straight leg raising (SLR) test was performed earlier in the subvastus group as the quadriceps had been left intact; this was evident in the short term period of time at 4 weeks postoperatively. There was no difference in the range of mtotion (ROM).
J.R. Berstock et al’s comparative study showed that the SV approach resulted in earlier recovery of SLR and improved ROM at one week. However, there was no statistical difference between the SV and MPP approaches in KSS (Knee Severity Score) at 6-weeks and 1-year postoperatively [3].
A meta-analysis by P.A. Bouché et al. concluded that no differences were found between various approaches of TKA regarding the functional outcomes, but the SV approach showed higher mean ROM at 6-month post-surgery as compared to all the other surgical approaches of TKA [11].
According to Y. Wu et al's meta-analysis, the SV approach offered higher total KSS and fewer days of SLR ability during primary TKA. The SV approach provided early ROM improvement and a mean decrease in SRL days of 2.35 days compared to patients in the MPP group [12].
M.N.H. Khan and his colleagues concluded that individuals who had surgery using the SV method recovered their quadriceps strength more quickly. This supported their claim that the SV approach is more anatomically sound and speeds up the healing process after surgery [13].
-
G. J. Matehuala et al’s results of the total of 64 patients included in their study showed better evolution in the first four weeks with the subvastus approach, but after six-month follow-up the results were very similar [14].
The SV technique maintains vascular flow to the patella and protects the quadriceps tendon's integrity during surgery, that's why in our series, there was statistical difference regarding blood loss collected in hemovac drain postoperatively.
In our study, we have faced difficulty in surgical exposure in some cases of the SV group. Therefore, there was longer operative time which was statistically significant during collecting our results.
This prolonged time enabled the surgeon to adequately expose the articular surfaces, inserting homan retractors, directly visualizing the placement of our jigs without compromising the inserted implants nor the final result.
According to Y. Wu et al's meta-analysis, patients in the SV group had a mean increase in operation time of 8.88 minutes over those in the MPP technique. On the other hand, compared to the patients receiving the MPP approach, the SV group could dramatically minimize blood loss by a mean of 56.92 mL [12].
Other authors found no appreciable variations in either the length of the procedure nor in the amount of blood loss, as well as no modifications in the end ROM result by operating via the subvastus technique at any time point [15, 16].
Although the subvastus method has numerous advantages, some authors have theorized that because of the small surgical field, it might have a negative impact on the prosthesis positioning and limb alignment [17–20].
-
R. Butala and his collegues in the original study did not recommend the SV approach as they stated that TKA by conventional MPP approach demonstrated better functional outcomes, reduced operative time, reduced tissue trauma (lesser pressure by retractors), shorter learning curve, easier availability of implant and instrument sets and precise implant placement due to a good visualization of the surgical field in comparison to minimal invasive SV approach [21].
In another study by M.G. Bourke et al., it was clear that surgeons viewed the SV technique to be a more technically challenging surgical approach and that the AKSS Functional ratings by 12 months postoperatively favored the MPP group [22].
It is important to consider the M. Sukeik et al's opinion about the limitations of the SV approach. The current meta-analysis found that using an SV technique makes surgery more challenging and demanding since total visibility is decreased, especially in obese patients [23].
In their study, L. Geng et al. found that SV group had an advantage over the conventional MPP group in terms of ROM, VAS, satisfaction rate and the recovery time to SLR within 7 days after operation. However, the above outcomes showed no statistical difference on postoperative day 30 between the two groups. The alignment of the component did not differ significantly between the two groups [24].
In our study, one patient in each group suffered patellar maltracking due to component malrotation which had no relation statistically with the approach used.
The proper component orientation was essentially related to proper visualization of the articular surfaces and proper placement of the retractors.
During the operation via the MPP approach, the index suture positioned at the superomedial border of the patella and the opposite suture on the medial retinacular flap had enabled the surgeon to avoid patellar maltracking during closure of the wound.
In the SV group, the L-shaped incision of the medial capsule was considered an efficient landmark for accurate soft tissue closure avoiding the patellar maltracking.
CONCLUSION
The subvastus approach offers the advantage of keeping the integrity of quadriceps muscle thus the extensor mechanism remains intact post-surgery. It causes less pain and less blood loss postoperatively than the regular parapatellar approach. It can restore the function of the knee joint earlier after the operation with few complications, which is greatly in line with the concept of ERAS (Enhanced Recovery After Surgery). We recommend in cases of BMI obese class I, an expert arthroplasty surgeon perform the subvastus approach in total knee replacement surgery.
Список литературы Prospective comparative study of medial parapatellar and medial subvastus approaches in total knee arthroplasty
- Mahomed NN, Barrett J, Katz JN, et al. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87(6):1222-1228. doi: 10.2106/JBJS.D.02546
- Barrack RL, Smith P, Munn B, et al. The Ranawat Award. Comparison of surgical approaches in total knee arthroplasty. Clin OrthopRelatRes. 1998;(356):16-21. doi: 10.1097/00003086-199811000-00004
- Berstock jR, Murray JR, Whitehouse MR, et al. Medial subvastus versus the medial parapatellar approach for total knee replacement: A systematic review and meta-analysis of randomized controlled trials. EFORTOpen Rev. 2018;3(3):78-84. doi: 10.1302/2058-5241.3.170030
- Fehring TK, Odum S, Griffin WL, Mason JB. Patella inversion method for exposure in revision total knee arthroplasty. J Arthroplasty. 2002;17(1):101-104. doi: 10.1054/arth.2002.29326
- Hofmann AA, Plaster RL, Murdock LE. Subvastus (Southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res. 1991;(269):70-77.
- Lin TC, Wang HK, Chen JW, et al. Minimally invasive knee arthroplasty with the subvastus approach allows rapid rehabilitation: a prospective, biomechanical and observational study. JPhys TherSci. 2013;25(5):557-562. doi: 10.1589/ jpts.25.557
- Engh GA, Holt BT, Parks NL. A midvastus muscle-splitting approach for total knee arthroplasty. J Arthroplasty. 1997;12(3):322-331. doi: 10.1016/s0883-5403(97)90030-9
- Dileep P, Padmanabhan V, Krishnaraj CP. Subvastus approach versus medial parapatellar approach in total knee arthroplasty - A prospective comparative study of functional outcome. Journal of Orthopaedic Association of South Indian States. 2022;19(1):2-6. doi: 10.4103/joasis.joasis_5_22
- Hafez MA. The subvastus approach for primary total knee replacement: Does it affect the early results? Pan Arab J Orth Trauma. 2002;6:181-187.
- Seon JK, Song EK. Navigation-assisted less invasive total knee arthroplasty compared with conventional total knee arthroplasty: a randomized prospective trial. J Arthroplasty. 2006;21(6):777-782. doi: 10.1016/j.arth.2005.08.024
- Bouché PA, Corsia S, Nizard R, Resche-Rigon M. Comparative Efficacy of the Different Surgical Approaches in Total Knee Arthroplasty: A Systematic-Review and Network Meta-Analysis. J Arthroplasty. 2021;36(3):1187-1194.e1. doi: 10.1016/j.arth.2020.09.052
- Wu Y, Zeng Y, Bao X, Xiong H, Hu Q, Li M, Shen B. Comparison of mini-subvastus approach versus medial parapatellar approach in primary total knee arthroplasty. Int J Surg. 2018;57:15-21. doi: 10.1016/j.ijsu.2018.07.007
- Khan MNH, Abbas K, Faraz A, et al. Total knee replacement: A comparison of the subvastus and medial parapatellar approaches. Ann Med Surg (Lond). 2021;68:102670. doi: 10.1016/j.amsu.2021.102670
- Matehuala GJ, Pérez AJM, Villarreal BFJ, Ramos GMQ. Subvastus versus medial parapatellar approach in total knee arthroplasty, functional results. Orthotips. 2021;17(4)7206-210. (In Span.) doi: 10.35366/102218
- Matsueda M, Gustilo RB. Subvastus and medial parapatellar approaches in total knee arthroplasty. Clin Orthop RelatRes. 2000;(371):161-168. doi: 10.1097/00003086-200002000-00020
- Cila E, Güzel V, Ozalay M, et al. Subvastus versus medial parapatellar approach in total knee arthroplasty. Arch Orthop Trauma Surg. 2002;122(2):65-68. doi: 10.1007/s004020100319
- Barrack RL, Barnes CL, Burnett RS, et al. Minimal incision surgery as a risk factor for early failure of total knee arthroplasty. J Arthroplasty. 2009;24(4):489-98. doi: 10.1016/j.arth.2009.02.004
- Lin WP, Lin J, Horng LC, et al. Ouadriceps-sparing, minimal-incision total knee arthroplasty: a comparative study. J Arthroplasty. 2009;24(7):1024-i032. doi: 10.1016/j.arth.2008.07.005
- Thiengwittayaporn S, Fusakul Y, Kangkano N, Jarupongprapa C, Charoenphandhu N. Hand-held navigation may improve accuracy in minimally invasive total knee arthroplasty: a prospective randomized controlled trial. Int Orthop. 2016;40(1):51-57. doi: 10.1007/s00264-015-2848-x
- Jung YB, Lee YS, Lee EY, et al. Comparison of the modified subvastus and medial parapatellar approaches in total knee arthroplasty. Int Orthop. 2009;33(2):419-423. doi: 10.1007/s00264-007-0510-y
- Butala R, Parelkar K, Pandey A. Comparative Analysis of Functional Outcome of Conventional Midline Parapatellar to Minimally Invasive Subvastus Approach in Total Knee Replacement. Orthop J MPC. 2021;27(2):70-74.
- Bourke MG, Buttrum PJ, Fitzpatrick PL, et al. Systematic review of medial parapatellar and subvastus approaches in total knee arthroplasty. J Arthroplasty. 2010;25(5):728-734. doi: 10.1016/j.arth.2009.06.008
- Sukeik M, Sohail MZ, Hossain FS, et al. Comparing the Sub-Vastus and Medial Parapatellar Approaches in Total Knee Arthroplasty: A Meta-Analysis of Short-Term Outcomes. Dr. Sulaiman Al Habib Med J. 2021;3(2):66-73. doi: 10.2991/ dsahmj.k.210203.001
- Geng L, Fu J, Xu C, et al. The Comparison between Mini-Subvastus Approach and Medial Parapatellar Approach in TKA: A Prospective Double-Blinded Randomized Controlled Trial. Orthop Surg. 2022;14(11):2878-2887. doi: 10.1111/ os.13494


