Prospects for cardiovascular system telemonitoring in solving tasks in federal national project “Generation seniors”
Автор: Yakushin Mikhail A., Gorenkov Roman V., Dvorina Olga G., Yarotsky Sergey Y.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 17, 2020 года.
Бесплатный доступ
The paper presents an analysis of some promising lines of developing off-office telemonitoring. Some applications of expert systems designed on the basis of algorithms used for medical decision making are discussed herein. The whys and wherefores of the design of automated hardware & software systems in CVD therapy, which can be used for prevention and off-office follow-up telemonitoring in elderly individuals, are given herein. Methods We evaluated a total of 1078 consecutive anterior STEMI patients who underwent PPCI with deployment of new generations DES. The patients were divided according to the number of implanted stents into 2 groups; multiple-stents group having ≥2 overlapping stents (n =388) and single-stent group (n =690). We compared the rates of major adverse cardiovascular events (MACEs; composite of cardiac death, reinfarction, ischemia-driven target vessel revascularization (TVR), definite stent thrombosis (ST), and stroke) between the 2 study groups. Results There was a non-significant trend toward increased in-hospital mortality in the multiple-stents group [3.4% vs 1.7%; P=0.096] related to a significant higher rate of cardiogenic shock [9.5% vs 6.1%; P=0.037] and post-procedural suboptimal TIMI flow [26.3% vs 19.4%; P=0.009] as compared to the single-stent group. Yet, there were no significant differences between the 2 groups in the incidence of 6-month MACEs: [9% vs 7.1%;The paper presents an analysis of some promising lines of developing off-office telemonitoring. Some applications of expert systems designed on the basis of algorithms used for medical decision making are discussed herein. The whys and wherefores of the design of automated hardware & software systems in CVD therapy, which can be used for prevention and off-office follow-up telemonitoring in elderly individuals, are given herein. Methods We evaluated a total of 1078 consecutive anterior STEMI patients who underwent PPCI with deployment of new generations DES. The patients were divided according to the number of implanted stents into 2 groups; multiple-stents group having ≥2 overlapping stents (n =388) and single-stent group (n =690). We compared the rates of major adverse cardiovascular events (MACEs; composite of cardiac death, reinfarction, ischemia-driven target vessel revascularization (TVR), definite stent thrombosis (ST), and stroke) between the 2 study groups. Results There was a non-significant trend toward increased in-hospital mortality in the multiple-stents group [3.4% vs 1.7%; P=0.096] related to a significant higher rate of cardiogenic shock [9.5% vs 6.1%; P=0.037] and post-procedural suboptimal TIMI flow [26.3% vs 19.4%; P=0.009] as compared to the single-stent group. Yet, there were no significant differences between the 2 groups in the incidence of 6-month MACEs: [9% vs 7.1%;
Telemedicine, telemonitoring, information technologies, off-office monitoring, expert systems, medical decision making, geriatry, medical follow-up
Короткий адрес: https://sciup.org/148311475
IDR: 148311475 | DOI: 10.12710/cardiometry.2020.17.3948
Текст научной статьи Prospects for cardiovascular system telemonitoring in solving tasks in federal national project “Generation seniors”
Mikhail А. Yakushin, Roman V. Gorenkov, Olga G. Dvorina, Sergey Y. Yarotsky. Prospects for cardiovascular system telemonitoring in solving tasks in Federal National Project “Generation Seniors”. Car-diometry; Issue 17; November 2020; p.39-48; DOI: 10.12710/cardi-ometry.2020.17.3948; Available from: issues/no17-november-2020/cardiovascular-system-telemonitoring
In 2019 the implementation of Federal National Project “Generation Seniors” has been started in the Russian Federation that is aimed at an increase of life longevity on the basis of health improvement of the elderly population. The key mechanism in achieving this objective is to extend the coverage of preventive check-ups and examinations of the elderly individuals including follow-up. It has been scheduled that before 2024 the above prevention coverage shall be more than three times greater: namely, it shall be increased from 23% to 70%. It is suggested that 90% of the individuals with diagnosed diseases and pathologies shall be involved in further follow-up care. It is proposed to solve this task by establishing the geriatric health care system and expanding responsibilities of primary care doctors (primary therapists, GPs and preventive care doctors) [1].
To treat seniors is always a complicated case, since most of them show comorbidities that is the cause that they receive multi-component, duplicative or even counteracting medical drugs administered by medical doctors. A primary care doctor, who has no special competencies in treatment of geriatric patients, cannot make the proper medical decision, when assessing two diseases in the same elderly person, due to their complex manifestation pattern, and, as a result, can administer an inadequate or improper medication. As a consequence, a huge number of seniors are treated with negatively geriotropic drugs, which have poten- tially harmful effects on an elderly person organism. In the circumstances, a geriatry care doctor, who is competent in geriotropicity, comorbidities and polypragmasia, shall become a carrier of rapidly developing geriatric technologies to avoid this sort of risks [2].
But at the same time, according to Order No.38 “Approval of Geriatric Care Procedure Regulations” dd. 29th of January, 2016 issued by the Russian National Health Care Ministry, the standard staff in the Geriatry Care System shall be assigned according to calculation as follows: one full-time geriatric doctor per 20000 of elderly individuals that means that it is possible to establish and support the Geriatry Care offices in large cities with a population over 100000 or 1000000 people only. Therefore, it may be concluded that the establishing geriatric care system will not be capable of rendering global geriatric servicing, not to mention follow-up of this sort of patients. Moreover, it is scheduled that a full-time geriatric doctor shall be financed by a responsible medical office within the pre-assigned salary fund that might be realized in case of a personnel reduction within the office only.
Capabilities in primary health care are also limited. Each primary general practitioner is responsible for servicing of 1700 patients, which include, as a rule, ~30% of the elderly patients (~510 individuals). Considering the requirements set forth by Order No.173n “Approval of Follow-up Procedure Regulations Applicable to Adults” dd. 29th of March, 2019 and Order No. 290 “Approval of Standard Time Specifications per Patient Visiting General Practitioner’s Office” dd. 02.06.2015 issued by of the Health Care Ministry of Russia, we arrive to a conclusion that workload per primary doctor to undertake follow-up duties will increase by 20%, so that, taking into account his/her regular duties, it may lead either to obstructive consequences or rather formal performance of the duties by the responsible doctor.
Fortunately, there is a good alternative thereto available: to intensify prevention and follow-up is possible with the use of telemedicine technologies. The possibility of this offered solution is regulated by Cl.7 of Order No.173n “Approval of Follow-up Procedure Regulations Applicable to Adults” dd. 29th of March, 2019 issued by of the Health Care Ministry of Russia, and telemedicine may be officially used according to the procedure of establishing and rendering of health care services with the application of telemedicine technologies approved by Order No. 965n “Approval 40 | Cardiometry | Issue 17. November 2020
of Procedure of Establishing and Rendering of Medical Service with the Use of Telemedicine Technologies” dd. 30th of November, 2017.
Telemonitoring (off-office monitoring) is an intensively developing area of the patient-centered telemedicine sector (i.e. based on a remote interaction between a medical doctor and a patient) that is governed by the Russian Federal Law No.242-FZ “Introduction of Changes in some Legal Acts of the Russian Federation Related to Issues of Applications of Information Technologies to the Health Care Area” dd.29th of July 2017.
There is the evidence that telemonitoring of any parameter of the biological data increases the patient’s adherence to treatment, so that the patient pays more attention to his/her own health, makes efforts to follow the administered medical prescriptions and recommendations. An exemplary case to illustrate this is as follows: even a simple pedometer-based telemonitoring results in a rise in the physical activity by 200025000 steps a day [3].
Widely used is the patient-centered telemonitoring technology based on video-channel technique (teledermatology, teletraumatology, telerheumatology, teleorthodontics), telemonitoring of glucometer parameters (telediabetology), telemonitoring of statical, stabilometrical, locomotor-related and dynamical indicators (teleneurology), body mass index values (teledietology), and thermographic data in case of infectious, oncological and rheumatological diseases.
The greatest advance in telemedicine has been made by cardiology, based on remote recording of the real-time heart performance data. For this purpose, designed have been simple, reliable, sensors of the electrocardiography (ECG), which can be properly placed even by intuitive users at home [4].
Most advanced ECG recording devices and analyzers can be easily integrated in smartphones; mobile apps make it possible to process and interpret the re- corded ECG parameters in automated modes, without physician assistance; the obtained processed interpreted data can be sent on-line to the responsible medical staff [5].
There are original engineering concepts of the Holter monitoring available that allows examining a patient without his/her active participation: the Holter monitoring sensors are inserted immediately in garment or fixed to the skin areas with special adhesive tape; recording is carried out with a pre-set periodicity, covering sleeping time, too [6].
Another option in patient-centered telemonitoring is the complex telemonitoring that implies recording of complete sets of different biological data in parallel with their further integral processing. The complex monitoring that has employed the widest application includes the following: ECG + pulse metering + arterial pressure metering + determination of oxygen saturation level of hemoglobin (O2 sats). In addition to the heart performance data, this option offers recording abnormalities or deviations from the normal performance of the respiratory and vascular systems that is of great importance for seniors showing comorbidities.
Connected Local Telemedicine Booth H4D developed in France makes it possible not only to provide remote general check-up, measure antropomet-ric data, but also to make ECG diagnostics, conduct blood sample test, otoscope examination and retinog-raphy [7].
A higher information potential of the complex telemonitoring can be offered by another advanced technology: the ECG recording of the ascending aorta conducted in parallel with Rheogram recording (using PC-assisted hemodynamic analyzer Cardiocode). In addition to the conventional ECG analysis, the Cardiocode technology is capable of noninvasively delivering complete sets of data on hemodynamics of the heart, as listed below: stroke volume, minute volume, volume of blood entering the ventricle in the early diastole (detection of diastolic dysfunction of the left ventricle, if any), volume of blood entering the ventricle in the atrial systole (assessment of contractility of the atrium and identification of the hemodynamic loading on the atrium), total diastolic volume of blood, volume of blood ejected by the ventricle in the rapid ejection phase, volume of blood ejected by the ventricle in the slow ejection phase (assessment of the contractility of the ventricle and identification of the hemodynamic loading on the ventricle), volume of blood delivered by the ascending aorta (assessment of the aorta tonus). A remarkable merit of this technology is its capability to calculate the ejection fraction value (EF) which is the key indicator of the cardiovascular system performance in general and which is decisive for an identification of strategy and tactics of CVD treatment. Conventionally, EF is determined with the use of echocardiography that requires the medical office conditions only.
The complex telemonitoring is the only possible option of rendering health care services in remote areas and regions, where no public medical offices are available (some isolated remote areas, winter quarters in remote regions, remote mines, exploration missions etc.), as well in those cases when patients are immobilized or when patients may not be suitable for transport. It should be mentioned that 6% of the telemedicine projects in health care in the USA are addressed to patients in penitentiaries. Telemedicine is in high demand in case of epidemics (including the COVID-19 epidemic), natural calamities, natural disasters or technological accidents [8, 9].
It might be expected that replacing an in-office consultation by a remote one will discharge the medical office from overloading and relocate the spare resources for a follow-up extension. But actually the saved time is consumed due to an additional time required for telemonitoring establishing and maintenance: training of the patient in use and operation of sensors, formalities in equipment handing-over, delivery and return of telemedicine equipment, data processing, preparation and submission of findings and a final report. A remote consultation hinders (as a consequence, makes longer) collection of history data of the patient and his/her physical examination that produces a negative effect on diagnosis-making and decision-making on adequate treatment [9].
Telecommunication in telemedicine differs from an in-office communication; even a short-time contact requires an attention concentration and switching-over from one activity to another that takes at least 15 minutes [10]. An interruption in a routine activity results in a doubled increase of a risk to make an improper decision [11]. Only 4 telephone conversation a day deprives of more than one working hour. As practice shows, a combination of the telemedicine consultation and the routine in-office duties in primary care lead to a decline in effectiveness of the occupational performance of the medical staff employed [12].
The patient-centered telemonitoring is limited by the possibility to use simple-operated sensors that constrains the range of biological data to be monitored in such a way. In contrast to the clinical telemonitoring, when a doctor-to-doctor communication is maintained and any medical equipment may be used to deliver the required data, the off-office telemonitoring excludes an application of x-ray or sophisticated ultrasound equipment (despite the fact that the respective portable devices are already available), since the applications of the medical instrumentation of this class is associated with the need to involve trained high-competence medical staff only.
Among other essential obstacles to widely use telemonitoring we should note high costs for the special equipment and the absence of well-defined regulations on fees to be paid for telemedicine services. The costs for advanced sensors may vary from several thousands to tens of thousands Roubles so that it cannot be expected that they are purchased by users on their own account. Although we observe a stable tendency to reduce telemedicine costs due to integration of recording devices and retranslating units in personal gadgets as well as due to greater availability of Internet everywhere, we may suggest the final solution of this problem will take at least more than one year. A lot of time will be required for large-scale testing of cost-effectiveness of medical instrumentation and services as well as for legal regulation, routing design & implementation and financing of this type of activity. Issues on education and training of medical staff in telemedicine competencies remain unsolved; there are no educational standards applicable thereto. Doctor-biotechnologists and doctor-cybernetics experts are graduated from some medical universities, which are not entitled to conduct treatment, while a few number of researchers and research institutions, really experienced in the telemedicine theory and practice, cannot use their high potential for these purposes [13,14].
The communication unit of TMCC is a front office, furnished with the server to collect the relevant data from a patient, store them in the database (eHistory Record of the patient), analyze and submit to an expert according to the prescribed routing [16].
The full-time medical staff of TMCC shall include mainly nurseries, who have completed their special training. The task of the staff is to match the client (the patient or the doctor) and the expert performer (the implementer) of the requested medical service. The expert performer duties can be undertaken by any specialist (not always by a medical doctor), who is employed by TMCC, who is well aware of the relevant information and who has the required applicable qual- ification. The expert may cooperate as a remote worker and live even on another continent: that may be of advantage in servicing people during the night time.
At present, the North-American Center Cisco provides the proper routing of medical calls with a staff employing 590 000 doctors and medical specialists and more than 4900 hospitals; it integrates audio- and video-technologies in medical equipment that successfully expands health care in rural areas and remote regions with poor infrastructure. Each working place in this TMCC is capable of servicing up to 500 patients in parallel, and the total number of the serviced clients (patients, personal gadgets) reach hundreds of thousands. It has been evidenced that the operation of TMCC makes possible to reduce the consultation costs by more than 10 times as compared with the standard examinations or check-ups, and in case of monitoring of the cardiovascular system by 5,5 times, respectively [17].
According to the data presented by the Health Care System’s King’s Fund in Great Britain, savings in therapy of major groups of diseases after introduction of the telemedicine technologies vary from 20,4 to 54,6% a year [18].
The off-office telemedicine monitoring is capable of decreasing demand for in-hospital treatment and reducing treatment times. So, as to the patients with heart insufficiency, according to the data of a number of controlled investigations, a reduction in their hospitalization rate by 27-40% is recorded. For the North-American Veteran’s Hospitals reported is a decrease in the hospitalization rate by 20% and in the inpatient bed days by 25%, respectively [19,20].
Analysts believe that the annual demand for telemedicine health care in Russia is 5-8% of the total population that is equivalent to 7,5 – 11 million consultations per year [21, 22].
The most appropriate format of this sort of scenarios may be those expert systems (ES), which are implemented as an electronic algorithm for supporting medical decision making (SMDM) constructed on the basis of expertise and actual expert’s decisions applicable to a given problem (international and national clinical guidelines, medical standards and regulations governing health care service procedures). The ES repertoire, analyzing the relevant diagnostics data obtained with medical instrumentation and primary examination, integrated with telemetric data, delivered in the course of teleconsultation, is capable of substantially expanding and standardizing the telemedicine service as well as avoiding eventual influences produced by subjective factors [23].
Practice shows that, in the medium and long term period, the need for developing the SMDM systems and services will inevitably increase. The current volume of the domestic market for medical information systems, which amounts to 11.5 billion Roubles a year, has a strong tendency of growth rate approximately of 9% a year. The market covers all medical segments: b2b (medical offices, insurance companies, medical equipment manufacturers); b2c (patients and doctors); b2g (authorities responsible for health care development). [24]
Against the background of ageing of population and growing of social dependence, the costs for medical (including telemedical) services for patients of elderly groups demonstrate their annual increase; in Japan up to 47% of the health care budget is spent for these purposes. This is a stimulus for the development of ES for diagnostics and treatment of geriatric diseases. Of particular interest is the design and development of automated ES [25, 26].
Table 1
Influence of AHD* on SHD
|
INN* |
HR** |
TPVR 1*** |
TPVR 2**** |
SV***** |
|
Atenolol |
decreases |
increases |
decreases |
decreases |
|
Bisoprolol |
decreases |
increases |
decreases |
decreases |
|
Betaxolol |
decreases |
decreases |
decreases |
decreases |
|
Nebivolol |
decreases |
decreases |
decreases |
decreases |
|
Metoprolol |
decreases |
decreases |
decreases |
decreases |
|
Amlodipine |
no change |
decreases |
decreases |
no change |
|
Diltiazem |
decreases |
decreases |
decreases |
no change |
|
Nifedipine |
increases |
decreases |
decreases |
increases |
|
Nitrendipine |
increases |
decreases |
decreases |
no change |
|
Moxonidine |
no change |
decreases |
decreases |
no change |
|
Kaptopril |
no change |
decreases |
decreases |
no change |
|
Chinapril |
no change |
decreases |
decreases |
no change |
|
Lizinopril |
no change |
decreases |
decreases |
no change |
|
Perindopril |
no change |
decreases |
decreases |
increases |
|
Ramipril |
no change |
decreases |
decreases |
no change |
|
Fosinopril |
no change |
decreases |
decreases |
no change |
|
Enalapril |
no change |
decreases |
decreases |
increases |
|
Candesartan |
no change |
decreases |
decreases |
no change |
|
Eprosartan |
no change |
decreases |
decreases |
no change |
|
Irbesartan |
no change |
decreases |
decreases |
no change |
|
Losartan |
decreases |
decreases |
decreases |
increases |
|
Telmisartan |
no change |
decreases |
decreases |
no change |
|
Valsartan |
no change |
decreases |
decreases |
no change |
|
Indapamide |
no change |
decreases |
decreases |
no change |
*INN - international non-proprietary name of the drug, **HR - heart rate; ***TPVR1 - total peripheral vascular resistance in the first month of starting treatment; ****TPVR2 - total peripheral vascular resistance after a month of beginning the treatment;
*****SV - stroke volume.
The above integration allows us to fully automate the clinical process and minimize the role undertaken by an expert to just reviewing the made decisions. [10]
The operation of ES "Monitoring and correction of SHD indicators" is based on the determination of the optimal relationship between an antihypertensive drug (AGP) and the SHD personal profile of the patient. The AP level is determined by the following three parameters of SHD: HR, SV and TPVR; by influencing on these parameters, we can control the level of AP, both upwards and downwards. The influence of AHD on SHD is well studied; this information is freely available (see Table 1 herein).
After identifying the personal SHD profile performed is an automatic selection of AHD, which have a normalizing effect on the changed (increased or decreased) SHD parameters and do not affect those indicators, which are within the normal range. If a patient has comorbidities, the selected drugs are further filtered according to the priorities and limitations set out in the current clinical guidelines, and also taking into account possible contraindications.
The format of the daily off-office monitoring allows us to accurately select the AHD dosage and, if 44 | Cardiometry | Issue 17. November 2020
necessary, change the periodicity of the prescribed medication and dosage. In case of negative values in the SHD trend indicators, the administered AHD shall be replaced by other most suitable drugs. All these actions are carried out in an automated way and sent to the responsible attending physician for approval in the form of ready-made solutions, supported by a reasoned justification.
As an integrator of the ES and software of the device, we have used a web-based platform “Neurodoctor" developed by the Vladimirsky Moscow Regional Research and Clinical Institute (MONIKI), which, in addition to storing the necessary databases (electronic medical records, clinical guidelines, medical standards and procedures of health care), is a matrix for the design, construction and placement of ES of any complexity [11].
A patient conducts recording of the SHD parameters staying at home. The recorded data are sent to the central server and the web-based platform, added to the patient record in the archive and stored for their further systematic analysis. The web-based platform, being in the automatic mode of the around-the-clock telemonitoring, with a certain periodicity makes request for updated measurement data on the central server.
|
фЬдкПма BPiQbocg ugbolo жеигИочкд >дд^ (СНСФВ) |
|||||
|
XbOHNrlECKVH CEbTTErlHVH HETTDC1V1DHHOC1P |
фЬдкпна BPiQbocg ugbolo HtGuitoodkg <395 |
|Д фЙНК1ТН0Н9иРНР1у KU9CC |
|||
|
UErlEHNEXCH |
^Ьэкпна BPiQbocg ugbolo жеи№охк9 ^o-pQS (СНиФВ) |
III ,±,rlHKlTNOHgUPHPI0 KU9CC |
|||
|
VblEbNVUPHVti LNUEblOHNU rl UOXNUPIX |
V |
фЬэкПна BPiQbocg ugbolo жвигкГонкэ 32-^0$ (СННФВ) |
II фЙНКЛГ4ОН9иРНР1у KU9CC |
||
|
ЗОНУ иоЬчЖбННЦ |
фЬ9К|ГНН виуЬосэ ugbolo жеиЛИолкч |
цэЬДтвннэя фАнкЛин |
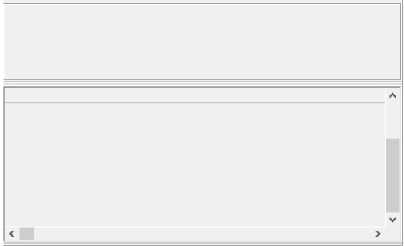
Figure 1. CHF ES, the 1st stage of algorithmic search
| Вверх
eS <8-
Вперед Нозология Справочники
Ф
Назад
В начало
Для перехода к нозологической диагностике нажмите кнопку "Нозология"
□ систолического артериального давления?
Й частота сердечных сокращений?
] Й • бронхиальная астма, атриовентрикулярная блокада 2 и более степени, облитерирующий атеросклероз?
: ; Ь- АРНИ + Ивабрадин + АМКР [базовая схема лечения)
| АРНИ ■•• БАБ 4-АМКР (базовая схема лечения) |
Возможные уровни поражения
АРНИ + БАБ ■•■ АМКР (базовая схема лечения]
■
[ Й • бронхиальная астма, атриовентрикулярная блокада 2 и более степени, облитерирующий атеросклероз?
] ] ь- АРНИ ■•• Ивабрадин + АМКР1 (базовая схема лечения)
] ] i— АРНИ + БАБ ■•• АМКР1 [базовая схема лечения]
] Й • бронхиальная астма, атриовентрикулярная блокада 2 и более степени, облитерирующий атеросклероз?
] р- АРНИ + АМКР (базовая схема лечения)
i р... ДРНИ + БАБ ■•• АМКР (базовая схема лечения)
-
i— Показан перевод в отделение интенсивной терапии
Й- частота сердечных сокращений?
Й ■ бронхиальная астма, атриовентрикулярная блокада 2 и более степени, облитерирующий атеросклероз?
i Ek непереносимости иАПФ (ангионевротический отек, мучительный кашель, появившийся на Фоне приема лекартва]?
i i i— БРА ■•■ Ивабрадин + АМКР [базовая схема лечения)
[ i ь~ иАПФ ■•• Ивабрадин + АМКР [базовая схема лечения)
i Й- непереносимости иАПФ (ангионевротический отек, мучительный кашель, появившийся на Фоне приема лекартва]?
i ;.... БРА + БАБ ■•■ АМКР [базовая схема лечения]
| =— иАПФ -I- БАБ -I- АМКР (базовая схема лечения)
В- бронхиальная астма, атриовентрикулярная блокада 2 и более степени, облитерирующий атеросклероз?
Й" непереносимости иАПФ (ангионевротический отек, мучительный кашель, появившийся на Фоне приема лекартва]?
i к -БРА 4-Ивабрадин 4-ДМКР1 [базовая схема лечения]
i ;.... иАПФ ■•• Ивабрадин + АМКР1 (базовая схема лечения)
В- непереносимости иАПФ (ангионевротический отек, мучительный кашель, появившийся на фоне приема лекартва]? к- БРА + БАБ + АМКР1 (базовая схема лечения)
; - иАПФ + БАБ + АМКР1 [базовая схема лечения)
В бронхиальная астма, атриовентрикулярная блокада 2 и более степени, облитерирующий атеросклероз?
-
В- непереносимости иАПФ (ангионевротический отек, мучительный кашель, появившийся на фоне приема лекартва]?
[ Ь БРА + АМКР [базовая схема лечения]
[ ! - иАПФ + АМКР (базовая схема лечения)
Й- непереносимости иАПФ (ангионевротический отек, мучительный кашель, появившийся на фоне приема лекартва]?
Figure 2. CHF ES, the 2nd stage of algorithmic search (determination of basic plan of treatment)
An automated workplace on the web-based platform controls information updates on the central server in a specified mode and automatically displays the relevant information on the physician’s screen, carrying out filtering, ranking and selection of patients depending on the severity of the identified deviations. Information about patients given in the form of specific diagnostic and treatment recommendations is delivered to the responsible attending physician with the corresponding marking defining the urgency of response.
The effectiveness of HSC "Treatment of hypertension" is confirmed by clinical studies; its potential allows correcting high blood pressure in an unlimited cohort of users. In practice, the capabilities of the web platform are restricted by the intensity of work of the responsible attending physician who shall approve the prepared recommendations. When switching the web-based platform to a fully automated mode (there is an engineering solution already available today), the number of serviced patients may be increased by thousands [10].
The research team from FSSI "National Research Institute of Public Health named after N.A. Semashko", together with the Vladimirsky Moscow Regional Research and Clinical Institute (MONIKI) carries out works on design and development of automated HSS "Treatment of chronic heart failure" based on the combination of the same name ES and the cardiomonitoring equipment software.
ES "Treatment of chronic heart failure" (ES CHF) in the form of an electronic MDMS algorithm is built on the clinical guidelines expertise base “Heart failure: (CHF) and acute decompensated herat failure (ADHF). Diagnostics, prevention, treatment” [12].
Integrated in the above mentioned CHF ES algorithm has 8 steps and 2304 expert solutions. In the process of algorithmic search the following parameters are taken into account: EF, HR, systolic AP, duration of the QRS interval, the presence or the absence of left His' bundle branch block (measured remotely, e.g., via PC-aided hemodynamic analyzer Cardiocode); CHF functional class (FC), the presence or the absence of congestion (defined from the patient’s survey).
At the first stage, a basic plan of treatment is determined; taken into account are the following:
-
a) actual EF values and FC (Figure 1).
-
b) systolic AP, HR and tolerability of angiotensin-converting enzyme inhibitors (ACEi) and beta-blockers (BB) (Figure 2).
Issue 17. November 2020 | Cardiometry | 45
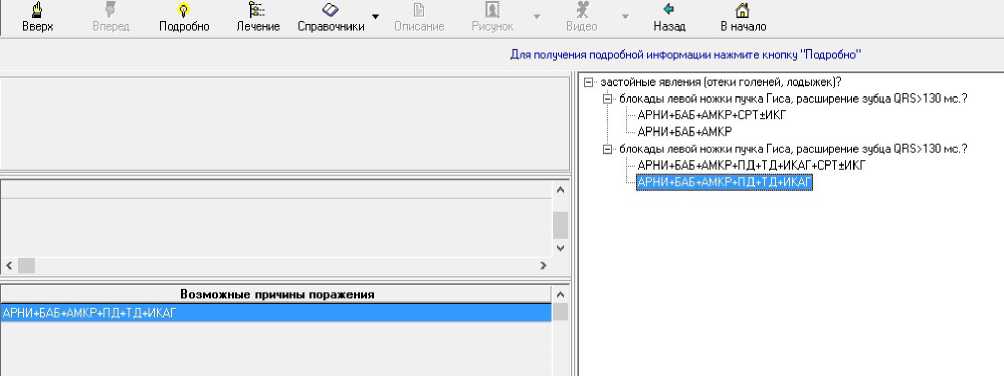
Figure 3. The 3rd stage of algorithmic search (determination of basic plan of treatment)
Table 2
Criteria for determining the treatment strategy and tactics under various forms of arrhythmias
|
Form of arrhythmia |
Instrumental criteria |
Clinical criteria |
|
Atrial fibrillation and flutter |
EF (or and) left ventricular wall thickness greater than 1.5 cm, value of AP and HR |
Primary or recurrent paroxysms |
|
Supraventricular tachycardia, supraventricular tachycardia |
EF (or and) left ventricular wall thickness greater than 1.5 cm, value of AP and HR, structural lesions of the myocardium (ischemia, AMI, CHF) |
|
|
Ventricular arrhythmias |
The form of ventricular tachycardia, prolongation of interval QT, EF (or and) left ventricular wall thickness greater than 1.5 cm, value of AP and HR, structural lesions of the myocardium (ischemia, AMI, increased heart dilatation) |
Primary or recurrent paroxysms, progression of attacks, growth of CHF signs |
Substituting the values of the corresponding indicators determined is the basic plan of treatment. For example, for a combination of EF <35%, FCIII, SAP> 100 mm Hg, HR 70-90 bpm the basic plan is the following: ARNI + BB + AMKR, where ARNI -angiotensin receptors and neprilysin inhibitors, BB - beta-blocker, AMCR - mineralocorticoid receptor antagonists.
At the second stage of the algorithmic search specified is the basic plan of treatment; taken into account are the presence or the absence of stagnation, incomplete LBBB and the QRS duration (see Figure 3 herein). In the presence of stagnation, QRS <130 ms and no signs of LBBB, the basic plan of treatment is the following: ARNI+BB+AMCR + LD + TD + CAIs, where LD are loop diuretics, TD are thiazide diuretics, CAIs are carbonic anhydrase inhibitors.
At the final stage of the algorithmic search specified is the final treatment plan which takes into account the contraindications and patient tolerability of medical drugs used in the basic plan.
Telecardiomonitoring capabilities allow designing the automated HSS for diagnostics and treatment of other cardiovascular diseases, depending on the cri-
46 | Cardiometry | Issue 17. November 2020
teria applied to selecting the strategy and tactics of treatment. For example, an analysis of clinical guidelines regulating the treatment of arrhythmias shows the possibility of developing an appropriate HSs (see Table 2 herein) [13-16].
The restriction on the proper selection of antiar-rhythmic drugs is imposed due to abnormalities of A-V conduction (amiodarone, BB, procainamide, propafenone, sotalol), sinus node disease (amiodarone, procainamide, propafenone, verapamil), lengthening of interval QT (amiodarone), bradycardia (amiodarone, BB, propafenone, sotalol, verapamil), intraventricular conduction disturbances (procainamide, propafenone), AF (propafenone, verapamil), the presence of accessory pathways (verapamil). All the above parameters can be identified by cardiac monitoring (e.g., using the Cardiocode device).
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Prospects for cardiovascular system telemonitoring in solving tasks in federal national project “Generation seniors”
- National Federal Project "Generation Seniors". Avail¬able online: http://www. rosmintrud.ru. [in Russian]
- Yakushin MA, Drovnikova LV. Tactics of man¬agement of patients in older age groups taking into account age polymorbidity. Uspekhi gerontologii. 2015;28(2):381–6. [in Russian]
- Medvedev OS, Yatskovsky MYu. Mobile healthcare (m-health) and health monitoring in modern medicine. Remedium. Journal of the Russian market of medicines and medical equipment. 2013;9:8-15. [in Russian]
- Bobyleva LA, Mikryukova EYu. Information and communication technologies in cardiology. In the col-lection: Theory and practice of priority research Col¬lection of scientific papers on the materials of the III International scientific and practical conference. 2018. p. 33-35. [in Russian]
- Kotenev DD, Kanishchev VV. Development of a hu¬man condition monitoring system based on data on heart rate variability. Issues of science and education. 2018;8(20):36-9. [in Russian]
- Podolsky MD, et al. Modern systems for rapid assess¬ment of the state of the human cardiovascular system based on electrocardiogram analysis. Cardiovascular therapy and prevention. 2016;15(5):92-96. [in Russian]
- Saraiva AP, Sousa MCB, Nunes J. The ideal user profile for telemedicine services – the Portuguese experience. Journal of telemedicine and e-health. 2017;3(5):144-8. [in Russian]
- Amadaev AA, Gunasheva ZYa, Isaev TM. Features of the application of the phenomenon of telemedicine in foreign and Russian practice. Management of so¬cio-economic systems: theory, methodology, collection of articles of the III International scientific and practical conference. In 2 parts. 2017. Pp. 186-195. [in Russian]
- Kobrinskiy BA. Telemedicine in practical health¬care. Moscow-Berlin: Directmedia, 2016; 238 p. Rus¬sian [in Russian]
- van Solingen R., Berghout E., van Latum F. In¬terrupts: Just a minute never is. IEEE Software 1998; 15(5):97–103.
- Czerwinski M, Horvitz E, Wilhite S. A diary study of task switching and interruptions. In: Proceedings of the SIGHCI Conference on Human Factors in Com¬puting Systems 2004. pp. 175–182.
- Kupriyanov RV, et al. Experience of implementing a call center in the activities of a budget medical orga¬nization (on the example of the ICDC). Health man¬ager. 2017;3:63-70. [in Russian]
- Maksimov IB, et al. History, analysis of the state and prospects of telemedicine development. Journal of tele¬medicine and e-health. 2018;3(8):103-10. [in Russian]
- Rudenko MYu, Zernov VA. Individual telemedi¬cine: what is it and what awaits us in the near future. Glavny vrach yuga Rossii. 2017;4(57):23-4. [in Russian]
- Dokuchaev VA, Yuvchenko ON. Analysis of the architecture and features of the multimedia contact center of a medical institution. T-Comm: Telecommu¬nications and transport. 2012;6(5):41-8. [in Russian]
- Medvedev OS. Remote monitoring and control of the patient using mobile technologies. CONNECT. 2011;5:2–4. [in Russian]
- Smyshlyaev AV, Melnikov YY, Artemova PV. For¬eign experience of state regulation of healthcare in the field of telemedicine technologies application. Prob¬lems of economics and legal practice. 2018;4:207-11. [in Russian]
- Cruickshank. What can the NHS learn from ex¬perience at the US Veterans Health Administration? J. Telehealth. January. 2012. Published by 2020 health.org http://www.2020health.org/2020health/ Publica¬tion/NHSit/Telehealth.html. 2.
- Dang S, et al. Evaluating the evidence base for the use of home telehealth remote monitoring in el-derly with heart failure. Telemedicine J. and e-health. 2009;15(8):783–96.
- Beale S, Sanderson D, Kruger J. Evaluation of the Telecare development Programme. Final Report. Ed-inburgh: Scottish Government, 2009. Р. 1–115. http://www.jitscotland.org.uk/downloads/1235404195- B59058%20Final%20Report%20low%20res.pdf.
- Information systems in the economy / ed. by G. A. Titorenko, Moscow: Unity-Dana, 2008. [in Russian]
- Lipsky SP, Egorov EV. Use of modern information technologies in improving the efficiency of the health care system in the Russian Federation on the example of telemedicine. Bulletin of the North Ossetian state University named after K. L. Khetagurov. 2014;2:249-52. [in Russian]
- Maksimov IB, et al. History, analysis of the state and prospects of telemedicine development. Journal of tele¬medicine and e-health. 2018;3(8):103-10. [in Russian]
- Efimenko IV, Khoroshevsky VF. Intelligent de¬cision support systems in medicine: a retrospective review of the state of research and development and prospects. Open semantic technologies for designing intelligent systems. 2017;7:251-60. [in Russian]
- Medvedev OS, yatskovsky MYu. Mobile healthcare (m-health) and health monitoring in modern medicine. Remedium. Journal of the Russian market of medicines and medical equipment. 2013;9:8-15. [in Russian]
- Roberts L. 9 Billion? Science. 29 July 2011;333:540–3.
- Vladzimirsky AV, Lebedev GS. Telemedicine. Mos¬cow: GEOTAR-Media, 2018. 570 p. [in Russian]
- Telemed. technologies: UNITEDHEALTH GROUP T-Comm: Telecommunications and transport . 2009; 3(5):43. [in Russian]
- Yakushin M. A., et al. Expert system for monitor¬ing and correction of indicators by the hemodynam¬ic system in solving strategic public health problems. Practical medicine. 17(5):241-9. [in Russian]
- Yakushin MA, Goryanov AD. Computer program for construction and operation of medical diagnostic algorithms and information databases "Neurodoctor". Certificate No. 2004610806 of the Russian patent and trademark agency, dated March, 31, 2004. [in Russian]
- Clinical guidelines on PRAS-cardiology-internal medicine "Heart failure: chronic (CHF) and acute de-compensated (ADHF). Diagnostics, prevention, treat¬ment". Cardiology. 2018;58. [in Russian]
- Clinical guidelines of the Russian Ministry of health on "Ventricular arrhythmias in adults», 2016. [in Russian]
- Clinical guidelines of the Russian Ministry of health on "Atrial Fibrillation and flutter in adults»,2016. [in Russian]
- Clinical guidelines of the Russian Ministry of health on "Supraventricular rhythm disorders in adults»,2016. [in Russian]
- ESC guidelines on the treatment of patients with ventricular arrhythmias and prevention of sudden cardiac death, 2015, European Society of Cardiolo¬gy (ESC) working group on the treatment of patients with ventricular arrhythmias and prevention of sud¬den cardiac death.


