Research study on the efficiency of a defibrillating biphasic pulse of various durations based on mathematical modeling and simulation of a cardiomyocyte
Автор: Chernov N.N., Bezverkhii A.A.
Журнал: Cardiometry @cardiometry
Статья в выпуске: 18, 2021 года.
Бесплатный доступ
The paper presents the results of our research study on the impact of different durations of a biphasic rectangular pulse on the efficiency of the defibrillating action based on modeling and simulation of a cardiomyocyte in the framework of Cell Electrophysiology Simulation Environment. We used Luo-Rudy Mammalian Ventricular Model II (dynamic) as the mathematical model of the biochemical processes, which occur both on the surface and inside a cardiomyocyte in a guinea pig. An analysis of the obtained results allowed us to determine the optimal time of the defibrillating pulse. It has been shown that a pulse of 4 ms duration has the highest efficiency. The research has been carried out directly based on the mathematical model and simulation of the cardiomyocyte that makes it possible to minimize errors which may occur in experiments on animals
Transthoracic defibrillation, biphasic pulse, current stabilization, cardiomyocyte repolarization, ventricular fibrillation
Короткий адрес: https://sciup.org/148321611
IDR: 148321611 | DOI: 10.18137/cardiometry.2021.18.4449
Текст научной статьи Research study on the efficiency of a defibrillating biphasic pulse of various durations based on mathematical modeling and simulation of a cardiomyocyte
Nikolay N. Chernov, Aleksandr А. Bezverkhii. Investigation of the efficiency of a defibrillating biphasic pulse of various durations based on a mathematical model of a cardiomyocyte. Car-diometry; Issue 18; May 2021; p.44-49; DOI: 10.18137/cardiom-etry.2021.18.4449; Available from: issues/no18-may-2021/defibrillating-biphasic-pulse
According to numerous studies, 76% of the sudden cardiac arrests (SCA) are conditionally preventable cases, as they occur due to ventricular fibrillation (VF) 44 | Cardiometry | Issue 18. May 2021
[1-3]. Immediate electro-pulsed therapy (EPT) by external defibrillation is the main method of treating this type of arrhythmia [3-5]. The comparative study of modern forms of pulses carried out earlier made it possible to identify the concept of development of this field in science [6]. An analysis of the reference literature and the results of recent developments are conditions to define the key parameters of the pulse for an individual selection of the characteristics of the transthoracic defibrillation signal. The representation of the average current (I) and charge (Q) in the form of a certain function I (t) is the best way to dose the defibrillation pulse [7].
The calculation of the main parameters was carried out based on the work by Weiss and Lapicque [8], who proved the existence of the effect of cardiac tissue stimulation, and according to the calculations made by Blair, who described the existence of a rheo-base [9, 10]. Studies by Irnich define in detail the effect of a pulse exposure time on cardiomyocytes as the key pulse parameter [11, 12]. Later, a large number of studies have proven in practice the high efficiency of a two-phase pulse against the single-phase one. There is still no theoretical justification for this evidence available, but there is a hypothesis that the second phase prevents the appearance of ectopic foci in the heart tissue that increases the effectiveness of defibrillation [13-17]. A detailed calculation of the ratio between the forward and the reverse pulse signals was conducted by Kroll, who demonstrated the possibility of minimizing the energy of the second phase [18], and many developers subsequently confirmed the large variation of the current amplitude tolerances [14]. The fact cannot be ignored that the phase switching time should not exceed 1 ms and be possibly minimized, otherwise the biphasic signal converts into two monophasic signals [19]. Bourlands in his paper in 1978 showed the comparative efficiency of pulses with a time constant, regardless of the chest impedance [20]. An unfairly neglected publication by Schuder in 1964 confirms the high efficiency of the rectangular pulse as compared with other pulse variants [13]. In 1993, Tucker has presented a graph derived from his analysis and proven that there is a delicate balance between an effectiveness of defibrillation and damage produced by each pulse [21]. In 1988 Wilson described the effect of charge building-up due to multiple defibrillations
-
[22] . Fishler summarized all the experiments in 2000 and determined the time interval for a rectangular pulse in the range from 3 to 6 ms and the ratio of the current amplitude of the first and second phases as 15A to 10A, respectively [23].
The aim of the our research work is to study the efficiency of a biphasic rectangular pulse using mathematical modeling and simulation of a cardiomyocyte.
Materials and methods
An acceptable range of the time interval has been obtained by analyzing the reference literature and applying our own calculations. Experimental studies can be the next stage of optimizing the time interval of the pulse impact in question [7,23]. For the purpose of a humane approach to the study, we have completed signal modeling and simulation, and the obtained results have been objectified by with mathematical modeling in the Cell Electrophysiology Simulation Environment (CESE) [24]. Mathematical model Luo-Rudy Mammalian Ventricular Model II (dynamic) to simulate the biochemical processes occurring on the surface and inside the guinea pig cardiomyocyte has been applied. With the help of this model, it is possible to simulate an impact made by an electric pulse of a certain duration, shape and intensity by current strength on the cell membrane and obtain curves of the ion channels operation, changes in the concentration of ions on the surface and inside the cardiomyocyte.
Using the Java programming language, a rectangular signal of sufficient intensity to overcome the threshold of cardiomyocyte excitability was coded and implemented in the CESE. Taking into account the reference literature data and our own calculations [6,7], several rectangular signals with a duration of 3 to 6 ms with a step of 1 ms were selected for an analysis to identify the optimal pulse duration. The earlier experiments showed a difference in the duration of threshold pulses for the Luo-Rudy Mammalian Ventricular Model II (dynamic) cardiomyocyte and the results for the human cardiomyocyte model. The 11 ms pulse for the Luo-Rudy model was identical in its effects to the 4 ms signal in the human cardiomyocyte model [26, 27], i.e., the ratio of the pulse duration in the model used to that in the human cardiomyocyte model is 1: 2.75. In this regard, it was decided to introduce a correction factor for the pulse duration: Kt = 2.75.
Let us find the voltage on the surface of the membrane (membrane voltage (mV)) as the main param- eter under consideration. The membrane resting potential (MRP) is constantly available on the surface of the membrane, and it is formed mainly due to the diffusion of the Na+ and K+ions. The MRP value of a cardiomyocyte is approximately 86 mV [28]. When an electric pulse is applied to the cell membrane, depolarization occurs, and an action potential (AP) is generated on its surface. AP of the cardiomyocyte is fired at a voltage of 56 mV. In this case, the protein channels of the cell membrane are activated, and the Na+ ions enter the cell. The Na+ ions come into the cell according to the "all or nothing" principle, so the fact of AP generation can be clearly traced by the change in the velocity of the Na+ ions travelling through the membrane [29]. The given mathematical model allows us to construct a graph to depict the Na+ ion flow (Total Na ion flow (mM/ms)), and we can use it as a criterion for the efficiency of the signals under consideration.
In the repolarization phase, active cellular channels are involved, the operation of which is aimed at restoring the MRP value. The calcium ions play an important role at the repolarization stage. Their function is to maintain MRP at a certain level (86mV), and, with a decrease in their concentration, the excitability of the cell decreases. The maintenance of the Ca2+ concentration is regulated by the Na+ / Ca2+pump, and, as a rule, its operation is aimed at pumping Ca2+ out of the cell using the Na+ / Ca2+pump [30]. The peculiarity of the Na+ / Ca2+pump is the exchange of one Ca2+ ion for three Na+ ions. It follows from this that the overload in the operation of this mechanism, associated with an excessive entry of the Na+ ions, may lead to a reduction in the excitability of the cardiomyocyte [31]. To evaluate the efficiency of the defibrillation pulses in the model in our study, a plot was used that reflects the activity of the Na+ / Ca2+pump - Na-Ca exchanger current (uA/uF). A comprehensive analysis of the above parameters allows evaluating the efficiency of the pulses and assess their safety.
Results and Discussion
The pulse impact process was simulated in the framework of the CESE using the Luo-Rudy Mammalian Ventricular Model II (dynamic), with the proper rectangular signal of sufficient intensity to form an AP. The change in the duration of the rectangular pulse in CESE is performed by manual correcting of the required parameter: this function is called clamp of the parameter, namely, it is the stimulus duration. As de
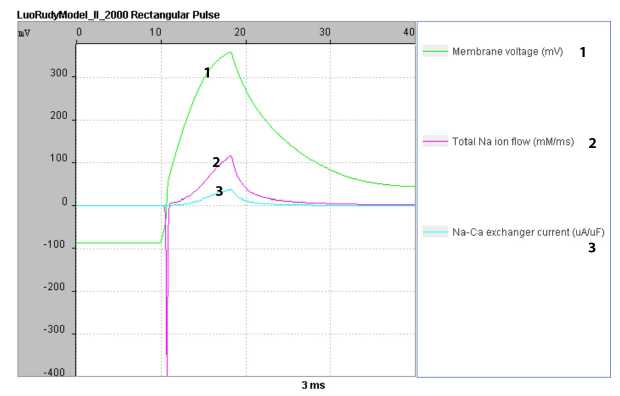
Figure 1. Mathematical modeling of changes in the parameters of the voltage on the cardiomyocyte membrane surface, the Na+ transmembrane current and the Na+ - Ca2+ pump activity, when exposed to an equivalent pulse with a duration of 3 ms
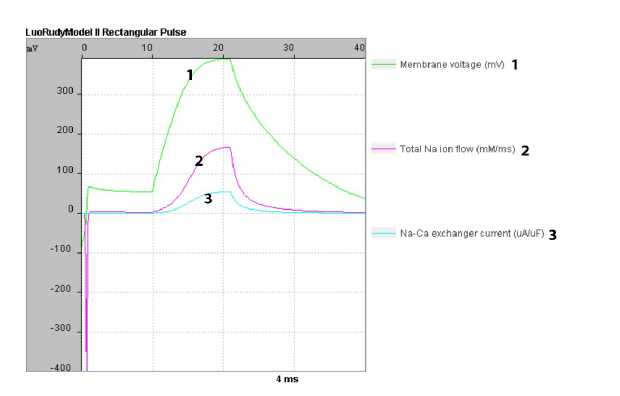
Figure 2. Mathematical modeling of changes in the parameters of the voltage on the cardiomyocyte membrane surface, the Na+ transmembrane current and the Na+ - Ca2+ pump activity, when exposed to an equivalent pulse with a duration of 4 ms
scribed above, from earlier studies, in order to obtain results applicable to the human cardiomyocyte, it is necessary to introduce a correction factor Kt. After the correction, the pulse duration was the following: 8.25 ms (4ms), 11 ms (4ms), 13.75 (5ms) and 16.5 (6ms).
In the simulation environment, some summary plots were constructed showing changes in the membrane surface voltage (mV), the Na+ ion flow (Total Na ion flow(mM/ms)), and the Na+ / Ca2+ pump activity (Na-Ca exchanger current (uA/uF)) for each pulse separately.
When considering the plot produced by simulating a signal with a duration equivalent for a pulse of 3 ms (8.25 ms), as shown in Figure 1 herein, the following data are obtained: action potential (AP = -56 mV) develops at 0.35 ms, and the opening of the Na+ channels takes place at 0.4 ms. In this case, the reverse flow of the Na+ ions begins immediately after closing and reaches its peak at 4.2 ms, followed by a smooth decline. The operation of the Na+ / Ca2+ pump on the curve follows the dynamics of restoring the Na+ balance. In general, the effect made by a rectangular pulse with its duration of 3 ms can be characterized as sufficient to provide general repolarization. The pulse creates conditions for a standard contraction considering duration and activity of the ion channels [32].
In Figure 2 herein, obtained by simulating a pulse with a duration of 4 ms (11 ms under the simulation conditions in the context of the presented model), the formation of AP also occurs at 0.35 ms, and the opening of the Na+ channels is found at 0.4 ms. The respective curve shows the key difference between the 3 and 4 ms pulses: a plateau appears on the cell membrane from 0.9 ms till 10.1 ms with an average amplitude of 46 | Cardiometry | Issue 18. May 2021
64 mV. Due to this plateau, the reverse current of the Na+ ions and their active transport from the cardiomyocyte cell are locked. The operation of the Na+ / Ca2+ pump shows a smooth start and shutdown, and it is a true illustration of the Na+ions current dynamics. The formation of the locking plateau on the cardiomyocyte membrane surface reflects the very essence of defibrillation, which consists in creating general repolarization for every cell in the heart tissue.
When analyzing the pulse of the 5 ms duration (13.25 ms for the model in question), as illustrated by Figure 3, the formation of AP and the opening of the Na+ channels are similar to the previous results, which have been recorded to be 0.35 and 0.4 ms, respectively. Attention should be drawn to the absence of a plateau that is the same case with the 4 ms pulse and to the formation of the first peak on the membrane surface at 3.7 ms with amplitude of 238 mV. At the same time, the first peak in the velocity of the reverse flow of the Na+ ions is also noted. A detailed analysis of the data from the simulation revealed a pattern: the active current of the Na+ ions from the cell begins at the membrane surface voltage of more than + 80 mV. Further decrease and re-rise of the membrane voltage is accompanied by the synchronous activity of the Na+ ion current and the operation of the Na+/Ca2+ pump. The total operating time of the Na+/Ca2+ pump is 19 ms (from 1.35 ms to 30.35 ms). And if we address the fact that the duration of the Na+ channels opening is 0.6 ms for any pulse duration, and the maximum velocity does not have a significant difference (395 – 398 mmol/ms), we can conclude about the excess transport of Na+ from the cardiomyocyte cytoplasm. It should be mentioned that this involves the transport of Ca2+ ions into the
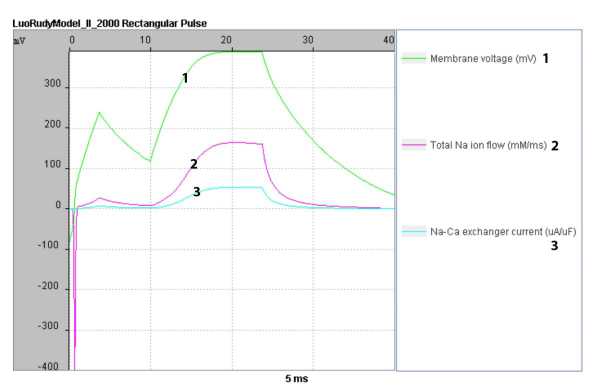
Figure 3. Mathematical modeling of changes in the parameters of the voltage on the cardiomyocyte membrane surface, the Na+ transmembrane current and the Na+ - Ca2+ pump activity, when exposed to an equivalent pulse with a duration of 5 ms
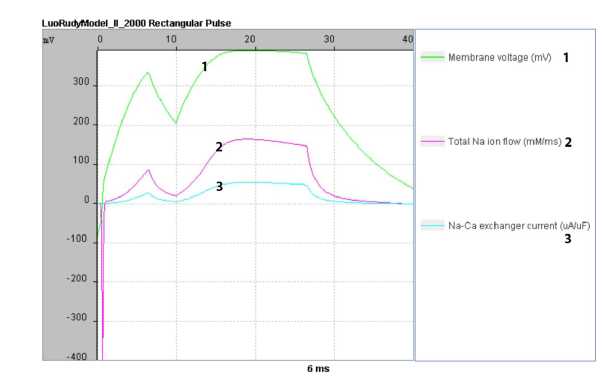
Figure 4. Mathematical modeling of changes in the parameters of the voltage on the cardiomyocyte membrane surface, the Na+ transmembrane current and the Na+ - Ca2+ pump activity, when exposed to an equivalent pulse with a duration of 6 ms
cell and, as a result, a decrease in the excitability of the cardiomyocyte [31]. From the results of modeling and simulation of the rectangular pulse with an equivalent duration of 5 ms, it can be concluded that prolonged exposure of a cardiomyocyte to a high-density current leads to excessive transport of the Ca2+ and Na+ ions inside the cell and on its surface, respectively.
The further increase in the pulse duration to 6 ms (16.5 ms in the model under study) confirms the conclusions drawn from the previous simulation. High voltage on the membrane surface induces an active ion substitution transport, which leads to a decrease in the concentration of the Ca+ ions on the cardiomyocyte membrane surface and, as a result, a decrease in the excitability of the cell, including for subsequent defibrillating pulses. Figure 4, which shows the curve of a pulse of the 6 ms equivalent duration, characterizes it as redundant for all the studied parameters.
As a result of modeling, we obtained the respective curves characterizing the response of a cardiomyocyte to rectangular pulses of different durations. Using this study, it is possible to evaluate the main processes of the cell excitability: the formation of AP under a shortterm exposure to a defibrillating pulse, the repolarization of the membrane and the restoration of MRP.
Conclusions
The aim of our research study was to study the efficiency of a biphasic rectangular signal of various durations using the cardiomyocyte simulation in the framework of mathematical modeling system CESE. Using our analysis of the obtained results, we determined the optimal time of the defibrillating pulse extracted from the range produced by analyzing the data of some pre- vious studies and calculations [7]. It has been shown that a pulse of 4 ms duration has the highest efficiency. Our research study has been carried out directly with the use of the mathematical model and simulation of a cardiomyocyte that makes possible to minimize errors that may occur during the experiment on animals. Differences in the thorax geometry in animals may result in a great number of difficulties in applying the results to human individuals, and the mathematical modeling for studying the time interval can be treated as a more preferable option. The next step in designing a biphasic pulse is to calculate the optimal current amplitude for the most efficient defibrillation, taking into account the varying chest impedance in a patient.
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Research study on the efficiency of a defibrillating biphasic pulse of various durations based on mathematical modeling and simulation of a cardiomyocyte
- Ringh M, Herlitz J, Hollenberg J, Rosenqvist M, Svensson L. Out of hospital cardiac arrest outside home in Sweden, change in characteristics, outcome and availability for public access defibrillation. Scandinavian journal of trauma, resuscitation and emergency medicine 2009; 17: 18.
- Hulleman M, Berdowski J, de Groot JR, et al. Implantable cardioverter defibrillators have reduced the incidence of resuscitation for out of hospital cardiac arrest caused by lethal arrhythmias. Circulation 2012; 126: 815–21.
- Blom MT, Beesems SG, Homma PC, et al. Improved survival after outofhospital car diac arrest and use of automated external defibrillators. Circulation 2014; 130: 1868–75.
- Weisfeldt ML, Sitlani CM, Ornato JP, et al. Survival after application of automatic external defibrillators before arrival of the emergency medical system: evaluation in the resuscitation outcomes consortium population of 21 million. J Am Coll Cardiol 2010; 55: 1713–20.
- Berdowski J, Blom MT, Bardai A, Tan HL, Tijssen JG, Koster RW. Impact of onsite or dis patched automated external defibrillator use on survival after out_of_hospital cardiac arrest. Circulation 2011; 124: 2225–32.
- Nikolay N. Chernov, Aleksandr A. Bezverkhii, Vladimir I. Timoshenko. Evaluation of general repolarization of cardiomyocites with biphasic pulses of different shapes. Cardiometry. May 2020;16:80-4; DOI: 10.12710/cardiometry.2020.16.8084; WOS:000539041400010;
- Nikolay N. Chernov, Oksana I. Korotkova, Aleksandr A. Bezverkhii. Systematic design of optimized pulse shape for transthoracic defibrillation. Cardiometry. November 2020;17:34-8; DOI: 10.12710/cardiometry.2020.17.3438;
- Lapicque L. Denition experimentelle de l'excitabilite. Proc. Soc. deBiol. 1909;77:280-25.
- Blair HA. On the Intensity-Time Relations for Stimulation by Electric Currents I. J. Gen. Physiol. Jul 1932;15:709-29.
- Blair HA. On the Intensity-Time Relations for Stimulation by Electric Currents II. J. Gen. Physiol. 1932;15(6):731-55.
- Irnich W. The fundamental law of electrostimulation and its application to debrillation. Pacing Clin Electrophysiol. Nov 1990;13:1433-47.
- Irnich W. Optimal truncation of defibrillation pulses. Pacing Clin Electrophysiol. Jun 1995;18:673-88.
- Schuder JC, Stoeckle H, Dolan AM. Transthoracic Ventricular Defibrillation with Squarewave Stimuli: One-Half Cycle, One Cycle, and Multicycle Waveforms. Circ Res. 1964;15(3):258-64.
- Schuder JC, Rahmoeller GA, Stoeckle H. Transthoracic Ventricular Defibrillation with Triangular and Trapezoidal Waveforms. Circ Res. 1966;19(10):1524-71.
- Schuder JC, et al. Transthoracic ventricular defibrillation in the 100 kg calf with symmetrical one-cycle bidirectional rectangular wave stimuli. IEEE Trans Biomed Eng. Jul 1983;30:415-22.
- Chapman PD, et al. Strength-duration curves of fixed pulse width variable tilt truncated exponential waveforms for nonthoracotomy internal defibrillation in dogs. Pacing Clin Electrophysiol. Jul 1988;11:1045-50.
- Bardy GH, et al. A prospective randomized evaluation of biphasic versus monophasic waveform pulses on defibrillation efficacy in humans. J Am Coll Cardiol. Sep 1989;14:728-33.
- Kroll M. A minimal model of the single capacitor biphasic defibrillation waveform. Pacing and Clinical Electrophysiology. 1994;17:1782-92.
- Cooper RA, et al. The effect of phase separation on biphasic waveform defibrillation. Pacing Clin Electrophysiol. Mar 1993;16:471-82.
- Bourland JD, et al. Comparative efficacy of damped sine wave and square wave current for transchest ventricular defibrillation in animals. Med Instrum. 1978;12(1):42-5.
- Tacker W. Defibrillation of the Heart: ICDs, AEDs, and Manual. St. Louis: Mosby - YearBook, 10 1993.
- Wilson CM, et al. Death and Damage Caused by Multiple Direct Current Shocks: Studies in an Animal Model. European Heart Journal. 1988;9(11):1257-65.
- Fishler M. Theoretical Predictions of the Optimal Monophasic and Biphasic Defibrillation Waveshapes. IEEE Transcadtons on Bimedical Engineering. 2000;47(1):59-67.
- http://www.simulogic.com/products/platforms/
- Faber GM, Rudy Y. Action Potential and Contractility in [Na+]i Overload Cardiac Myocytes. Biophysical Journal. Vol. 78 №5 pp. 2392-2404.
- Gorbunov BB. The study of the properties of the membrane of myocardial cells on the Luo-Rudy model. Medical equipment. 2012; 3: 32—34. [in Russian]
- Cansell A. Wirksamkeit und Sicherheit der Impulskurvenformen bei transthorakaler Defibrillation. Notfall & Rettungsmedizin. 1998; 1 (6): 372—380. http://dx.doi.org/10.1007/s100490050087
- Normal human physiology / ed. by B. I. Tkachenko. - 2nd ed. - M.: Medicine, 2005. - P. 115. - 928 p. - ISBN 5-225-04240-6 [in Russian]
- Gaiton A. K., Hall D. E. Medical Physiology.Textbook of Medical Physiology / Ed. IN AND. Cobrina. Moscow: Logosphere, 2008. P. 113. 1296 p. - ISBN 978-5-98657-013-6 [in Russian]
- Bers DM. Cardiac excitation-contraction coupling. Nature. 415 (6868): 198–205. doi:10.1038/415198a
- Koeppen BM, Stanton BA. Berne & Levy Physiology. — 6th edition. — Philadelphia: Mosby/Elsevier, 2008. — С. 295. — 834 с. — ISBN 0323045820
- Hamill OP. Ion transport by single receptor channels. Cold Spring Harbor Symp. Quant. Biql. 1983; 48: 247-57.


