Resorbable implants in paediatric orthopaedics and traumatology
Автор: Lascombes P., Journeau P., Popkov D.A.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 6 т.29, 2023 года.
Бесплатный доступ
Background Development of resorbable implants for paediatric orthopaedics is promising as there is no need for implant removal.The aim of this paper is to present our experience in resorbable implants in paediatric traumatology, and to make an overview of the recent literature.Material and methods In our department of paediatric traumatology and orthopaedics, we have operated 7 children with fractures of long bones with resorbable screws (ActivaScrew™). The inclusion criteria were intra-articular and juxta-articular fractures in children with an indication for screw fixation. To prepare the review, we searched for information sources at the scientific platforms such as PubMed, Scopus, ResearchGate, RSCI, as well as other published products (Elsevier, Springer).Results The cohort is represented by 7 patients, 4 girls and 3 boys, aged from 5 to 14 years old. The 7 fractures were 3 at the elbow and 4 at the ankle joint. In the immediate postoperative period, no patient presented with abnormal swelling, redness, or tissue reaction. Pain disappeared at day 7 in all cases. Weight-bearing and return to sport activities were allowed in normal delay. Radiological bone union was obtained between 3 and 6 weeks. Range of motion in adjacent joints was comparable to the opposite non-fractured side at 3 months. There were no cases of complications, no infection, and no need for a reoperation.Discussion The use of resorbable implants, either co-polymers or magnesium, solves the problem: removal of implants is not anymore necessary. Resorbable implants are becoming safer as they have good solidity allowing bone union of fractures and osteotomies before their eliminating.Conclusion Main indications of resorbable implants in pediatrics remain fractures and osteotomies fixed with screws. The development of plates and intramedullary nails will enlarge the indications. Level of evidence: IV.
Paediatric fracture, resorbable implants, co-polymer, magnesium
Короткий адрес: https://sciup.org/142240033
IDR: 142240033 | УДК: 616.71-001.5-089.227.84-003.95-053.2 | DOI: 10.18019/1028-4427-2023-29-6-629-634
Текст научной статьи Resorbable implants in paediatric orthopaedics and traumatology
The surgical treatment of paediatric fractures usually requires their fixation with metallic implants, made of stainless steel or titanium. Main indications of internal fixation are intraarticular fractures classified as Salter
III and IV types and diaphyseal fractures which cannot be treated with conservative methods. The former need most often screw fixation via an open or a closed approach. On many occasions, diaphyseal fractures are treated with
intramedullary fixation. The first choice is the flexible nailing technique in forearm and humerus fractures, and in femur and tibia fractures before the end of growth. The advantages of metallic implants are well-known, but among their disadvantage, one question is permanent: removal or not? In one hand, the future is uncertain in case of a need for orthopaedic surgery. To remove implants after a long term may be a nightmare. But on the opposite, the removal of implants needs a second surgery, and complications are not negligible. In addition, the use of those devices can entail complications as hematomas, healing problems, local sepsis.
For these reasons, the development of resorbable implants is promising as there is no need for implant removal. But resorbable implants must be safe. This means they must have a comparable efficiency with classic metallic implants to stabilize the fractures: firstly, stability and resistance of the implants are mandatory till bone union is obtained; secondly, absence of free debris which might damage some tissues like brain, liver, ganglions, lungs. For that reason, some resorbable implants used in the past have been withdrawn from the market due to some complications as intraarticular synovitis and spread of debris.
Interference screws [1] and absorbable anchors are currently used in tendons and ligaments reconstruction. In adult trauma, some fractures of the ankle are treated with absorbable plates and screws. The biomechanical stability of these implants has shown excellent qualities and biological properties.
One category of resorbable or biodegradable materials is a polymer that has been used for around 40 years in many surgical applications. Initially used just for sutures, resorbable plates and screws are commonly used in maxillofacial surgery, such as for osteotomy syntheses or mandibular fractures. A second group of resorbable implant is the new generation of magnesium implants: experimental studies demonstrate their good tolerance and nice results. The first clinical studies show good results too.
The main goal of this paper is to present our experience with resorbable implants in paediatric traumatology, and to make an overview of the recent literature.
MATERIAL AND METHODS
In our level I department of paediatric traumatology and orthopaedics, we operated on 7 patients with fractures of long bones with resorbable screws, partially threaded ActivaScrew™ LAG (Bioretec). The decision to select these new implants was taken under following consideration: absence of debris and urine elimination of the polymer polylactide-co-glycolide (PLGA), strong fixation ability till bone union .
The inclusion criteria were intra-articular and juxta-articular fractures in children with an indication for screw fixation, and acceptation of the patient and the family for a resorbable implant after given precise information. The exclusion criteria were pathological fractures.
Surgical technique Reduction of the fractures was obtained either by closed method and mini-invasive approach or by open approach with the same technique as in fixation with conventional metallic screws. One hole by screw was performed strictly into the epiphysis with a drill smaller than the diameter of the screw under the C-arm control to be parallel to both physis and joint (Fig. 1), thus a drill of 2.5 mm diameter was used for a screw of 3.5 mm diameter. Then, the cortex was enlarged with a countersink to bury around 50 % of the screw head. The adapted tap, 3.5 mm for 3.5 mm screws, is mandatory to be used. Just before insertion, the screw was dipped in a contrast fluid expecting to be visible on the C-arm control, but unfortunately it was not always visible. Finally, the screws were inserted with an adapted cap. At that moment, the first screw was not yet tightened. A second screw, of the same size, same technique was inserted almost parallel to the first one. Then, we tightened both screws: we just turn the screwdriver till the adapted system pulled out. It is not recommended to continue tightening the screws themselves as their head may break, leading to a complete loosening of the compressive effect on the fracture.
Imaging control should demonstrate the fracture line to disappear completely, proof of an excellent reduction. An immediate arthrogram of the joint confirmed the satisfactory anatomical reduction of the fracture (Fig. 2). An immediate immobilization was done with a splint plaster cast, replaced three days later with a resin cast.

Fig. 1. Surgical technique: a – fracture with dislocation; b – reduction of the fracture and drilling of the epiphysis; c – screw with contrast fluid is visible on the C-arm control
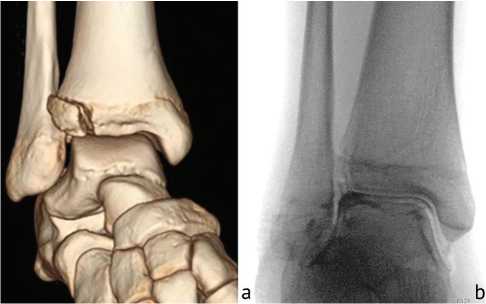
Fig. 2. Control of reduction: a – Tillaux fracture; b – fracture line disappeared, an immediate arthrogram confirms satisfactory anatomical reduction of the fracture
Assessed criteria were duration of the surgical procedure; presence or not of swelling, redness, tissue reaction, pain on day 1, day 7, and day 30; time for bone union, date of full weight-bearing, and range of motion at 3 months; date of return to sport activities; complications and reoperation rate.
RESULTS
The cohort is represented by 7 patients, 4 girls and 3 boys, aged from 5 to 14 years old. The 7 fractures were three at the elbow (Fig. 3) and four at the ankle joint. All of them were classified as intra-articular displaced fractures requiring anatomical reduction and stable screw fixation. The used resorbable screws were partially threaded, 3.5 mm diameter and of different length from 20 to 45 mm.
In the immediate postoperative period, day 1, 7 and 30, no patient presented with abnormal swelling, redness, or tissue reaction. Pain disappeared at day 7 in all cases. Weight-bearing and return to sport activities were allowed in normal delay. Radiological bone union was obtained between 3 and 6 weeks. Range of motion in adjacent joints was comparable to the opposite non-fractured side at 3 months. There were no cases of complications, no infection, and no need for a reoperation (Table 1).

Fig. 3. Medial epicondyle fracture: a – radiograph at admission; b – reduction and osteosynthesis
Table 1
|
Sex |
Age (years) |
Fracture |
Implants diameter/length |
Duration of surgery (minutes) |
Delay of bone union |
Delay of weight bearing |
Delay sport return |
Range of motion at 3 months |
Complication |
Follow-up |
|
Girl |
13 |
bimalleolar, ankle dislocation |
2 screws 3.5/45 mm 3.5/45 mm |
57 |
6 weeks |
6 weeks |
3 months |
comparable to opposite side |
no |
1 year |
|
Boy |
14 |
proximal first metatarsal bone Salter III |
1 screw 3.5/З0 mm |
S4 |
6 weeks |
6 weeks |
3 months |
comparable to opposite side |
no |
1 year |
|
Boy |
5 |
olecranon longitudinal |
2 screws 3.5/20 mm 3.5/20 mm |
87 |
4 weeks |
N/A |
3 months |
comparable to opposite side |
no |
9 months |
|
Girl |
14 |
distal tibia Salter III (Tillaux') |
1 screw 3.5/40 mm |
54 |
6 weeks |
6 weeks |
3 months |
comparable to opposite side |
no |
1 year |
|
Girl |
10 |
medial epicondyle |
1 screw 3.5/40 mm |
47 |
4 weeks |
played piano at 4 weeks |
3 months |
comparable to opposite side |
no |
3 years |
|
Girl |
12 |
medial malleolus |
1 screw 3.5/20 mm |
35 |
4 weeks |
4 weeks |
3 months |
comparable to opposite side |
no |
6 months |
|
Boy |
10 |
elbow dislocation lateral condyle fracture |
2 screws 3.5/24 mm 3.5/40 mm |
47 |
6 weeks |
N/A |
2 months |
comparable to opposite side |
no |
6 months |
Cases included in the study
DISCUSSION
Different polymers of lactic acid (PLA) and glycolic acid (PGA) have been proposed for orthopedic surgery both in adults and children [2, 3]. PLA implants are known as responsible of local reactions during absorption and rapid degradation which may cause instability before bone union. On the other hand, poly-(L)-lactic acid (PLLA) implants have a slow resorption and may lead to bone cavity filled with either fibrous tissue or fluid [4]. They may also cause local reaction as foreign-body reactions. As for others, the PLLA/PGA interference screw completely degraded, and no remnant was present 3 years after implantation for a bone-patellar tendon-bone graft ACL reconstruction [1].
In reconstruction of nerves, implantation of poly (DL-lactic acid) PDLLA film did not alter liver or renal functions. Pathologic examinations showed that implantation of PDLLA film did not cause pathologic changes to the rat liver, kidney, pancreas, or spleen. Taken together, these results suggest that PDLLA films have excellent biocompatibility and no obvious toxicity in vivo , and may be used to prevent nerve adhesion, thereby promoting nerve regeneration [2].
Poly lactic-co-glycolic acid (PLGA) has been developed as another component. This new resorbable implant slowly degrades while it reacts with water in the human body. It adds advantages of a mid-term resorption, with a good stiffness enough to obtain bone union, and without any type of inflammatory reaction [5, 6]. The degraded components are exhaled and excreted, the total elimination occurs within approximatively 2 to 3 years. Since theses implants do not include any metal, there is neither X-ray, ultrasound nor MRI disturbances [6, 7, 8].
In clinical practice, the advantages to avoid removal of implants have been widely emphasized [9, 10]. We had a previous experience with resorbable screws, 2.8 mm diameter made of poly-L-lactide- poly-D-lactide acid and trimethylene carbonate. Among 24 patients, we observed some complication like a loose screw head, joint stiffness and joint effusion [11].
Our short series demonstrate that resorbable screw osteosynthesis is justified in paediatric traumatology as this approach does not modify either the surgical technique or the follow-up care. The follow-up is comparable with classic metallic implants. We did not observe any abnormal mobility during the resorption period between the head and the body of the screw.
In a retrospective study, Kassai et al. [12] compared the fixation of the medial humeral epicondyle fractures with either a biodegradable poly L-lactide-co-glycolic acid (PLGA) or a traditional metallic implant. They observe normal delay for bone union, comparable results between both groups, and no specific complications with resorbable implants.
Varga et al. [13] published a comparative study of the treatment of 94 distal fractures of the radius, associated or not with ulna fractures. One group treated with one or two stainless steel Kirschner wires which were buried under the skin (n = 40), a second group with K-wire left outside (n = 24) and the third group with an original technique of distal radial elastic nailing with bioresorbable
PLGA pins (n = 30). There was no difference between the complication rates of both K-wires groups, while the complication rate of the bioresorbable group was significantly lower.
In 2013, Sinikumpu et al. [14] from Finland published a preliminary technical report of a mini-invasive technique forpediatricdiaphysealforearmfractureswithbioabsorbable elastic stable intramedullary nailing. They developed a two-stage surgical technique in children between 5 and 15 years old. The first stage was identical to the Nancy method [15, 16, 17]: mini-invasive approach, reduction of the fractures, introduction of metallic implants into the medullary canal of both bones through a metaphyseal small hole, and fixation of the radius and ulna. The second part of the technique was a careful removal of each metallic implant, each of them being immediately replaced by an absorbable rod (made of poly lactide-co-glycolide (PLCG) developed by the Bioretec company, first in the radius and second in the ulna, or reverse.
Recently, an international Europe-based, multicenter, prospective, single-arm, open-label study has evaluated the elastic stable intramedullary nailing of forearm fractures in children between age 3 and 13 with a resorbable Activa IM-NailTM. Seventy-six patients with a mean age at inclusion of 8.9 ± 2.4 years have been operated on. The mean time of operation was 58.9 ± 22.9 minutes. Except one case of postoperative fall, no case of recurrent fractures was observed at a mean follow-up of 8.9 ± 5.1 months. The authors draw a conclusion of the safety and effectiveness of the resorbable Activa IM-NailsTM in the treatment of forearm fractures [18].
Hedelin et al. [19, 20] reported a series of 32 pelvic osteotomies: Salter osteotomy (n = 21) and triple osteotomy (n = 11), fixed with a 4.5 mm (55-70 mm) PLGA polymer screw Activa®. They demonstrated the good stability of pelvic osteotomies after fixation with PLGA screws. In all hips studied, the overall correction was maintained, and there were no complications related to the resorption of the screws. On the MRI performed 2 years after the surgery, there were no significant local reactions. In another paper, the same author reports a series of 21 cases of Salter osteotomy fixed with resorbable screws. Neither perioperative surgical complications nor local reactions occurred [19].
In 2018, Grün presented an excellent paper which describes all resorbable implants used in paediatrics, resorbable, ceramic and metallic, with a specific focus on the magnesium-based (Mg-based) implants [21]. Biodegradable Mg is more tensile, stable, and load bearing, compared to polymers and ceramics. Magnesium also shows favorable biomechanical properties able to support bone fracture healing.
Holweg et al. [22] reported a successful series of 20 fractures of the ankle joint, bi- and trimalleolar fixed with bioabsorbable Mg-based screws. These implants were composed of pure Mg alloyed with calcium and zinc. Blood analysis revealed that Mg and Ca were within a physiologically normal range. No loosening or breakage of screws was observed. Holweg et al. [23, 24] also demonstrated that specific balance between zinc and calcium improved mechanical strength and a reduced in vitro degradation rate. In in vivo experiments with screws, all osteotomies completely consolidated after a maximum of 12 weeks. But screws were resorbed at a mean of 2.5 years after medial malleolus fracture fixation [25]. Marek et al. demonstrated no influence of Mg-Zn-Ca screws on physis and longitudinal bone growth throughout their degradation [26, 27]. Wiktor et al. stated only good and excellent outcomes for humeral capitellum fractures in 6 immature patients aged 10.6-15.3 treated with internal fixation with bioabsorbable nails [28].
CONCLUSION
As the major problem of metallic implants, stainless-steel or titanium, is to remove them or not, the use of resorbable implants, either co-polymers or magnesium-based, solves the problem: removal of implants is not anymore necessary. Year after year, new components are available on the market. These components are becoming safer as they show good solidity allowing bone union of fractures and osteotomies. The implants decompose and are eliminated from the body. Main indications for resorbable implants in paediatrics remain fractures and osteotomies fixed with screws. The development of plates and intramedullary nails will enlarge the indications.
Conflict of interest Authors declare no conflict of interest.
Funding This research received no external funding.
Ethical approval The study was conducted in accordance with the Declaration of Helsinki, and approved by the Local Ethics Committee of the CHRU of Nancy.
Informed consent All patients or their legal representatives provided informed consent.
Список литературы Resorbable implants in paediatric orthopaedics and traumatology
- Barber FA, Dockery WD. Long-term absorption of poly-L-lactic Acid interference screws. Arthroscopy. 2006;22(8):820-826. doi: 10.1016/j. arthro.2006.04.096
- Li RY, Liu ZG, Liu HQ, et al. Evaluation of biocompatibility and toxicity of biodegradable poly (DL-lactic acid) films. Am J Transl Res. 2015;7(8):1357-1370.
- Popkov A, Kononovich N, Dubinenko G, et al. Long Bone Defect Filling with Bioactive Degradable 3D-Implant: Experimental Study. Biomimetics (Basel). 2023;8(2):138. doi: 10.3390/biomimetics8020138
- Popkov AV, Stogov MV, Gorbach EN, et al. Hydrolysis of Bone-Replacing Materials Based on Polylactic Acid and Containing Hydroxyapatite in an In Vitro Experiment. Bull Exp Biol Med. 2022;174(1):99-103. doi: 10.1007/s10517-022-05656-3
- Hedelin H, Larnert P, Antonsson P, et al. Stability in Pelvic Triple Osteotomies in Children Using Resorbable PLGA Screws for Fixation. J Pediatr Orthop. 2021;41(9):e787-e792. doi: 10.1097/BPO.0000000000001873
- Hedelin H, Hebelka H, Brisby H, Laine T. MRI evaluation of resorbable poly lactic-co-glycolic acid (PLGA) screws used in pelvic osteotomies in children-a retrospective case series. J Orthop Surg Res. 2020;15(1):329. doi: 10.1186/s13018-020-01858-5
- Waelti SL, Wildermuth S, Willems EP, et al. Prospective Evaluation of Magnetic Resonance Imaging Features of Magnesium-Based Alloy Screw Resorption in Pediatric Fractures. J Clin Med. 2023;12(8):3016. doi: 10.3390/jcm12083016
- Waelti SL, Fandak J, Markart S, et al. Prospective evaluation of ultrasound features of magnesium-based bioabsorbable screw resorption in pediatric fractures. Eur Radiol. 2023. doi: 10.1007/s00330-023-10091-7
- Heye P, Matissek C, Seidl C, et al. Making Hardware Removal Unnecessary by Using Resorbable Implants for Osteosynthesis in Children. Children (Basel). 2022;9(4):471. doi: 10.3390/children9040471
- Gigante A, Setaro N, Rotini M, et al. Intercondylar eminence fracture treated by resorbable magnesium screws osteosynthesis: A case series. Injury. 2018;49 Suppl 3:S48-S53. doi: 10.1016/j.injury.2018.09.055
- Poircuitte JM, Popkov D, Huber H, et al. Resorbable osteosynthetic devices in pediatric traumatology: a prospective series of 24 cases. Eur J Orthop Surg Traumatol. 2015;25(6):997-1004. doi: 10.1007/s00590-015-1656-8
- Kassai T, Varga M, Jozsa G. Pediatric medial humeral epicondyle fracture in children: Are biodegradable pins with tension band absorbable sutures efficient? Medicine (Baltimore). 2022;101(30):e29817. doi: 10.1097/MD.0000000000029817
- Varga M, Jozsa G, Hanna D, et al. Bioresorbable implants vs. Kirschner-wires in the treatment of severely displaced distal paediatric radius and forearm fractures - a retrospective multicentre study. BMC Musculoskelet Disord. 2022;23(1):362. doi: 10.1186/s12891-022-05305-w
- Sinikumpu JJ, Keränen J, Haltia AM, et al. A new mini-invasive technique in treating pediatric diaphyseal forearm fractures by bioabsorbable elastic stable intramedullary nailing: a preliminary technical report. Scand J Surg. 2013;102(4):258-264. doi: 10.1177/1457496913490459
- Lascombes P, Huber H, Fay R, et al. Flexible intramedullary nailing in children: nail to medullary canal diameters optimal ratio. J Pediatr Orthop. 2013;33(4):403-8. doi: 10.1097/BP0.0b013e318285c54d
- Korobeinikov AA, Popkov DA. Intramedullary elastic stable osteosynthesis in treatment of forearm bone shaft fractures in children. Genij ortiopedii. 2013;(1):14-18. (In Russ.)
- Lascombes P, Journeau P, Popkov DA. Use of flexible nails in children diaphyseal fractures. Five questions and answers. Genij Ortopedii. 2021;27(4):413-417. doi: 10.18019/1028-4427-2021-27-4-413-417
- Roeder C, Alves C, Balslev-Clausen A, et al. Pilot Study and Preliminary Results of Biodegradable Intramedullary Nailing of Forearm Fractures in Children. Children (Basel). 2022;9(5):754. doi: 10.3390/children9050754
- Hedelin H, Larnert P, Hebelka H, et al. Innominate Salter osteotomy using resorbable screws: a retrospective case series and presentation of a new concept for fixation. J Child Orthop. 2019;13(3):310-317. doi: 10.1302/1863-2548.13.180195
- Hedelin H, Brynskog E, Larnert P, et al. Postoperative stability following a triple pelvic osteotomy is affected by implant configuration: a finite element analysis. J Orthop Surg Res. 2022;17(1):275. doi: 10.1186/s13018-022-03169-3
- Grün NG, Holweg PL, Donohue N, et al. Resorbable implants in pediatric fracture treatment. Innov Surg Sci. 2018;3(2):119-125. doi: 10.1515/ iss-2018-0006
- Holweg P, Herber V, Ornig M, et al. A lean bioabsorbable magnesium-zinc-calcium alloy ZX00 used for operative treatment of medial malleolus fractures: early clinical results of a prospective non-randomized first in man study. Bone Joint Res. 2020;9(8):477-483. doi: 10.1302/2046-3758.98. BJR-2020-0017.R2
- Holweg P, Berger L, Cihova M, et al. A lean magnesium-zinc-calcium alloy ZX00 used for bone fracture stabilization in a large growing-animal model. Acta Biomater. 2020;113:646-659. doi: 10.1016/j.actbio.2020.06.013
- Holweg P, Labmayr V, Schwarze U, et al. Osteotomy after medial malleolus fracture fixed with magnesium screws ZX00 - A case report. Trauma Case Rep. 2022;42:100706. doi: 10.1016/j.tcr.2022.100706
- Labmayr V, Suljevic O, Sommer NG, et al. Mg-Zn-Ca Alloy (ZX00) Screws Are Resorbed at a Mean of 2.5 Years After Medial Malleolar Fracture Fixation: Follow-up of a First-in-humans Application and Insights From a Sheep Model. Clin Orthop Relat Res. 2023. doi: 10.1097/ CORR.0000000000002799
- Marek R, Cwieka H, Donohue N, et al. Degradation behavior and osseointegration of Mg-Zn-Ca screws in different bone regions of growing sheep: a pilot study. Regen Biomater. 2022;10:rbac077. doi: 10.1093/rb/rbac077
- Marek R, Eichler J, Schwarze UY, et al. Long-term in vivo degradation of Mg-Zn-Ca elastic stable intramedullary nails and their influence on the physis of juvenile sheep. Biomater Adv. 2023;150:213417. doi: 10.1016/j.bioadv.2023.213417
- Wiktor L, Tomaszewski R. Humeral Capitellum Fractures in Adolescents: A Study of 6 Cases Treated by Open Reduction and Internal Fixation with Bioabsorbable Nails. Adv Orthop. 2022;2022:4012125. doi: 10.1155/2022/4012125


