The effect of competition-simulated training on arterial blood gas responses in football players
Автор: Hassoon Alshuwaili, Hasan Sarraa, Hussein Razzaq, Khazaal Ameen, Kudryavtsev M.D.
Журнал: Человек. Спорт. Медицина @hsm-susu
Рубрика: Физиология
Статья в выпуске: 2 т.25, 2025 года.
Бесплатный доступ
Aim: this study aimed to investigate the effects of football match-intensity physical activity on arterial blood gas responses in young football players using the Bangsbo test.
Arterial blood gases (abg), oxygen partial pressure (pao2), saturation (sao2), carbon dioxide partial pressure (pco2), blood bicarbonate concentration ([hco-], baseline blood ph (phb)
Короткий адрес: https://sciup.org/147251208
IDR: 147251208 | УДК: 796.814 | DOI: 10.14529/hsm250209
Текст научной статьи The effect of competition-simulated training on arterial blood gas responses in football players
Hassoon Alshuwaili1, ; Hasan Sarraa1, , Hussein Razzaq1, , Khazaal Ameen1, , M.D. Kudryavtsev2,3,4, , 1 University of Thi-Qar, Nasiriyah city, Iraq
Хассун Алшувайли1, , Хасан Сарраа1, , Хуссейн Раззак1, , Хазаал Амин1, , М.Д. Кудрявцев2,3,4, , 1 Университет Ти-Кар, Эн-Насирия, Ирак
Introduction. Football is a team sport in which players rely on multiple energy production systems. It is a blend of the three energy systems: the ATP-PC system, the lactic acid system, and the aerobic energy system. The aerobic energy system plays the most significant role in football, accounting for approximately 80% of the total energy production during an official match [3, 4]. Therefore, testing the mechanisms of blood gas transfer from the lungs to the working muscles during exercise is crucial to identify the primary functional barriers that hinder metabolic processes during physical exertion lasting more than 90 minutes. Oxygen transport from atmospheric air to skeletal muscle mitochondria involves six key steps:
-
• The introduction of oxygen into the lungs via alveolar ventilation.
-
• The transfer of oxygen across the alveolar-capillary membrane through diffusion.
-
• The binding of oxygen to hemoglobin.
-
• The delivery of oxygen to capillaries at the level of arterial blood and tissues.
-
• The transfer of oxygen to the mitochondria through diffusion at the capillary level.
-
• The use of oxygen in oxidative phosphorylation to produce ATP [23].
Studying the impact of these six steps on a football player subjected to aerobic physical exertion is of paramount importance for evaluating suitable training pathways.
When PO2 and pH decrease and temperature rises, hemoglobin releases oxygen. Each of these conditions may indicate an increased need for oxygen by the working muscles. These conditions enhance the metabolic release of oxygen in active tissues. Hemoglobin is usually saturated with about 98% oxygen. This is a much higher oxygen capacity than our bodies typically require, so the blood’s oxygen-carrying capacity rarely limits the performance of healthy individuals [9].
One study notes that as PCO 2 in the blood increases on the hemoglobin-oxygen dissociation curve, the rate of hemoglobin-bound oxygen gradually rises. This is known as the hemoglobin saturation percentage. Given that arterial blood PO 2 is around 95 mm Hg, the dissociation curve indicates that arterial blood oxygen saturation is generally 97 %. On the other hand, venous blood PO 2 from tissues is about 40 mm Hg, with hemoglobin saturation around 75 % [11].
The acquired knowledge about the peculiarities of the motor qualities, functional indicators and technical readiness manifestation from the level of speed abilities should be used in the educational and training process of young football players. It will allow for more effective training of football players, which will prevent the athletes’ retraining, which requires a lot of effort and cost [17].
The physical effort exerted by the runner with high intensity causes the accumulation of lactic acid quantities in the blood, as the rate of its accumulation reached (90%) at the end of the tests. The researcher also noted significant differences between the percentage of lactic acid accumulation at the end of the first test (8.1 mmol/L) and the end of the second test (9.9 mmol/L) [3].
Cyclic exercises cause the development of respiratory muscles and increase the vital capacity of the lungs, which improves the motor quality and endurance of the body to physical activity [10].
Aim: to study the effect of physical activity, similar to a football match, on the reaction of arterial blood gases in young football players using the Bangsbo test.
Materials and methods. The research sample comprised players from the College of Physical Education and Sport Sciences team at Thi-Qar University. A total of 12 players were selected from a pool of 24, representing 50% of the total population. This group was chosen based
Table 1 Baseline characteristics of the footbal players in the study sample
Bangsbo Test. The Bangsbo soccer field test circuit. (A) Circuit dimensions. The length and width of the circuit correspond to that of the penalty area of a soccer pitch. The recovery zone is delimited by four small cones at the corners and wooden battens on the field. Cones 15 and 39 correspond to running direction changes, and cones 21 and 33 to the beginning and end of the slalom. They should be of different color to be easily identified. The four cones at the area corners (0, 12, 18, and 36) and the slalom cones (21–33) must be at least 1.2 m high. The others can be small cones. (B) The test lasts 16.5 minutes, during which players alternate between 40 15-second bouts of high-intensity exercise and 10-second low-intensity exercise jogs. During the high-intensity periods, subjects follow the 160 m circuit, running 40 m forward, 8.25 m backwards, 95.25 m forward and through a 120° angle sla-
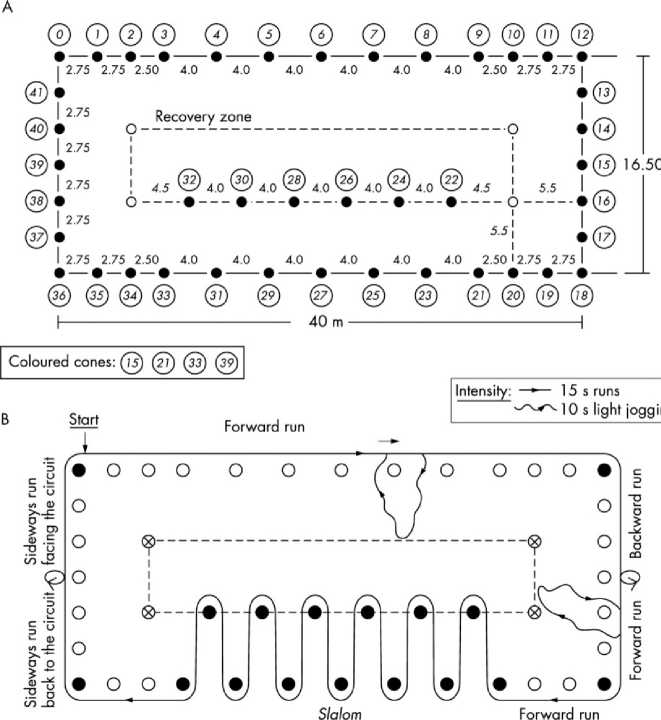
Fig. 1. The BANGSBO test protocol lom, 8.25 m sideways while facing away from the center of the circuit, and 8.25 m sideways while facing the center of the circuit. During the low-intensity periods, players jog to the center of the circuit and back to the last cone-marked position they reached at the end of the previous high-intensity period. If the sound signal stops them during the slalom, the low jogging is performed towards the next slalom cone and back to the last cone they reached before the signal.
Results. The test performance is the distance covered during the 40 periods of high-intensity running (Fig. 1) [4].
Blood Samples. Blood samples were collected both before running (at rest) and immediately after completing the Bangsbo test by the medical staff for all participants. The medical specialist palpated the pulse at the wrist, selecting a prominent pulse site. After sterilizing a small area, the specialist slowly inserted the syringe into the artery. Once the needle was in the artery, arterial blood appeared in the syringe chamber. The specialist then extracted 3 milliliters of arterial blood, as per health guidelines, before withdrawing the needle and sterilizing the area. The player was instructed to apply direct and firm pressure to the puncture site to prevent bleeding. The blood was then transferred from the syringe into special test tubes containing heparin, labeled with the player's name, and placed in a cooling container (Coleman). The blood samples were promptly sent to the laboratory for analysis.
Statistical Analysis. After data collection, statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 27. The primary statistical method employed was the paired samples t-test (Table 2).
Table 2
Arterial blood gas parameters pre- and post-exercise
|
After test |
Before test |
Parameter |
|
85.10 ± 1.01 |
91.22 ± 0.71 |
PaO 2 , mmHg |
|
92.64 ± 1.02 |
97.98 ± 0.93 |
SpO 2 , % |
|
32.88 ± 1.04 |
40.10 ± 1.07 |
PaCO 2 , mmHg |
|
20.10 ± 1.74 |
25.33 ± 1.73 |
HCO 3 ⁻, mmol/L |
|
8.25 ± 1.19 |
1.27 ± 0.23 |
Lactate, mmol/L |
|
7.202 ± 0.04 |
7.403 ± 0.2 |
pH |
Discussion. Partial Pressure of Oxygen (PaO2). Increased oxygen demand during high-intensity exercise from muscle fibers is a primary reason for decreased PaO2. One discovered mechanism is the reduction in the affinity between oxygen and hemoglobin (Hb-O2) under increased tissue oxygen demand. This reduction is more pronounced as red blood cells pass through tissues with high O2 demand. However, once the blood returns to the lungs, the affinity between oxygen and hemoglobin reverts to its baseline level. Thus, changes in the oxygen-hemoglobin bond are localized and not systemic [19].
The rate of gas exchange in pulmonary alveoli and the speed of blood flow through capillaries contribute to decreased time for oxygen diffusion from alveoli to blood. Experimental studies agree that reduced PaO 2 during high-intensity exercise compared to rest is due to decreased transit time of blood through the alveoli [14, 25, 30, 31].
Inadequate time for oxygen diffusion within the lungs was confirmed by Dempsey [7], who found that oxygen diffusion limitations arise during high-intensity exercise due to insufficient time for oxygen equilibration across the bloodgas barrier.
A decrease in PaO 2 is also attributed to the increased oxygen demand by muscle tissues during exercise. Studies suggest that during exercise, the increased demand for oxygen is met by enhancing blood flow to muscles, which improves O 2 unloading from Hb by reducing Hb-O 2 affinity [18].
Another factor influencing decreased PaO 2 is the elevated body temperature during intense exertion, which significantly affects PaO 2 by increasing the dissociation of oxygen from hemoglobin. Increased body temperature during exercise enhances Hb-O 2 dissociation in arterial blood and muscle capillaries, resulting in a greater release of O 2 from Hb to the muscles compared to rest. The temperature in the lungs remains lower than in the working muscles, which promotes normal hemoglobin oxygen loading. However, normal Hb-O 2 affinity values are not fully restored during intense exercise [19].
Oxygen Saturation (SpO 2 ). Reduced arterial oxygen saturation is attributed to rapid breathing and insufficient time for gas exchange, as well as the decreased affinity between oxygen and hemoglobin due to muscle tissue oxygen demands during exertion. This aligns with findings by Mairbäurl [20], who noted that decreased Hb-O 2 affinity weakens arterial O 2 loading, reducing arterial oxygen saturation from 97.5% at rest to 95% during high-intensity exercise.
Decreased PaO2 negatively impacts SpO2 due to lower oxygen balance in the blood, as con- firmed by Dempsey [8]. Arterial hypoxemia during exercise results from decreased PaO2, and the extent of reduction depends on the exercise load. The decline in blood oxygen saturation is linked to insufficient exchange time due to rapid blood flow through capillaries and gas transfer in alveoli, consistent with studies indicating that capillary transit time for O2 can drop below 0.33 seconds, leading to reduced PaO2 [13].
Partial Pressure of Carbon Dioxide (PCO 2 ). The decrease in PCO 2 post-exercise is due to several factors, including the respiratory system’s compensation via hyperventilation to restore acid-base balance (pH) after increased acidity. This was noted by Hopkins [14], who reported that PCO 2 significantly drops following high-intensity exercise due to hydrogen ion accumulation reducing pH, which triggers hyperventilation to compensate. Metabolic acidosis from exercise results in reduced CO 2 levels during and after exercise [12].
Some studies attribute the drop in PCO 2 to inadequate tissue oxygenation during high-intensity effort, which negatively impacts PaCO 2 . This aligns with Dempsey, who observed that during submaximal exercise, increased respiration may be insufficient, and when athletes reach maximal VO 2 levels, PCO 2 typically ranges between 35 and 38 mmHg, leading to hyperventilation.
The researcher suggests that limitations in gas exchange due to insufficient time for adequate ventilation, similar to those observed with O 2 , may also impact the diffusion of carbon dioxide during exercise. “Laboratory-based calculations indicate minor constraints on carbon dioxide diffusion at rest, resulting in an arterial-alveolar PaCO 2 gradient of approximately 0.2 mmHg at rest, increasing to 7 mmHg at peak exercise” [27, 28].
The researcher attributes the reduction in PaCO 2 to impaired carbon dioxide-oxygen balance. “Oxygen exchange may be compromised by a slight delay in the rise of PaO 2 due to concurrent carbon dioxide exchange across the alveolar-capillary membrane” [30]. This can be elucidated by the leftward shift of the hemo-globin-oxygen dissociation curve, with a decrease in PaCO 2 facilitating increased O 2 uptake by hemoglobin.
The accelerated blood flow during high-intensity efforts and inadequate time for complete transit through all ventilation regions contribute to this phenomenon. The “pulmonary shunt theory” posited by Riley (2013) highlights that during high-intensity exercise, blood flows from the venous to the arterial system without traversing all pulmonary ventilation areas, unlike at rest [24]. “These shunts lower the oxygen concentration in blood exiting the left ventricle and circulating to the body. Additionally, poorly ventilated lung units progressively reduce O2 and CO2 tensions in arterial blood” [29]. The functional advantage of pulmonary shunts is to maximize the utilization of residual oxygen in venous blood and reduce the burden on alveoli during high physical exertion. For instance, assuming end-capillary O2 content of 20.4 mL O2/100 mL, with peak cardiac output of 25 L/min and mixed venous O2 content of 5 mL O2/100 mL, a 3% pulmonary shunt effect on O2 content during exercise is significantly beneficial [16].
Bicarbonate ( HCO3 – ):
The reduction in bicarbonate levels stems from its role as a buffering agent that maintains blood pH within normal ranges, preventing deviations toward either high acidity or alkalinity. “Bicarbonate is released into the blood to counteract exercise-induced acidity, thereby supporting energy production. Wasserman [32] notes that energy supply through glycolytic pathways under high-performance conditions leads to further decreases in blood pH, with exercise-induced acidosis becoming a limiting factor for sustained energy production. Protons (hydrogen ions) generated in working muscles are subsequently released into the bloodstream and primarily buffered by bicarbonate ( HCO3– ). Thus, bicarbonate levels during exercise reflect the acid-base balance during intense physical activity” [5].
Oxygen Deficiency and Carbon Dioxide:
Oxygen deficiency leads to increased CO 2 , an acidic gas that reacts with water to form carbonic acid (H 2 CO 3 ). The dissociation of carbonic acid yields elevated concentrations of hydrogen ions (H+) and bicarbonate ( HCO3– ), as detailed by Conhaim [6].
Carbonic Acid Formation Equation: H 2 CO 3 # H 2 O + CO 2
Acid Dissociation Equations: Weak Acid Dissociation:
H+ + HCO- # H 2 CO 3
Stronger Acid Dissociation:
H+ + CO32- # HCO—
Lactate:
Extended high-intensity exercise, as observed in the Bangsbo test, activates anaerobic energy production mechanisms through glycogen metabolism, resulting in increased lactate production. “High-intensity exertion leads to lactate formation due to energy substrate utilization and decreased oxygen availability in the athlete's body” [21].
Muscle Oxygenation:
Inadequate muscle oxygenation during high-intensity efforts represents a primary cause of elevated lactate levels. “Lactic acid accumulates early during submaximal exercise and during oxygen deficit periods due to slowed energy processes and insufficient oxygen delivery to active muscles. Consequently, muscles metabolize glycogen without adequate oxygen, leading to increased lactate production” [1].
Acid-Base Balance (pH):
Post-exercise decreases in pH values are attributed to elevated blood lactate levels. According to Al-Jabali, “Increased lactic acid contri- butes to blood pH reduction, resulting in higher acidity. This impairs actin-myosin cross-bridging essential for muscle contraction and affects energy enzyme activity and neural signaling to muscle fibers” [23].
Research Consensus:
Numerous studies corroborate the negative impact of pH reduction from lactate and hydrogen ion accumulation. Michael K. Stickland [26] confirms that “decreased pH during exercise correlates with increased lactic acid, leading to elevated [H+] concentrations attributed to heightened PCO 2 production in muscle tissue” [22].
Conclusion. The physical exertion involved in the Bangsbo test leads to decreased arterial blood gases and increased lactate levels, negatively impacting muscle oxygenation. This highlights the importance of incorporating aerobic endurance training for football players to enhance their ability to manage these physiological stresses.