The phenomenon of glycated hemoglobin in patients with a new coronavirus infection (COVID-19) with type 2 diabetes mellitus
Автор: Sklyarov Bogdan А., Samoilova Alena D., Pavlov Bogdan V., Levina Anastasia V., Sinelnikova Irina S., Vardanyan Susanna М., Papin Viktor А.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 26, 2023 года.
Бесплатный доступ
During the pandemic of coronavirus infection, medical staff around the world has faced the problem of a significant deterioration in the health conditions of patients, who have a history of type 2 diabetes mellitus and who have infected with COVID-19.The problem of the combination of the coronavirus infection and diabetes mellitus is urgent and requires an indepth study in this context. This article presents and reviews some results of an experiment during which the clinical indicators of 15 patients with type 2 diabetes mellitus, with elevated glycated hemoglobin, infected with coronavirus infection, aged 45 to 65, were taken on the 14th day of observation.
Glycated hemoglobin, type 2 diabetes mellitus, coronavirus infection, blood glucose level, phenomenon
Короткий адрес: https://sciup.org/148326599
IDR: 148326599 | DOI: 10.18137/cardiometry.2023.26.139143
Текст научной статьи The phenomenon of glycated hemoglobin in patients with a new coronavirus infection (COVID-19) with type 2 diabetes mellitus
Bogdan А. Sklyarov, Alena D. Samoilova, Bogdan V. Pavlov, Anastasia V. Levina, Irina S. Sinelnikova, Susanna М. Vardanyan, Viktor А. Papin. The phenomenon of glycated hemoglobin in patients with a new coronavirus infection (COVID-19) with type 2 diabetes mellitus. Cardiometry; Issue No. 26; February 2023; p. 139-143; DOI: 10.18137/cardiometry.2023.26.139143; Available from: phenomenon-glycated-hemoglobin
The new coronavirus infection (COVID-19) has many clinical manifestations and also causes severe respiratory distress syndromes that lead to metabolic disorders. An identification of factors, which influence the severity of the patient’s condition, is important. Patients with diabetes account for approximately one third of the confirmed cases of COVID-19 [1]. Glycosylated hemoglobin (hereinafter referred to as HbA1c) gives a better idea on the patient’s glycemic control [2]. HbA1c is a product of non-enzymatic hemoglobin glycation, reflecting an averaged plasma glucose level through the previous 2-3 months [3], and it is at the same time both a marker for diagnostics and a target for treatment [4, 5].
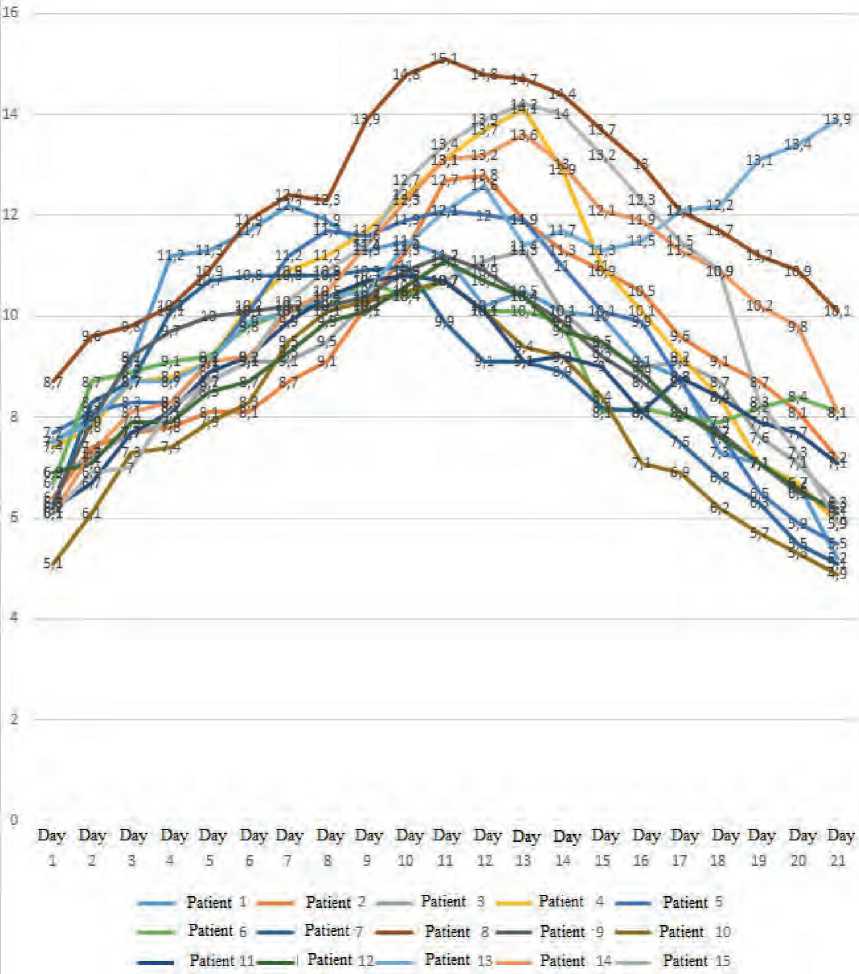
In the course of the study, we took clinical indicators of 15 patients aged 45 to 65 years, who infected with the coronavirus and who suffered from type 2 diabetes mellitus with elevated HbA1c, who were treated at a hospital for the COVID-19patients. All patients have previously given their written consent on medical intervention and processing of their personal data. During the observation and measurement of patients’ parameters, we found that on the 7th day, when oxygen therapy was added, HbA1c began to behave chaotically, after which an increase in the parameter was detected with its maximum recorded to be 15.1%. Further, a phenomenon was recorded, namely from 7 to 12 days, when an increase in the HbA1c value was found to be not typical for the above indicator, since we know that it shows the glucose level as a result from the last 3 months. From day 13, HbA1c dropped sharply, and until day 21, we observed a decrease in the HbA1c value to 5.1%
Further, we have noticed that a sharp drop in the HbA1c value is fatal. If the HbA1c level does not fall below 6.5%, then the outcome is more favorable. The optimal performance for this phenomenon or a favorable outcome is recorded at a glucose level not higher than 12.0 -13.5 mmol / l, while the HbA1c value should not exceed 10.0%, and its sharp drop should not be below 6.5%.
In the infected patients, there was severe intoxication, lack of appetite (diabetes associated with hy-poinsulinemia develops against the background of starvation, which exacerbates and increases glycated hemoglobin), body weight loss, and lack of basal insulin. As a result of observation, 10 patients, who had high levels of blood glucose and HbA1c, died at the hospital, and 5 individuals with more optimal indi- cators were discharged from the hospital with an improvement in their general health state.
Higher levels of HbA1c in the patients with diabetes directly affect the severity of the condition in the COVID-19patients that is a factor responsible for an aggravation of the condition of these patients and that may lead to their death. This phenomenon is explained by the fact that coronavirus infection triggers mechanisms responsible for increasing blood glucose levels, in this case, it retains an excess of glucose in the organism. In addition, hyperglycemia causes structural changes in the lung tissue, including collapse of some parts of the lungs and increased permeability of blood vessels [6]. The main complication of the coronavirus infection in hospitalized patients is pneumonia [7].
Table 1
12^л.
Dav Dav Dav Day Dav Dav Day Day Day Dav Dav Dav Dav Dav Dav Dav Dav Dav Dav Day Day
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21
--Patient 1 — Patient 2 ■
- - Patient 6 — Patient 7 -^—
— Patient 11 Patient 12
Patient 3 -
Patient 8 —
Patient 13^—
Patient 4
Patient 9
Patient 14
— Patient 5
— Patient 10
Patient 15
Figure 1. The phenomenon of glycated hemoglobin in coronavirus infection COVID-19 during oxygen therapy 140 | Cardiometry | Issue 26. February 2023
Список литературы The phenomenon of glycated hemoglobin in patients with a new coronavirus infection (COVID-19) with type 2 diabetes mellitus
- Guan WJ,Ni ZY,Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708-20.
- Yang J, Zheng Y, Gou X, et al.: Prevalence of comorbidities and its effects in patients infected with SARSCoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020, 94:91-5. 10.1016/j.ijid.2020.03.017.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020, 395:1054-62. 10.1016/S0140-6736(20)30566-3.
- Sacks DB, Arnold M, Bakris GL, Bruns DE, Horvath AR, Kirkman MS, Lernmark A, Metzger BE, Nathan DM, National Academy of Clinical Biochemistry. Evidence-Based Laboratory Medicine Committee of the American Association for clinical chemistry guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabetes Care. 2011;6:e61–99.
- American Diabetes Association. Classification and diagnosis of diabetes: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Supplement 1): S15–33.
- American Diabetes Association. Glycemic targets: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Supplement 1):S73–84.
- Means C. (2020). Mechanisms for increasing morbidity and mortality from SARS-CoV-2 infection in people with diabetes: what it means for an effective management strategy. Metabolism108, 154254.
- Khalbaginov AA, et al. Clinical and histological studies of the pathophysiological impact of COVID-19 on the cardiovascular system. International Journal of Medicine and Psychology. 2022;5(4):139-45. [in Russian]
- Voronin IМ, et al. Pathophysiological analysis of the impact of COVID-19 on the morphological characteristics of patients' organisms. International Journal of Medicine and Psychology. 2021;4(6):150-6. [in Russian]
- Misnikova IV, et al Glycated hemoglobin is the main parameter in the control of diabetes mellitus. Diabetes. 2008;4:38-40. [in Russian]
- Belikina DV, et al. COVID-19 in concomitant diabetes mellitus: features of the clinical course, metabolism, inflammatory and coagulation disorders. Modern technologies in medicine. 2020;12(5):6-18. [in Russian]
- Cherkasova YB, et al. The combination of type I diabetes mellitus and diabetes associated with a mutation in the GCK gene. Questions of history. 2022;8-2:280-7. [in Russian]
- Yulia B. Cherkasova, et al. Combination of type I diabetes mellitus and diabetes associated with GCK gene mutation: features of the clinical course in puberty. Cardiometry; Issue 24; November 2022; p.210-216; DOI: 10.18137/cardiometry.2022.24.210216;
- Ilyin AV, et al. Glycated hemoglobin as a key parameter in monitoring patients with diabetes mellitus. Optimal organization of research. Diabetes. 2008;2:60-4. [in Russian]
- Sklyarov BA. Research data and findings related to the omicron strain of coronavirus (COVID-19). International Journal of the Humanities and Natural Sciences. 2022;5-1(68):102-5. [in Russian]
- Biryukova EV. The role of glycated hemoglobin in the diagnosis and improvement of the prognosis of diabetes mellitus. Medical council. 2017;3:48-53. [in Russian]
- Majatsaria АD, et al. Coronavirus infection (COVID-19) and disseminated intravascular coagulation syndrome. Obstetrics, gynecology and reproduction. 2020;14(2):123-31. [in Russian]
- Shestakova MV, et al. Diabetes mellitus in the context of the COVID-19 viral pandemic: features of the course and treatment. Diabetes. 2020;23(2):132-9. [in Russian]
- Shestakova MV, et al. Diabetes mellitus and COVID-19: analysis of clinical outcomes according to the diabetes registry of the Russian Federation. Problems of endocrinology. 2020;66(1):35-46. [in Russian]
- Glybochko PV, et al. Outcomes in patients with severe COVID-19 hospitalized for respiratory support in intensive care units. Clinical pharmacology and therapy. 2020;29(3):25-36. [in Russian]
- Glybochko PV, et al. Clinical characteristics of 1007 patients with severe SARS-CoV-2 pneumonia requiring respiratory support. Clinical pharmacology and therapy. 2020;29(2):21-9. [in Russian]


