Высокомощностная брахитерапия в монорежиме у пациентов с локализованным раком предстательной железы
Автор: Щукина Е.О., Бирюков В.А., Карякин О.Б., Иванов С.А.
Журнал: Экспериментальная и клиническая урология @ecuro
Рубрика: Онкоурология
Статья в выпуске: 3 т.16, 2023 года.
Бесплатный доступ
Введение. Рак предстательной железы (РПЖ) является вторым по распространенности раком среди мужчин. В России число больных РПЖ в I-II стадии увеличилось с 47,7% в 2010г. до 60,7% в 2021г. Одним из основных методов лечения локализованного РПЖ является высокомощностная брахитерапия, которая на сегодняшний день обеспечивает высокую точность охвата дозой предстательной железы, одновременно минимизируя воздействие на рядом расположенные органы. В постоянно растущем объеме литературы высокомощностная брахитерапия рассматривается как метод безопасного и эффективного радикального лечения РПЖ.
Рак предстательной железы, брахитерапия, высокомощностная брахитерапия, сравнение режимов, брахитерапия в монорежиме
Короткий адрес: https://sciup.org/142240010
IDR: 142240010 | DOI: 10.29188/2222-8543-2023-16-3-136-145
Текст обзорной статьи Высокомощностная брахитерапия в монорежиме у пациентов с локализованным раком предстательной железы
Рак предстательной железы (РПЖ) является вторым по распространенности раком среди мужчин.В 2020 году в мире было зарегистрировано 1 414 259 (30,7% от числа всех зарегистрированных) новых случаев рака РПЖ,при этом в Европе РПЖ занял первое место - 473 344 новых случая (20,2% от числа всех зарегистрированных случаев) [1]. В Соединенных штатах Америки РПЖ остается наиболее часто диагностируемым заболеванием среди мужчин, по оценкам исследователей в 2022 г. в США ожидается 268 490 новых случаев РПЖ [2, 3]. В Российской Федерации доля больных РПЖ в I-II стадии увеличилось с 47,7% в 2010 г. до 60,7% в 2021г. [4]. Основными методами лечения локализованного РПЖ являются хирургический (радикальная простатэктомия в различных вариантах исполнения) и лучевой (дистанционная лучевая терапия (ДЛТ) и брахитерапия). В лечении РПЖ применяют 2 основных вида брахитерапии: низкомощностную (НМ-БТ) (используются источники низкой мощности дозы с изотопами I-125, Pd-103, Cs-131 на постоянной основе) и высокомощностную (ВМ-БТ)(осуществляе-мую посредством временного контакта с тканью предстательной железы источников высокой мощности дозы, содержащих изотопы Ir-192, Co-60, Cs-137) [5].
МАТЕРИАЛЫ И МЕТОДЫ
Проведен поиск релеватных публикаций в базах данных PubMed и eLibrary c использованием ключевых слов «брахитерапия», «высокомощностная брахитерапия», «брахитерапия в монорежиме», «brachytherapy», «high-dose-rate brahytherapy», «brachytherapy as mono-therapy». В результате поиска было отобрано 52 источ-ника,которые были включены в литературный обзор.
РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
История развития брахитерапии насчитывает уже более ста лет. Так, вскоре после открытия радия в 1898 г., Pierre Curie предложил французскому врачу-дерматологу Danlos идею лечения злокачественных новообразований кожи непосредственным контактом с ними радиоактивного радия,что и было воплощено в жизнь в 1901 г. Способ лечения состоял в прикладывании к поверхности опухоли элемента радия, заключенного в стеклянную трубку или равномерно распределенного в слое липкого пластыря [6]. Впервые об использовании контактной лучевой терапии РПЖ было сообщено в 1911 году: в то время радий вводили через уретральный катетер [7, 8]. В 1917 году в Нью-Йорке была впервые проведена трансперинеальная имплантация радия [9]. Однако данный подход не одобряли, поскольку счи-талось,что РПЖ является относительно радиорези- стентным раком,и местный контроль не может быть получен без значительных осложнений [10, 11]. Потребовалось более 30 лет, чтобы появились последователи этого метода. В 1952 г. R.H. Floсks разработал технику постановки радиоактивных источников золота в ткань предстательной железы во время открытой операции. Однако большое число осложнений в сочетании с низкой эффективностью вновь отсрочили развитие брахитерапии на несколько десятилетий [12]. В 1970-х годах доктор WF Jr. Whitmore и его коллеги из Мемориального онкологического центра Слоана–Кеттеринга (Memorial Sloan Kettering Cancer Center) начали использовать для лечения РПЖ источники I-125, которые имплантировали во время открытой операции в предстательную железу, одновременно выполняя двустороннюю тазовую лимфаденэктомию [13, 14]. Развитие ультразвуковых технологий в медицинской практике, внедрение трансректального ультразвукового исследования в 1980-х годах для проведения НМ-БТ привели к тому, что к концу 1990-х гг. данный метод стал стандартным и был одобрен для лечения РПЖ низкого риска многочисленными организациями, включая Американское общество брахитера-певтов (ABS) и Американское общество радиационной онкологии (ASTRO) [11]. Однако в конце 1980-х годов анализ постимплантационной дозиметрии показал, что проведенное предварительное планирование было лучше, чем полученное после лечения пациента. Было предположено,что использование изотопа для высокомощностной брахитерапии Ir-192 с более высокой энергией обеспечит доставку дозы на периферическую зону предстательной железы с высокой степенью конформности, обеспечивая хороший охват опухоли и минимизируя дозу на органы риска: мочевой пузырь и прямую кишку [15]. Таким образом, с внедрением трансректального ультразвукового исследования началось активное применение ВМ-БТ в качестве буста к ДЛТ в Швеции, Германии, Японии, Великобритании и США в 1980-х и 1990-х годах [11]. Со временем стал увеличиваться интерес к использованию ВМ-БТ в качестве монотерапии. Так, в нескольких обзорных статьях были представлены результаты, согласно которым ВМ-БТ в монорежиме рассматривалась как новый метод, который может обеспечить высокую конформность дозы и повысить биологически эффективную дозу посредством гипофракционирования [16-19]. В 2000 г. Y. Yoshioka и соавт. впервые сообщили об использовании ВМ-БТ в качестве монотерапии локализованного РПЖ [20]. Полученные отдаленные результаты лечения этой когорты пациентов подтвердили его безопасность и эффективность [16]. За прошедшие десятиле-тия фракционирование при ВМ-БТ изменилось в сторону меньшего количества и более крупных фракций. Благодаря использованию трансректального ультразвукового исследования, планирование имплантации и лечение теперь могут быть завершены менее чем за 2часа,что обеспечивает ранее недостижимую эффективность. Это позволяет ВМ-БТ соперничать по практичности, удобству и стоимости с НМ-БТ [21]. Интерес к ВМ-БТ в лечении РПЖ становится более понятным при изучении его радиобиологии и гипофракционирования.Общая продолжительность традиционного радикального курса ДЛТ в некоторых случаях представляет собой проблему для пациентов, так как обычно такой курс длится 7-9 недель. Существующее традиционное фракционирование появилось на основе доказательств того, что поздние осложнения, вызванные лучевыми повреждениями здоровых тканей, особенно слизистой оболочки прямой кишки, могут быть снижены путем уменьшения дозы за фракцию при одновременном увеличении количества фракций,без влияния на местный контроль [22, 23]. Для того, чтобы описать реакцию нормальных тканей и опухолевой ткани на облучение, было введено понятие величины α/β. Это соотношение представляет собой радиобиологический параметр, объясняющий,как нормальные и опухолевые ткани будут реагировать на разные режимы облучения. В частности, низкое значение α/β характерно для неко- торых медленно пролиферирующих опухолей и некоторых нормальных тканей, преимущественно проявляющих позднюю реакцию на облучение: было продемонстрировано, что в таком случае ткани в основном чувствительны к высоким дозам за фракцию [24]. Несколько клинических исследований показали, что при РПЖ имеет место низкое значение α/β, колеблющееся в пределах 1,5–2 Гр (против 3 Гр для стенки прямой кишки). Таким образом, РПЖ может быть более чувствительным к высоким дозам за фракцию, обычно доставляемым по гипофракционированным схемам [25]. Следовательно, становится обоснованным тот факт, что использование ВМ-БТ с высокими дозами излучения за фракцию может обеспечить лучший контроль над заболеванием. На сегодняшний день ВМ-БТ с использованием объемных изображений (image-guided HDR) обеспечивает высокую точность охвата дозой предстательной железы,одновременно минимизируя воздействие на рядом расположенные органы риска, что позволяет использовать высокомощностную брахитерапию в монорежиме [26]. В постоянно растущем объеме литературы ВМ-БТ рассматривается как метод безопасного и эффективного радикального лечения РПЖ (табл. 1) [27].
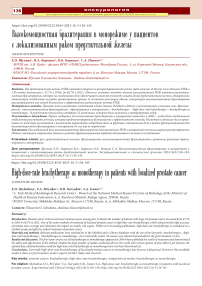
Таблица 1. Онкологические результаты высокомощностной брахитерапии у больных локализованным раком предстательной железы в режиме монотерапии [27]
Table 1. Oncological results of HDR monotherapy for localised prostate cancer [27]
|
Авторы Authors |
Число, n Number, n |
Режим брахитерапии HDR protocol Количество фракций РОД, Гр (процедур (фракция) имплантаций) СОД, Гр Gy Number of Total, Gy (fraction) fractions (implantation procedures) |
Медиана наблюдения, лет Median follow-up, years |
Безрецидивная выживаемость, % Disease-free survival, % |
BED, Гр BED, Gy |
EQD2, Гр EQD2, Gy |
||
|
G. Morton et al. [29] |
170 |
19 13,5 |
1(1) 2 (2) |
19 27 |
6,0 |
73.5% LR/IR5 лет 95% LR/IR 5 лет |
260-270 |
111-116 |
|
I. Strouthos et al. [30] |
450 |
11,5 |
3 (3) |
34,5 |
4,7 |
96% LR, 96% IR, 92% HR 5 лет |
299 |
128 |
|
P. Hoskin et al. [31] |
293 |
19-20 13 10,5 |
1(1) 2 (1) 3 (1) |
19-20 26 31,5 |
4,1 5,3 9,0 |
94% IR/HR4 года 77% IR/HR7 лет 81% IR/HR 7 лет |
251-260 |
108-111 |
|
D.J. Krauss et al. [32] |
58 |
19 |
1 (1) |
19 |
2,9 |
93% LR/IR 3 года |
260 |
111 |
|
Y. Yoshioka et al. [16] |
190 |
6,0 6,0 6,5 |
8 (1) 9(1) 7 (1) |
48 54 45,5 |
7,6 |
93% IR, 81% HR 5 лет |
240-270 |
103-116 |
|
H. Hauswald et al. [33] |
448 |
7,0-7,25 |
8 (1) 9(1) 7 (1) |
42-43,5 |
6,5 |
98.9% LR, 95.2% IR 10 лет |
238-253 |
102-108 |
|
M.S. Jawad et al. [34] |
494 |
9,5 12,0 13,5 |
4(1) 2(1-2) 2(1-2) |
38 24 27 |
4,1 |
98% LR, 95% IR5 лет 92% LR, 81% IR5 лет 100% LR,79% IR 5 лет |
270–279 |
115–119 |
|
P.J. Prada et al. [35] |
60 |
19,0 |
1(1) |
19 |
6,0 |
66% LR, 63% IR 6 лет |
260 |
111 |
|
A. Kukiełka et al.[36] |
77 |
15,0 |
3(3) |
45 |
4,7 |
96,7% все группы риска 5 лет |
495 |
212 |
|
A. Komiya et al. [37] |
51 |
6,5 |
7(1) |
45,5 |
1,4 |
94% все группы риска 17 месяцев |
243 |
104 |
|
P. Hoskin et al.[38] |
197 |
8,5-9,0 10,5 13,0 |
4(1) 3(1) 2(1) |
34-36 31,5 26 |
3,1 |
95% IR, 87% HR 4 года |
227-252 |
97-108 |
|
C.L. Rogers et al. [39] |
284 |
6,5 |
6(2) |
39 |
2,7 |
94% IR 5 лет |
208 |
89 |

|
Авторы Authors |
Число, n Number, n |
Режим брахитерапии HDR protocol Количество фракций РОД, Гр (процедур (фракция) имплантаций) СОД, Гр Gy Number of Total, Gy (fraction) fractions (implantation procedures) |
Медиана наблюдения, лет Median follow-up, years |
Безрецидивная выживаемость, % Disease-free survival, % |
BED, Гр BED, Gy |
EQD2, Гр EQD2, Gy |
||
|
N. Zamboglou et al. [40] |
718 |
9,5 9,5 11,5 |
4(1) 4(2) 3(3) |
38 38 34,5 |
4,4 |
95% LR, 93% IR 93% HR 5 лет |
279-299 |
119-128 |
|
Barkatiet al. [41] |
79 |
10-11,5 |
3 (1) |
30-34,5 |
3,3 |
85.1% LR/IR 5 лет |
230-299 |
99-108 |
|
D.J. Demanes t al. [42] |
298 |
7,0 9,5 |
6 (2) 4 (1) |
42 38 |
5,2 |
97% LR/IR 5 лет |
238-279 |
102-119 |
|
R.J. Mark et al. [43] |
301 |
7,5 |
6 (2) |
45 |
8,0 |
88% все группы риска 8 лет |
270 |
117 |
|
A. Martinez et al. [44] |
248 |
7,0 9,5 |
6 (2) 4 (1) |
42 38 |
4,8 |
87% LR/IR5 лет 91% LR/IR5 лет |
238-279 |
102-119 |
|
P. Ghadjar et al. [45] |
36 |
9,5 |
4 (1) |
38 |
3,0 |
100% LR/IR 3 года |
279 |
119 |
|
I. Grills et al. [46] |
65 |
9,5 |
4 (1) |
38 |
2,9 |
98% LR/IR 3 года |
279 |
119 |
HR – high-risk group- группа высокого риска прогрессирования
IR – intermediate-risk group – группа промежуточного риска прогрессирования
LR – low-risk group – группа низкого риска прогрессирования
EQD2 – равноэффективная доза, вводимая в 2,0 Гр-фракциях с учетом соотношения a/β = 1,5 Гр
BED – биологически эффективная доза с учетом соотношения a/β = 1,5 Гр
РОД – разовая очаговая зона
СОД – суммарная очаговая доза
HR – high-risk group - group of high risk of progression
IR – intermediate-risk group - group of intermediate risk of progression
LR – low-risk group - group of low risk of progression
EQD2 – equally effective dose administered in 2.0 Gy fractions, taking into account the ratio a / β = 1.5 g
BED – biologically effective dose, taking into account the ratio a / β = 1.5 g
ROD – one-time focal zone
SOD – total focal dose
Согласно современным рекомендациям Национальной онкологической сети (NCCN), ВМ-БТ Ir-192 должна проводится в дозах 13,5 Гр за 2 фракции или 9,5 Гр (два раза в день) за 2 фракции [28].
В 2016 г. были представлены результаты одного из крупнейших исследований ВМ-БТ полученные в монорежиме в Калифорнийском университете в Лос-Анджелесе. Авторами были проанализированы результаты лечения 448 пациентов с локализованным РПЖ, получивших лечение с помощью ВМ-БТ с 1996 по 2009 г. Средний возраст составил 64 года (от 42 лет до 90 лет). 288 пациентов относились к группе низкого риска прогрессирования по критериям NCCN (National Comprehensive Cancer Network – национальная единая онкологическая сеть), 160 – к группе промежуточного риска, 42 пациента получали андроген-депривацион-ную терапию (АДТ) до лечения. Лечение состояло из 2процедур имплантации,выполняемых с интервалом в 1 неделю. Доза за фракцию составляла от 7 до 7,25 Гр, суммарная доза составила от 42 до 43,5 Гр. Период наблюдения составил от 3 до 216 месяцев (в среднем 83 месяца). Средний период наблюдения для групп низкого и среднего риска составил 83месяца и 67 месяцев соответственно.Период наблюдения был более длительным для группы низкого риска, поскольку монотерапия ВМ-БТ первоначально предлагалась только пациентам с низким риском. 6-летняя и 10-летняя ПСА-безрецидивная выживаемость составила 98,6% и
97,8% соответственно. 10-летняя общая выживаемость составила 76,7%. Частота генитоуринарной токсичности 3-4 степени, согласно критериям CTCAE (Common Terminology C riteria for Adverse Events – Общие терминологические критерии нежелательных явлений), составила 4,9%. Гастроинтестинальной токсичности 3-4 степени CTCAE за время наблюдения не было выявлено. Таким образом, ВМ-БТ в монорежиме продемострировала хорошие результаты лечения [33]. Представляет собой интерес исследование по изучению эффективности ВМ-БТ группы авторов из Польши под руководством А.M. Kukiełka, проведенное в режиме «экстремального фракционирования» [36]. 77 пациентов получили лечение ВМ-БТ в монорежиме, 45 Гр за 3 фракции по 15 Гр с перерывом между фракциями 21 день. 47 пациентов относились к группе низкого риска прогрессирования NCCN, 27 — промежуточного, 3 — высокого. Следует отметить, что в группе высокого риска прогрессирования пациентам не проводилась ДЛТ и АДТ. Медиана наблюдения в данном исследовании составила 4,7 лет. ПСА-безрецидивная выживаемость на данный период составила 96,7%. Молодой возраст в начале лечения способствовал появлению так называемого феномена «биохимического скачка ПСА» («bounce» – синдрома). У 24,6% пациентов возникли явления острой генитоуринарной токсичности >2 степени. Одному пациенту (1,3%) через 30 месяцев после проведенной брахитерапии была выполнена трансуретральная резекция с целью устранения стеноза уретры 3 степени и острой задержки мочи. У 26 пациентов (33,8%) развились явления поздней генитоуринарной токсичности. Однако авторы указывают на наличие ограничений в своем исследовании, таких как небольшое число выборки и недостаточно продолжительную медиану наблюдения для РПЖ (5 лет в сравнении с предполагаемыми 10-15 лет), что может быть причиной недостаточной оценки явлений поздней токсичности. В 2017 г. опубликованы результаты исследования I Strouthos и соавт. С февраля 2008 года по декабрь 2012 года 450 пациентов с клинически локализованным РПЖ были пролечены с помощью ВМ-БТ в монорежиме. В исследование были включены 198 пациентов группы низкого, 135 промежуточного и 117 высокого риска. Все пациенты получили три фракции по 11,5 Гр до СОД 34,5 Гр с межфракционным интервалом 21 день. 58 пациентов (12,8%) получали АДТ, 32 из которых относились к группе высокого и 26 – среднего риска. Медиана наблюдения составила 56,3 мес. Из 450 пациентов у 22 (4,9%) пациентов возник биохимический рецидив, а у 5 (1,1%) были выявлены отдаленные метастазы. 60-месячная общая выживаемость, ПСА – безрецидивная выживаемость и выживаемость без прогрессирования составили 96,2%, 95,0% и 99,0% соответственно. Таким образом, результаты подтверждали, что ВМ-БТ в монорежиме является безопасным и эффективным методом лечения при локализованном РПЖ [30]. Однако для того, чтобы сделать ВМ-БТ более близкой по конкурентности и переносимости с НМ-БТ, было необходимо доказать эффективность и переносимость однофракционного лечения. Считая отношение α/β для РПЖ равным 1,5 (1,2-3 Гр), можно было бы предсказать, что одна фракция 19 Гр будет иметь аналогичную биологическую эффективность по сравнению с мультифракционными протоколами 13,5 Гр х 2, 11,5 Гр х 3 или 9,5 Гр х 4 [17]. В серии исследований с использованием 19 Гр за одну фракцию были получены обнадеживающие клинические результаты, что, казалось, подтверждает радиобиологические предположения. Результаты лечения с использованием ВМ-БТ в монорежиме в одной фракции были опубликованы в 2012 г. P.J. Prada и соавт. Были проанализированы результаты лечения 40 пациентов. Лечения проводилось в режиме 19 Гр х 1 фракцию с одновременным введением трансперинеально гиалуроновой кислоты в параректальную жировую клетчатку с целью снижения радиационной нагрузки на прямую кишку. Средний возраст пациентов составил 71 год (59-79 лет). Сумма баллов по шкале Глисона составляла 6 баллов у 38 пациентов и 7 баллов у 2пациентов.Инициальный ПСА ≤10 нг/мл отмечен у 32 пациентов, от 10,1 до 20 нг/мл – у 8 пациентов. В исследование было включено 29 пациентов группы низкого риска (72,5%) и 11 (27,5%) па- циентов группы промежуточного риска. ПСА-безре-цидивная выживаемость составила 100% и 88% в группах низкого и промежуточного риска прогрессирования соответственно в течение 32 месяцев. Медиана ПСА после лечения составила 1,2 нг/мл. В исследовании ни у одного пациента не наблюдались явления ранней или генитоуринарной токсичности выше 2 степени. Острая задержка мочи 1 степени, требующая катетеризации мочевого пузыря в течение 7 дней в ближайшем послеоперационном периоде,на-блюдалась у 1 пациента (2,5%). У 89% пациентов была сохранена сексуальная активность. Таким образом, был сделан вывод о хорошей переносимости однофракционного режима высокомощностной брахитерапии [35]. В 2017 г. получены результаты исследования P. Hoskin и соавт., включившего в себя 293 пациента, которые были поделены на четыре группы. Пациентам в первой группе было выполнено лечение в объеме 1 фракции 19 Гр или 1 фракции 20 Гр (A = 49), во второй группе – 2 фракции по 13 Гр (B = 138) и пациентам третьей группы – 3 фракции по 10,5 Гр (C=106) ВМ-БТ в монорежиме. Медиана наблюдения составила 49, 63 и 108 месяцев (A, B и C соответственно). Четырехлетняя ПСА – безрецидивная выживаемость составила 94% в группе А, 93% – в В и 91% – в С (р=0,54). В результате исследования было выявлено, что одна фракция 19-20 Гр позволяет достичь аналогичных показателей ПСА-безрецидивной выживаемости по сравнению с 2-3 фракциями [31]. Также в 2017 г. были опубликованы предварительные результаты проспективного исследования D.J. Krauss и соавт. В исследование было включено 63пациента с РПЖ категории ≤T2a, уровнем ПСА ≤15 нг/мл и суммой баллов по шкале Глисона ≤7. Всем пациентам была выполнена одна фракция в дозе 19 Гр ВМ-БТ. Для анализа были получены данные 58 пациентов. Чуть более 1/3 пациентов (34,5%) были отнесены к промежуточному риску по критериям NCCN, а остальные относились к низкому риску. Сумма баллов по шкале Глисона составила 7 и 6 баллов у 29,3% пациентов и 70,7% соответственно. У 93,1% пациентов значение ПСА было <10 нг/мл на момент постановки диагноза. Медиана наблюдения составила 2,9 года. За это время биохимический рецидив был диагностирован у трех пациентов, в результате чего 3-летняя ПСА-безрецидивная выживаемость составила 93,2%. Таким образом, согласно предварительным результатам данного исследования, был сделан вывод, что ВМ-БТ в объеме одной фракции в дозе 19 Гр хорошо переносится отдельными пациентами. Однако следует отметить, что в этом исследовании был короткий интервал наблюдения, и преобладали пациенты группы низкого риска [32].
В 2019 году опубликованы результаты 5-летнего наблюдения за группой пациентов с низким и средним риском рака предстательной железы, которым выпол- нена ВМ-БТ в объеме 1 фракции 19 Гр. В исследовании наблюдались 68 пациентов,средний возраст составил 62 года (43-73 года), медиана наблюдения 3,93 года (0,33 – 6,13 лет). К группе низкого риска прогрессирования NCCN относились 40 (58,8%) пациентов, промежуточного – 28 (41,2%) пациентов. Поздняя генито-уринарная токсичность 2 степени и выше наблюдалась у 10 пациентов (14,7%), поздняя гастроинтестинальная токсичность – у 4 пациентов (5,9%). Пятилетняя без-рецидивная выживаемость составила 77,2%. В группе низкого риска пятилетняя безрецидивная выживаемость составила 79,0%, а промежуточного – 75,2%. Частота биохимического рецидива через пять лет составила 26,6%, а локального рецидива – 18,8%. Таким образом, полученные данные демонстрируют значительное увеличение частоты рецидивов при использовании однофракционного режима, и, по мнению авторов, дальнейшее применение данного режима оправдано только в рамках клинических исследований.Однако авторы подчеркивают целесообразность продолжения изучения однофракционных режимов брахитерапии в связи с хорошим профилем токсичности [47].
Результаты применения ВМ-БТ в однофракционном режиме также были представлены H . Tharma-lingam и соавт. [48]. Исследование включало в себя 441 пациента, и это одна из самых крупных по числу пациентов когорт. Следует отметить, что в данном исследовании высокомощностная брахитерапия в монорежиме применялась в группах как низкого и промежуточного, так и высокого риска: низкий риск – 44 пациента (10%), промежуточный благоприятный – 186 (42%), промежуточный неблагоприятный – 99 (23%), высокий – 112 (5%) пациентов. ВМ-БТ сопровождалась применением AДТ в течение 6 месяцев в группе промежуточного риска и 24-36 месяцев – в группе высокого риска, за 1-3 месяца до брахитерапии. Медиана наблюдения после лечения составила 26 месяцев (от 2 до 56 месяцев). Двухлетняя выживаемость без прогрессирования составила 94% для всех пациентов и 100%, 96%, 92% и 92% для пациентов групп низкого,промежуточного благоприятного, промежуточного неблагоприятного и высокого риска соответственно. 3-летняя выживае- мость без прогрессирования составила 88% (среди всех пациентов), 100% (низкий риск), 89% (благоприятный промежуточный риск), 81% (неблагоприятный промежуточный риск) и 75% (высокий риск). Острая токсичность выше 2 степени не наблюдалась (табл. 2). Острая задержка мочи, требующая катетеризации, произошла у 16 пациентов (5,4%). У двух пациентов развилась поздняя генитоуринарная токсичность 3 степени, была диагностирована стриктура уретры, выполнено хирургическое иссечение стриктуры. У двух пациентов развилась поздняя гастроинтестинальная токсичность 3 степени, у обоих сформировались свищи прямой кишки, требующие выполнения колостомии. Следует отметить, что один из этих пациентов ранее получал хи-миолучевую терапию по поводу рака прямой кишки.
Одним из ограничений данного исследования является короткий период наблюдения, и, таким образом, отдаленные результаты однофракционного режима остаются не до конца определенными. Результаты этого многоцентрового исследования показали, что монотерапия ВМ-БТ в однократной дозе 19 Гр является безопасным методом лечения пациентов с локализованным РПЖ низкого и благоприятного промежуточного риска, который хорошо переносится и имеет хорошие результаты ПСА-безрецидивной выживаемости. Однако у пациентов групп неблагоприятного промежуточного и высокого риска ВМ-БТ в монорежиме 19 Гр в разовой дозе не является достаточной опцией лечения.
G. Morton и соавт. опубликовали результаты II фазы рандомизируемого клинического исследования (РКИ), в котором сравнивалась эффективность ВМ-БТ в монорежиме 19 Гр х 1 или 13,5 Гр х 2. 170 пациентов были рандомизированы на группы: 19 Гр х 1 фракция – 87 пациентов, 13,5 Гр х 2 фракции – 83 пациента. Медиана наблюдения составила 60 месяцев (от 24 до 76 месяцев). Средний возраст составлял 65 лет (от 46 до 80 лет), а средний инициальный ПСА составил 6 ,33 нг/мл (от 1,12 до 16,01 нг/мл). 33 пациента (19%) относились к группе низкого риска NCCN, 86 (51%) к группе благоприятного промежуточного и 51 (30%) к группе неблагоприятного промежуточного.
Таблица 2. Распространенность острой и поздней токсичности ≤G2 при проведении ВМ-БТ в монорежиме [48]
Table 2. Prevalence of acute and late toxicity ≤G2 during HDR-BT as monotherapy [48]
|
Tоксичность (CTCAE v4.0) |
Распространенность токсичности ≤G2 (%) (месяцы после ВМ-БТ) Prevalence of toxicity ≤G2 (%) (months after HD-BT |
||||
|
Тoxicity (CTCAE v4.0) |
1 месяц 1 month |
3 месяц 3 month |
6 месяц 6 month |
12 месяц 12 month |
24 месяц 24 month |
|
Генитоуринарная токсичность Genitourinary toxicity |
12,0% |
6,8% |
7,4% |
8,8% |
8,5% |
|
Гастроинтестинальная токсичность Gastrointestinal toxicity |
3,0% |
1,0% |
0,7% |
0,0% |
2,6% |
|
Количество пациентов Number of patients |
301 |
295 |
269 |
227 |
153 |
5-летняя безрецидивная выживаемость составила 73,5% группе однофракционного режима и 95% – в группе пациентов, которым брахитерапия была проведена в двух фракциях [29]. В. Johansson и соавт. в июне 2021 г опубликовали результаты ретроспективного исследования с участием 229 больных РПЖ категории T1c-T2b, сумма баллов по шкале Глисона 6 (3 + 3), (ПСА) ≤ 15) или Глисон 7 (3 + 4) (ПСА ≤ 10), получивших лечение в период с 2004 по 2012 г. ВМ-БТ в монорежиме с использованием трех различных схем фракционирования 92-95 Гр (EQD (2), α/β = 3). В группе 4F (n = 19) пациенты получили 4 фракции по 9,5 Гр в течение 2 дней, в группе 3F – 3 фракции по 11 Гр в течение 4 недель, в группе 2F - 2 фракции по 14 Гр за 2 недели. Адъювантная гормональная терапия не проводилась. Медиана наблюдения составила 7,1 лет, биохимический рецидив был обнаружен у 22/229 (9,6%): 2/19 (10,5%) в группе 4F, 5/107 (4,7%) в группе 3F и 15/103 (14,6%) в группе 2F. В течение периода наблюдения умерли 23 из 229 пациентов, и только у четырех пациентов причина смерти была связана с РПЖ. Поздняя генитоуринарная токсичность G3 и G4 составила 3,5% [49].
Также в 2021 г. опубликован мета-анализ, включающий в себя 7 исследований ВМ-БТ в монорежиме с использованием нескольких фракций. Были проанализированы результаты лечения 2123 пациентов (ха- рактеристика пациентов приведена в таблице 3). ПСА-безрецидивная выживаемость на срок наблюдения 5 лет составила 95%. Была обнаружена связь между ПСА-безрецидивной выживаемостью и биологически эффективной дозой,что соответствует ранее опубликованным данным. И хотя стандартной схемы фракционирования для ВМ-БТ в монорежиме не существует, на сегодняшний день есть тенденция к уменьшению общего количества фракций.Несмотря на относительно высокую биологически эффективную дозу, поздняя генитоуринарная токсичность ≥ G3 в группах исследования составляла 2-3%, а гастроинтестинальная – менее 0,5%. Полученные результаты демонстрируют, что применение ВМ-БТ в качестве монотерапии в нескольких фракциях связано с высокими показателями выживаемости и низкими показателями токсичности 3-4 степени. Это доказывает эффективность применения данного метода лечения у пациентов с локализованным раком предстательной железы [50].
Одними из последних в 2022 г. J.-M. Hannoun-Levietal и соавт. представлены результаты еще одного проспективного исследования SiFEPI II фазы. 33 пациента (25 пациента из группы низкого риска и 8 – из благоприятного промежуточного риска прогрессирования). Медиана наблюдения – 72,8 мес. 6-летняя безрецидивная выживаемость составила 54%, опу-
Таблица 3. Характеристика пациентов [50]
Table 3. Information about patients [50]
|
Общее число пациентов Total number of patients |
2123 |
|
|
Число фракций Number of fractions |
5 (в среднем 2,9) |
|
|
Доза за фракцию, Гр Dose per fraction, Gy |
8,8 (от 6 до 13,5) |
|
|
Средний возраст, лет Average age, years |
66 (от 62 до 71) |
|
|
Категория Т Category T |
Т1, n (%) |
1109 (52,2) |
|
Т2, n (%) |
822 (38,7) |
|
|
Т3/Т4, n (%) |
188 (8,9) |
|
|
неизвестно, n (%) unknown, n(%) |
4 (0,2) |
|
|
Среднее значение ПСА (нг/мл)1 Mean PнA value (ng/ml)1 |
7,5 (от 6,3 до 17,4) |
|
|
Сумма баллов по шкале Глисона Gleason score |
≤ 6 n (%) |
1197 (56,4) |
|
7 n (%) |
742 (38,0) |
|
|
≥ 8 n (%) |
120 (5,6) |
|
|
Группа риска прогрессирования согласно критериям NCCN Group at risk of progression according to NCCN criteria |
низкий n(%) low n(%) |
860 (40,5) |
|
промежуточный n(%) intermediate (%) |
843 (39,7) |
|
|
высокий n (%) high n (%) |
420 (19,8) |
|
|
АДТ |
671 (31,6) |
|
|
Средняя продолжительность АДТ < 7 месяцев2, n Average duration of ADT < 7 months2, n |
1503 (в среднем 81,2) |
|
1 сообщается в 7 исследованиях; 2 сообщается в 9 исследованиях
1 reported in 7 studies; 2 reported in 9 studies
холь-специфическая выживаемость составила 100%, общая выживаемость – 89 %. Ранней токсичности выше 2 степени не наблюдалось. Поздняя генитоуринарная, гастроинтестинальная токсичность, эректильная дисфункция наблюдалась у 11, 4 и 7 больных соответственно. Поздней токсичности выше 2 степени не наблюдалось. Биохимический рецидив выявлен у 11 пациентов со средним временным интервалом между лечением и биохимическим рецидивом 51 месяц. Долгосрочные результаты исследования показывают, что одна фракция в 20 Гр приводит к неоптимальному биохимическому контролю, однако демонстрирует удовлетворительный профиль токсичности [51].
ЗАКЛЮЧЕНИЕ
На сегодняшний день ВМ-БТ в монорежиме зарекомендовала себя в качестве эффективного метода лечения пациентов с локализованным РПЖ.Несмотря на большое число проводимых во всем мире исследований с различными вариантами подведения дозы за фракцию, оптимальная доза и режим фракционирования для ВМ-БТ в монорежиме до сих пор не определены. Однофракционный режим с использованием 19 Гр связан с худшими показателями ПСА-безрецидив-ной выживаемости и не рекомендуется вне клинических испытаний. Однако в то же время подведение дозы за 1 фракцию остается привлекательным, являясь более экономичным, менее токсичным и удобным для пациента. Возможно, вскоре мы получим новые данные исследований эффективности и безопасности однофракционной ВМ-БТ с эскалацией дозы и бустирова-нием доминантного очага для того, чтобы вновь вернуться к монорежиму за 1 фракцию.
Список литературы Высокомощностная брахитерапия в монорежиме у пациентов с локализованным раком предстательной железы
- The Global Cancer Observatory. Estimated number of new cases in 2020. Cancer Today 2021. [Electronic resource]. URL: https://gco.iarc.fr/today/online-analysis-table?v=2020&mode=cancer&mode_population=continents&population=900&populations=900&key=asr&sex=0&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5 D=17&group_cancer=1&include_nmsc=0&include_nmsc_other=1.
- Nguyen AT, Liu CS, Kamrava M. A «scoping» review of prostate brachytherapy and immune responses. Brachytherapy 2023;22(1):21–9. https://doi.org/10.1016/j.brachy.2022.10.009.
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin 2022;72(1):7–33. https://doi.org/10.3322/caac.21708.
- Каприн А.Д., Старинский В.В, Шахзадова А.О. Состояние онкологической помощи населению России в 2021 году. М., 2022; 239 с. [Kaprin A.D., Starinsky V.V., Shakhzadovа A.O. The state of oncological care for the population of Russia in 2021. M., 2022; 239 p. (In Russian)].
- Каприн А.Д., Бирюков В.А., Черниченко А.В. и др. Брахитерапия рака предстательной железы. Опыт работы филиалов Национального медицинского исследовательского центра радиологии. Онкоурология 2018;14(1):94–9. [Kaprin A.D., Biryukov V.A., Chernichenko A.V. et al. Prostate cancer brachytherapy. Experience of the branches of the National Medical Research Center of Radiology. Onkourologiya = Cancer Urology 2018;14(1):94–9. (In Russian)]. https://doi.org/10.17650/1726-9776-2018-14-1-94-99.
- А.С. Павлов. Внутритканевая гамма- и бетатерапия злокачественных опухолей. М.: Медицина 1967; 283 с. [A.S. Pavlov. Interstitial gamma and beta therapy of malignant tumors. M.: Medicine 1967; 283 p. (In Russian)].
- Garzotto M, Fair WR. Historical perspective on prostate brachytherapy. J Endourol 2000;14(4):315-8. https://doi.org/10.1089/end.2000.14.315.
- Lederman M. The early history of radiotherapy: 1895–1939. Int J Radiat Oncol Biol Phys 1981;7(5):639-48. https://doi.org/10.1016/0360-3016(81)90379-5.
- Young HH. The use of radium and the punch operation in desperate cases of enlarged prostate. Ann Surg 1917;65(5):633-41.
- Deming CL. Results in one hundred cases of cancer of prostate and seminal vesicles treated with radium. Surg Gynecol Obstet 1922;34:99-118.
- Zaorsky NG, Davis BJ, Nguyen PL, Showalter TN, Hoskin PJ, Yoshioka Y, et al. The evolution of brachytherapy for prostate cancer. Nat Rev Urol 2017;14(7):415-39. https://doi.org/10.1038/nrurol.2017.76.
- Flocks RH, Kerr HD, Elkins HB, Culp D. Treatment of carcinoma of the prostate by interstitial radiation with radio-active gold (Au 198): a preliminary report. J Urol 1952;68(2):510-22. https://doi.org/10.1016/S0022-5347(17)68230-2.
- Whitmore WF Jr, Hilaris B, Grabstald H. Retropubic implantation to iodine 125 in the treatment prostatic cancer. J Urol 1972;108(6):918–20. https://doi.org/10.1016/s0022-5347(17)60906-6.
- Hilaris BS, Whitmore WF Jr., Batata MA, Grabstald H. Radiation therapy and pelvic node dissection in the management of cancer of the prostate. Am J Roentgenol Radium Ther Nucl Med 1974;121(4):832–8. https://doi.org/10.2214/ajr.121.4.832.
- Mate TP, Gottesman JE, Hatton J, Gribble M, Van Hollebeke L. High dose-rate afterloading 192 Iridium prostate brachytherapy: feasibility report. Int J Radiat Oncol Biol Phys 1998;41(3):525–33. https://doi.org/10.1016/ s0360-3016(98)00097-2.
- Yoshioka Y, Suzuki O, Isohashi F, Seo Y, Okubo H, Yamaguchi H, et al. High-dose-rate brachytherapy as monotherapy for intermediate- and high-risk prostate cancer: clinical results for a median 8-year follow-up. Int J Radiat Oncol Biol Phys 2016;94(4):675–82. https://doi.org/10.1016/j.ijrobp.2015.05.044.
- Yoshioka Y, Yoshida K, Yamazaki H, Nonomura N, Ogawa K. The emerging role of high dose-rate (HDR) brachytherapy as monotherapy for prostate cancer. J Radiat Res 2013;54(5):781-8. https://doi.org/10.1093/jrr/rrt027.
- Yoshioka Y, Suzuki O, Otani Y, Yoshida K, Nose T, Ogawa K. High-dose-rate brachytherapy as monotherapy for prostate cancer: Technique, rationale and perspective. J Contemp Brachytherapy 2014;6(1):91-8. https://doi.org/10.5114/ jcb.2014.42026.
- Demanes DJ, Ghilezan MI. High-dose-rate brachytherapy as monotherapy for prostate cancer. Brachytherapy 2014;13(6):529-41. https://doi.org/10.1016/ j.brachy.2014.03.002.
- Yoshioka Y, Nose T, Yoshida K, Inoue T, Yamazaki H, Tanaka E, et al. High-dose-rate interstitial brachytherapy as a monotherapy for localized prostate cancer: Treatment description and preliminary results of a phase I/II clinical trial. Int J Radiat Oncol Biol Phys 2000;48(3):675-81. https://doi.org/10.1016/ s0360-3016(00)00687-8.
- Crook J, Marbán M, Batchelar D. HDR Prostate Brachytherapy. Sem Radiat Oncol 2020;30(1):49–60. https://doi.org/10.1016/j.semradonc.2019.08.00310.1016/ j.semradonc.2019.08.003.
- Joiner MC, Kogel A, van der. Basic clinical radiobiology. 4th ed. CRC Press 2009; 392 p.
- De Bari B, Daidone A, Alongi F. Is high dose rate brachytherapy reliable and effective treatment for prostate cancer patients? A review of the literature. Crit Rev Oncol Hematol 2015;94(3):360-70. http://doi.org/10.1016/ j.critrevonc.2015.02.003.
- Cosset J-M, Mornex F, Eschwège F. Hypofractionnement en radiothérapie: l’éternel retour. Cancer Radiother 2013;17(5–6):355–62. https://doi.org/10.1016/ j.canrad.2013.06.027.
- Brenner DJ, Martinez AA, Edmundson GK, Mitchell C, Thames HD, Armour EP. Direct evidence that prostate tumors show high sensitivity to fractionation [low α/β value], similar to late-responding normal tissue. Int J Radiat Oncol Biol Phys 2002;52(1):6–13. https://doi.org/10.1016/S0360-3016(01)02664-5.
- Переход от 2D брахитерапии к 3D брахитерапии с высокой мощностью дозы. Доклады МАГАТЭ по здоровью человека 2021;(12):1-54. [Электронный ресурс]. [Transition from 2D brachytherapy to 3D high dose rate brachytherapy. Doklady MAGATE po zdorov'yu cheloveka = IAEA Human Health Reports 2021;(12):1-54. [Electronic resource]. (In Russian)]. URL: https://www-pub.iaea.org/MTCD/Publications/PDF/P1681R_HHR12_web.pdf.
- Strouthos I, Karagiannis E, Zamboglou N, Ferentinos K. High-dose-rate brachytherapy forprostate cancer: Rationale, current applications, and clinicaloutcome. Cancer Rep 2022;5(1):e1450. https://doi.org/10.1002/cnr2.1450.
- NCCN Guidelines Version 1. 2023 Prostate Cancer. [Electronic resource]. URL: https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf.
- Morton G, McGuffin M, Chung HT, Tseng C-L, Helou J, Ravi A, et al. Prostate high dose-rate brachytherapy as monotherapy for low and intermediate risk prostate cancer: Efficacy results from a randomized phase II clinical trial of one fraction of 19 Gy or two fractions of 13.5 Gy. Radiother Oncol 2020;146:90–6. https://doi.org/10.1016/j.radonc.2020.02.009.
- Strouthos I, Tselis N, Chatzikonstantinou G, Butt S, Baltas D, Bon D, et al. High dose rate brachytherapy as monotherapy for localised prostate cancer. Radiother Oncol 2018;126(2):270-77. https://doi.org/10.1016/j.radonc.2017.09.038.
- Hoskin P, Rojas A, Ostler P, Hughes R, Alonzi R, Lowe G. Single-dose high-dose-rate brachytherapy compared to two and three fractions for locally advanced prostate cancer. Radiother Oncol 2017;124(1):56-60. http://doi.org/10.1016/j.radonc.2017.06.014.
- Krauss DJ, Ye H, Martinez AA, Mitchell B, Sebastian E, Limbacher A, et al. Favorable Preliminary outcomes for men with low- and intermediate-risk prostate cancer treated with 19 Gy single fraction high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys 2017;97(1):98-106. http://doi.org/10.1016/ j.ijrobp.2016.08.011.
- Hauswald H, Kamrava MR, Fallon JM, Wang PC, Park SJ, Van T, et al. High-dose-rate monotherapy for localized prostate cancer: 10-year results. Int J Radiat Oncol Biol Phys 2016;94(4),667–74. http://doi.org/10.1016/j.ijrobp.2015.07.2290.
- Jawad MS, Dilworth JT, Gustafson GS, Ye H, Wallace M, Martinez A, Chen PY, et al. Outcomes associated with 3 treatment schedules of high-dose-rate brachytherapy monotherapy for favorable-risk prostate cancer. Int J Radiat Oncol Biol Phys 2016;94(4),657-66. http://doi.org/10.1016/j.ijrobp.2015.10.011.
- Prada PJ, Jimenez I, Gonzalez-Suarez H, Fernandez J, Cuervo-Arango C, Mendez L. High-dose-rate interstitial brachytherapy as monotherapy in one fraction and transperineal hyaluronic acid injection into the perirectal fat for the treatment of favorable stage prostate cancer: treatment description and preliminary results. Brachytherapy 2012;11(2):105–10. doi:10.1016/j.brachy.2011.05.003.
- Kukiełka AM, Dąbrowski T, Walasek T, Olchawa A, Kudzia R, Dybek D. High-dose-rate brachytherapy as a monotherapy for prostate cancer. Single-institution results of the extreme fractionation regimen. Brachytherapy 2015;14(3):359-65. https://doi.org/10.1016/j.brachy.2015.01.004.
- Komiya A, Fujiuchi Y, Ito T, Morii A, Yasuda K, Watanabe A, et al. Early quality of life outcomes in patients with prostate cancer managed by high-dose-rate brachytherapy as monotherapy. Int J Urol 2013;20(2):185-92. https://doi.org/10.1111/j.1442-2042.2012.03125.x.
- Hoskin P, Rojas A, Lowe G, Bryant L, Ostler P, Hughes R, et al. High-dose-rate brachytherapy alone for localized prostate cancer in patients at moderate or high risk of biochemical recurrence. Int J Radiat Oncol Biol Phys 2012;82(4):1376-84. https://doi.org/10.1016/j.ijrobp.2011.04.031.
- Rogers CL, Alder SC, Rogers RL, Hopkins SA, Platt ML, Childs LC, et al. High dose brachytherapy as monotherapy for intermediate risk prostate cancer. J Urol 2012;187(1):109-16. https://doi.org/10.1016/j.juro.2011.09.050.
- Zamboglou N, Tselis N, Baltas D, Buhleier T, Martin T, Milickovic N, et al. High-dose-rate interstitial brachytherapy as monotherapy for clinically localized prostate cancer: treatment evolution and mature results. Int J Radiat Oncol Biol Phys 2013;85(3):672-8. https://doi.org/10.1016/j.ijrobp.2012.07.004.
- Barkati M, Williams SG, Foroudi F, Tai KH, Chander S, van Dyk S, et al. High-dose-rate brachytherapy as a monotherapy for favorable-risk prostate cancer: a Phase II trial. Int J Radiat Oncol Biol Phys 2012;82:1889–96. https://doi.org/10.1016/j.ijrobp.2010.09.006.
- Demanes DJ, Martinez AA, Ghilezan M, Hill DR, Schour L, Brandt D, et al. High‐dose‐rate monotherapy: safe and effective brachytherapy for patients with localized prostate cancer. Int J Radiat Oncol Biol Phys 2011;81(5):1286-92. https://doi.org/10.1016/j.ijrobp.2010.10.015.
- Mark RJ, Anderson PJ, Akins RS, Nair M. Interstitial high‐dose‐rate brachytherapy as monotherapy for early stage prostate cancer: median 8‐year results in 301 patients. Brachytherapy 2010;9:S76. https://doi.org/10.1016/ j.brachy.2010.02.127
- Martinez AA, Demanes J, Vargas C, Schour L, Ghilezan M, Gustafson GS. High‐dose‐rate prostate brachytherapy: an excellent accelerated‐hypofractionated treatment for favorable prostate cancer. Am J Clin Oncol 2010;33(5):481-8. https://doi.org/10.1097/COC.0b013e3181b9cd2f
- Ghadjar P, Oesch SL, Rentsch CA, Isaak B, Cihoric N, Manser P, et al. Late toxicity and five year outcomes after high‐dose‐rate brachytherapy as a monotherapy for localized prostate cancer. Radiat Oncol 2014;9:122. https://doi.org/10.1186/1748-717X-9-122
- Grills IS, Martinez AA, Hollander M, Huang R, Goldman K, Chen PY, et al. High dose rate brachytherapy as prostate cancer monotherapy reduces toxicity compared to low dose rate palladium seeds. J Urol 2004;171(3):1098‐104. https://doi.org/10.1097/01.ju.0000113299.34404.22.
- Siddiqui ZA, Gustafson GS, Ye H, Martinez AA, Mitchell B, Sebastian E, et al. 5-year outcomes of a single institution prospective trial of 19 gy single-fraction HDR brachytherapy for low- and intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys 2019;104(5):1038-44. https://doi.org/10.1016/j.ijrobp.2019.02.010.
- Tharmalingam H, Tsang Y, Ostler P, Wylie J, Bahl A, Lydon A, et al., Single dose high-dose rate (HDR) brachytherapy (BT) as monotherapy for localized prostate cancer: Early results of a UK national cohort study. Radiother Oncol 2020;143:95-100. https://doi.org/10.1016/j.radonc.2019.12.017.
- Johansson B, Olsén JS, Karlsson L, Lundin E, Lennernäs B. High-dose-rate brachytherapy as monotherapy for low- and intermediate-risk prostate cancer: long-term experience of Swedish single-center. J Contemp Brachy- therapy 2021;13(3):245–53. https://doi.org/10.5114/jcb.2021.105846.
- Anderson EM, Kim S, Sandler HM, Kamrava M. High-dose-rate fractionated brachytherapy monotherapy for localized prostate cancer: a systematic review and meta-analysis. J Contemp Brachytherapy 2021;13(4):365-72. https://doi.org/10.5114/ jcb.2021.108590.
- Hannoun-Levi JM, Chand-Fouche ME, Pace-Loscos T, Gautier M, Gal J, Schiappa R, et al. Single fraction of HDR brachytherapy for prostate cancer: Results of the SiFEPI phase II prospective trial. Clin Transl Radiat Oncol 2022;37:64-70. https://doi.org/10.1016/j.ctro.2022.08.007.
- Henry A, Pieters BR, André Siebert F, Hoskin P. UROGEC group of GEC ESTRO with endorsement by the European Association of Urology. GEC-ESTRO ACROP prostate brachytherapy guidelines. Radiother Oncol 2022;167:244-51. https://doi.org/10.1016/j.radonc.2021.12.047.