Biological fixation of customized implants for post-traumatic acetabular deformities and defects
Автор: Bazlov V. A., Pronskikh A. A., Korytkin A. A., Mamuladze T. Z., Efimenko M. V., Pavlov V. V.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 6 т.29, 2023 года.
Бесплатный доступ
Introduction The number of surgical interventions using additive technologies in medicine has been growing both in Russia and with every year. Due to the development of printing customized implants, the use of standard (imported) designs has decreased by an average of 7 % in the provision of high-tech medical care. However, the issue of the pore size of customized implants for management of post-traumatic defects in the acetabulum remains open.Objective To evaluate the results of the treatment of patients with post-traumatic acetabulum defects and deformities with the implementation in clinical practice of customized implants with structure and size porous surface that are optimal from the point of view of biological fixation.Material and methods Porous implants with different types of porous structure were produced by direct laser sintering using Ti-6Al-4V titanium alloy powders. Experimental work was carried out in vitro to determine the ability of living fibroblasts to penetrate the pores of different sizes. Next, the clinical part of this study was conducted in order to determine the signs of biological fixation of customized acetabular implants in a group of patients (n = 30).Results The results of this experiment performed to analyze the penetration of living fibroblasts into the porous structure of implants with different pore size demonstrated that metal structures with a pore size of 400-499 μm can be singled out from all others. Discussion Analysis of the literature data shows that there is no consensus on the structure and size of the pores of a customized implant. In our work, we investigated the ability of human living fibroblasts to penetrate into the surface structure of a customized implant, as a result of which we determined their optimal pore size of 400-499 microns. It should be noted that this study was conducted for a definite anatomical location: the acetabulum. However, it cannot be excluded that the data obtained are relevant for other anatomical locations.Conclusion Management of bone defects in the acetabulum area with customized implants featuring the surface pore size of 400-499 microns is a justified and relevant method. A prerequisite for the use of such implants is strict compliance with the indications for their use, careful preoperative planning and correct positioning.
Individual implant, porous surface, pore structure, 3D printing technology
Короткий адрес: https://sciup.org/142240031
IDR: 142240031 | УДК: [004.9:67.02] | DOI: 10.18019/1028-4427-2023-29-6-609-614
Текст научной статьи Biological fixation of customized implants for post-traumatic acetabular deformities and defects
The total incidence of acetabulum fractures among the adult population reported by literature sources ranges from 1 case per 50 thousand people to 3 cases per
100 thousand people per year. [1]. According to several authors, primary total hip arthroplasty may be a surgery of choice in the presence of risk factors for osteosynthesis.
Such factors include multi-fragment fractures, massive damage to the articular cartilage in loaded parts, femoral head impaction [2, 3]. Due to untimely or incorrect treatment, there is a high risk of developing complications of acetabulum fractures such as aseptic necrosis of the femoral head, or degenerative ischemic damage to intra-articular cartilage [4-6]. The main difficulties faced by a surgeon in the treatment of post-traumatic coxarthrosis are primarily acetabulum bone tissue defects that do not allow achieving strong primary fixation of standard acetabulum components [7, 8]. Different autografts can be used to replace acetabulum defects; however, in case of the treatment of the consequences acetabulum fractures, the development of post-traumatic aseptic necrosis of the femoral head does not allow the use of autobone. In such cases, concomitant acetabulum deformation requires the use of augments and individual acetabulum components. The main issues during the planning of such surgical interventions are the following: absence of a common classification of pathological acetabulum changes [9], low reliability of the standard methods of preoperative planning using plain radiographs [10, 11]. Therefore, multispiral computed tomography is required, and the surgery is planned according to the developed 3D models. In several cases, when standard acetabular components and augments do not help in replacing the defect and achieving stable biological fixation, customized implants printed on a 3D printer are used [12].
One of the most important conditions for the implant surface formation is the possibility of the integration of bone tissue into the porous structure of a customized implant [12]. The size and structure of implant surface pores are essential for interacting with bone tissue in terms of primary and subsequent biological fixation of customized implants [13]. The absence of a unified approach to determining the size and geometry of the porous structure of implants is primarily associated with the analysis of bone tissue in different anatomical zones – lower and upper extremities, bones of facial and cerebral skull – since bone tissue has different macro- and micro architecture due to its organo-specificity [14, 15]. In addition to providing stable biological fixation of the acetabular component, an important condition for achieving good functional results is the restoration of anatomical relationships in the affected joint that are close to a healthy countralateral side.
Objective To evaluate the results of the treatment of patients with post-traumatic acetabulum defects and deformities with the implementation in clinical practice of customized implants with the structure and size of their porous surface that are optimal from the point of view of biological fixation
MATERIALS AND METHODS
The study was carried out in two stages to solve the task. Stage 1 included the experiment to determine the optimal pore size and shape of titanium coating for implants. Samples of porous implants with different surface pore size were obtained by direct laser sintering using Ti-6Al-4V titanium alloy powder. Twenty samples with different sizes of porous surface were prepared for this experiment: 4 batches of 5 plates (10 mm × 10 mm × 5 mm) (Table 1).
Table 1
Description of test samples
|
Sample No. |
Pore size, micron (μm) |
Pore depth, mm |
Sample size (L × W × H) |
|
1 |
200-299 |
4 |
10 mm × 10 mm × 5 mm |
|
2 |
300-399 |
||
|
3 |
400-499 |
||
|
4 |
500-599 |
||
|
5 |
600-699 |
An in vitro experiment was conducted to determine the ability of living fibroblasts to enter the pore structure of different size. This experiment was carried out together with the Novosibirsk Federal Research Center of Fundamental and Translational Medicine. 3D printed surgical hardware samples were colonized with fibroblasts (human living fibroblast culture), then stained with fluorescent stains: Hoechst 33342 (nuclei staining), DiOC6 (mitochondria staining) and Propidium Iodide (PI, nuclei of necrotic cells staining). Fluorescence intensity was registered using a LSM710 confocal microscope (Carl Zeiss); mean fluorescence intensity (mean RFU) for each section along the Z axis (depth, μm) was evaluated; the depth analyzed was up to 2 mm. At the end of the incubation period, the medium in chamber cells was replaced with
FluoroBrite DMEM Media (Gibco, USA) that contains fluorescent stains: 5 μg/mL DiOC6, 5 μg/mL Hoechst 33342, 1 μg/mL Propidium Iodide (manufacturer: Sigma, Germany). Incubation continued 30 minutes. The medium was replaced with fresh FluoroBrite DMEM Media (Gibco, USA) and analyzed using a LSM710 confocal microscope (Carl Zeiss) in z-stack mode. Photo processing was performed using Fiji ImageJ software (NIH, USA) algorithms.
For detailed qualitative and quantitative description of such pathological acetabulum changes as deformation and bone defects, our clinic uses the method of layered 3D visualization. Choice of the tactic of implanting acetabuluar components is based on the original method developed at the Novosibirsk Research Institute of Traumatology and Orthopedics [16]. The method is carried out as follows. Based on the MSCT data, a volumetric 3D model is developed that helps to determine reference angles and lines, and the hemisphere of a healthy joint by mirror transfer of marks to the pathological side. The hemisphere is divided into three sectors that correspond to the pubic, ischial and supra-acetabular parts of the acetabulum. To determine the sector of the corresponding size, a geometric figure is selected from the pre-formed library at 1 mm intervals. The sector is spatially located in such way that at least 75 % of the surface of its base is in contact with the supporting dense bone tissue, and the apex matches the rotation center. After selecting a properly oriented sector with known values of volume and surface area, these parameters are described for each sector corresponding to the pubic, ischial and supacetabular surfaces of the acetabulum. Area difference in percentage is specified as the deformation of supporting bone tissue, and the volume difference – as the defect of the abnormal segment (Fig. 1)
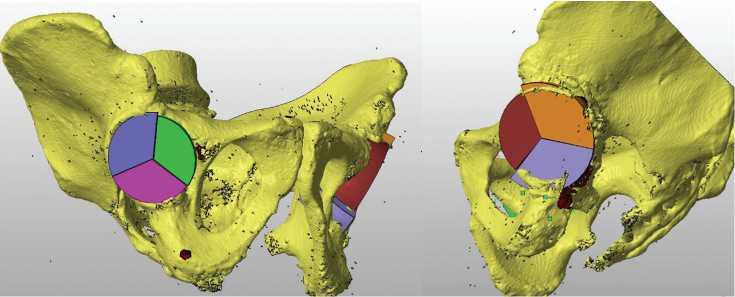
Fig. 1. Appearance of a 3D pelvic model with a sector-by-sector determination of acetabulum bone defect
In significant defects (bone deficiency of more than 40 %), it is essential to use customized acetabular components with a set polyaxial insertion of screws, or to use augments with a set direction of fixing screws.
The stage 2 of the study was carried out to determine the clinical efficacy of the proposed method: preoperative planning and surgical management of acetabulum defects with customized implants. A test group was formed that included 30 patients with significant post-traumatic acetabulum defects of grade III and IV according to AAOS classification. All patients underwent preoperative planning according to the developed algorithm [17]; customized implants with the pore size determined in the experiment (400-499 μm) were created, and surgical treatment of the defects was carried out. In addition to clinical and functional results, analyzed parameters included the state of bone tissue surrounding the customized implant, restoration of anatomical relationships in the hip joint, such as threedimensional spatial displacement of the rotation center and change in femoral offset in relation to the healthy contralateral joint parameters. Gender and age composition as well as distribution according to the defect type are presented in Table 2.
Table 2
General characteristics of the test group
|
Parameters |
Test group (n = 30) |
|
|
Type III AAOS (n = 11) |
Type IV AAOS (n = 19) |
|
|
Average age, years |
61 ± 24 |
49 ± 22 |
|
Gender (m) |
6 (20 %) |
10 (33 %) |
|
Gender (f) |
5 (17 %) |
9 (30 %) |
RESULTS
Together with the Research Institute of Experimental and Clinical Medicine (Novosibirsk), an in vitro experiment was conducted in order to analyze the ability of living fibroblasts to enter the pores of different sizes. The results obtained were subjected to statistical analysis (Table 3).
Figure 2a shows the results of implant surface confocal microscopy in the 3D mode: sample 3 (400-499 µm) – even stained, homogeneous arrangement of living fibroblasts at the depth of up to 2 mm; meanwhile, Figure 2b shows the results of the confocal microscopy of sample 2 (300-399 µm) – uneven, predominantly along pore edges, distribution of living fibroblasts at a depth of up to 2 mm in the structure of sample surface is observed.
Considering the results obtained during in vitro experiment, we observed the best penetration capacity of living human fibroblasts in sample 4 with a pore size of 400-499 μm. In the experiment, this sample was evenly colonized by living fibroblasts at a depth of up to 2 mm, while the cells remained viable with probability that was twice higher than in other samples.
In the clinical part of this study, the above approach was used in the test group (n = 30 clinical cases) for management of post-traumatic acetabulum defects grade III and IV according to AAOS with customized implants [18].
The average time of the surgery was 96.74 ± 43.57 minutes; intraoperative blood loss was 392.39 ± 198.6 mL. No revision interventions for component loosening or recurrent dislocation were required during 12 months following the surgery.
One year after the surgical treatment, the signs of biological fixation of customized implants were evaluated using the technique developed by Moore et al. [19]. Their method for assessing the biological fixation of the acetabular component of hip arthroplasty involves the analysis of five radiographic signs (Table 4).
Table 3
Results of the experiment performed to analyze the penetration of living fibroblasts into the porous structure of implants with different pore size structure
|
Sample No. |
Pore size, μm |
Maximum depth of implant colonization by culture, µm |
Evenness of colonization at a depth of 200 μm |
Staining of mitochondria with DiOC6, conditional unit |
Conditional living/necrotic cell ratio (Hoechst/ Propidium Iodide) |
|
1 |
100-299 |
50 |
even |
1 |
1/2 |
|
2 |
300-399 |
50 |
uneven |
1 |
1/1.8 |
|
3 |
400-499 |
under 250 |
even |
fluorescence intensity is twice higher |
1/1.3 |
|
4 |
500-599 |
300 |
even |
1 |
1/16 |
|
5 |
600-699 |
under 400 |
uneven |
1 |
1/1.7 |
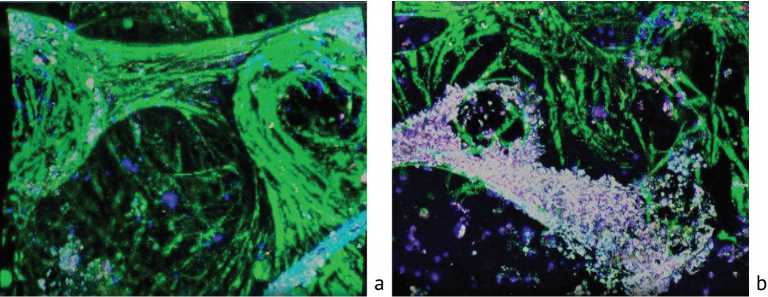
Fig. 2. Confocal microscopy in 3D mode: a – sample 3, fibroblasts are stained with green, 400-499 μm; b – sample 2, fibroblasts are stained with green, 300-399 μm
Table 4
Distribution of the number of radiographic signs of bone tissue change in the acetabulum region corresponding to the biological fixation of customized implants in the sample
|
Number of Rg signs of biological bone tissue fixation |
Patients (n = 30) |
% |
|
5 |
4 |
13.4 |
|
4 |
10 |
33.2 |
|
3 |
12 |
39.8 |
|
2 |
2 |
6.8 |
|
1 |
2 |
6.8 |
Moore et al. in their work proved that implants with three or more biological fixation signs had no manifestations of loosening [19]. Thus, after one year following the surgery, 86.8 % of patients had 3 or more radiographic signs; this fact indicates that there was no loosening of the customized components in the acetabulum area.
Tendency in the recovery of anatomical relationships were registered according to radiographs and MSCT before surgery and 12 months after it (Table 5).
Table 5
Shift of anatomical parameters in regard to healthy contralateral joint in mm
|
Parameter |
Value before surgery |
Value 12 months after surgery |
|
Vertical shift |
12.89 ± 12.42 |
3.72 ± 3.69 |
|
Horizontal shift |
11.09 ± 12.93 |
5.87 ± 3.96 |
|
Anterior-posterior shift |
8.41 ± 7.81 |
2.09 ± 1.21 |
|
Offset |
7.37 ± 8.54 |
4.20 ± 2.85 |
The results obtained prove that due to the rational preoperative planning and use of customized implants, the most accurate restoration of anatomical relationships in the replaced joint was achieved in relation to a healthy contralateral joint.
In the test group (n = 30), VAS parameters were evaluated, as well as the results of Harris and SF-36 questionnaires over time, i.e. before surgical treatment, at discharge and a year after surgical intervention. Results are shown in Table 6.
In the test group (n = 30), there was a significant decrease in VAS score from 7.4 to 2.7 twelve months after surgery with the use of customized implants (on average by 47 %); this fact demonstrates an effective reduction in pain syndrome. Assessment of the changes in Harris Hip Score demonstrates that the average value increased from 48 to 75 points over 12 months (on average by 23 %), so, it can be characterized as excellent and good results. SF-36 questionnaire also showed a significant increase in the quality of physical and mental health: average PH value increased by 46.7 %, MH value – by 38 %.
The pore size of a customized implant surface equal to 400-499 μm is optimal from the point of view of expected biological integration of bone tissue into implant surface up to 2 mm depth and, as a result, it determines good subsequent fixation of the implant that is confirmed by the X-ray signs of the changes in bone tissue of the acetabulum region. These data were also supported by an in vitro experiment conducted with the use of confocal microscopy.
Table 6
Evaluation of Harris and VAS scores and SF-36 questionnaire in the test subgroup (n = 30) over time
|
Parameter |
Before surgery |
12 months after surgery |
Intragroup comparison, Mann – Whitney U test |
||
|
Me [Q1; Q3] |
Me [Q1; Q3] |
Difference [95 % CI] |
p value |
||
|
VAS, points |
8 [7; 8] |
2.5 [2; 3] |
0-1: -3.5 [-4.0; -3.0] 0-2: -5 [-5.5; -4.5] 1-2: -1.5 [-2.0; -1.0] |
0-1: < 0.001* 0-2: < 0.001* 1-2: < 0.001* |
|
|
Harris, points |
48 [38.2; 52] |
75 [73.2; 78] |
0-1: 57 [48.0; 61.5] 0-2: 56.5 [46.0; 60.5] 1-2: -1.5[-6.0; 4.5] |
0-1: < 0.001* 0-2: < 0.001* 1-2: < 0.469 |
|
|
SF-36, % |
PH |
27.5 [24;29.7] |
65.5 [61;71] |
0-1: 26 [22.0; 29.0] 0-2: 39.5 [32.0; 43.0] 1-2: 12.5 [8.5; 15.5] |
0-1: < 0.001* 0-2: < 0.001* 1-2: < 0.001* |
|
MH |
31.5 [29.2;35] |
67 [65; 69.7] |
0-1: 27.5 [25.0; 30.0 0-2: 33.5 [28.0; 39.0] 1-2: 8.5 [4.5; 11.5] |
0-1: < 0.001* 0-2: < 0.001* 1-2: < 0.001* |
|
Assessment of social and clinical adaptation parameters (VAS, Harris, SF36 questionnaires) confirmed the high effectiveness of customized implants with set surface structure over time. However, it should be mentioned that this study was carried out within a narrow anatomical location, i.e. the acetabulum, accordingly, it cannot be ruled out that the data obtained are also relevant for other anatomical areas.
DISCUSSION
Laser selective sintering technology enables to manufacture implants with pore size control up to 20 microns [20, 21, 22].
However, the authors note that the optimal pore size of a customized implant surface has not been determined. The lack of a unified approach to determining the size and geometry of the porous structure of the implant is primarily due to the study of bone tissue of various anatomical zones – the lower and upper extremities, the bones of the facial and cerebral skull – because bone tissue, depending on organ specificity, differs in its macro- and microarchitectonics [15, 23]. Taniguchi Naoya in his work examined three samples of porous titanium implants (with an estimated porosity of 65 % and a pore size of 300, 600 and 900 microns), designated as implants P300, P600 and P900 [23].
Accordingly, the P600 implant (632 microns) demonstrated significantly higher fixation ability after 2 weeks than the other implants. After 4 weeks, all models showed a sufficiently high fixation ability in the detach test.
Ran Qichun et al. work studied the effect of the pore size of implants on biological characteristics (in particular osseointegration), conducted a number of experiments on implants with a pore size of 500-699 and 700-900 microns, both in vivo and in vitro [24, 25, 26]. According to the study, implants printed on a 3D printer with a given pore size up to 600 microns outperform the other groups in terms of osseointegration of bone tissue into the porous structure of the implant surface.
Yuhao Zheng, Jing Zhang et al. in their study of the porous surface of customized implants noted that the issue of the implant surface with a pore size of less than 300 microns was not well investigated at the moment. Yuhao Zheng, examining the average pore sizes of cylindrical implants 542, 366, and 134 microns, indicated that with a porosity of more than 60 %, the optimal pore size is 366 microns; however, they did not describe the pore geometry [27, 28, 29, 30].
The pore size of 400-499 microns of the surface of a customized implant is optimal for managing post-traumatic acetabular defects from the point of view of the predicted biological fixation of the bone. This approach determines a good subsequent fixation of the implant, which is confirmed by the presence of radiological signs of changes in the bone tissue of the acetabulum area. The findings are also confirmed by an in vitro experiment conducted using confocal microscopy. However, it is worth noting that this study was conducted for a definite anatomical location – the acetabulum. However, it cannot be excluded that the data obtained are relevant for other anatomical zones.
CONCLUSION
The analysis of porous structure size in this experimental work led to conclusion that the optimized parameter of implant surface porous structure for better osteogenic result is 400-499 μm. Too small or too large pore size may more or less interfere with cellular behavior and bone regeneration. Thus, the management of bone defects in the acetabulum region using customized implants with the surface of a mesh porous structure (400-499 μm) is a justified method that is also relevant and socially significant due to the increasing number of patients requiring such surgical interventions. A mandatory condition for using such implants is strict compliance with the indications for their use, careful preoperative planning, and correct positioning.
Conflict of interest All authors declare no conflict of interest.
Funding source The study was conducted within the framework of the state task "Improvement of diagnostic methods, preoperative planning and surgical treatment of patients with severe arthrosis of large joints, deformities and consequences of injuries of the lower extremities using additive technologies" (R&D state registration number 121051100289-0).
Ethical approval Ethical expertise conducted. Extract No. 005/23-5 from the protocol of the meeting 002/23 dated 16 February 2023 Informed consent All patients singed informed consents for conduction of the study and treatment.
Список литературы Biological fixation of customized implants for post-traumatic acetabular deformities and defects
- Laird A, Keating JF. Acetabular fractures: a 16-year prospective epidemiological study. J Bone Joint Surg Br. 2005;87(7):969-73. doi: 10.1302/0301-620X.87B7
- Madhu R, Kotnis R, Al-Mousawi A, et al. Outcome of surgery for reconstruction of fractures of the acetabulum. The time dependent effect of delay. J Bone Joint Surg Br. 2006;88(9):1197-203. doi: 10.1302/0301-620X.88B9.17588
- Stibolt RD Jr, Patel HA, Huntley SR, et al. Total hip arthroplasty for posttraumatic osteoarthritis following acetabular fracture: A systematic review of characteristics, outcomes, and complications. Chin J Traumatol. 2018;21(3):176-181. doi: 10.1016/j.cjtee.2018.02.004
- Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003;(407):173-186. doi: 10.1097/00003086-200302000-00026
- Grubor P, Krupic F, Biscevic M, Grubor M. Controversies in treatment of acetabular fracture. Med Arch. 2015;69(1):16-20. doi: 10.5455/ medarh.2015.69.16-20
- Beletskiy AV, Voronovich AI, Murzich AE, et al. Determination of Indications to Surgical Treatment and Choice of Surgical Approaches in Complicated Complex Acetabular Fractures. N.N. Priorov journal of traumatology and orthopedics. 2010;17(4):30-37. (In Russ.)
- Lai O, Yang J, Shen B, Zhou Z, Kang P, Pei F. Midterm results of uncemented acetabular reconstruction for posttraumatic arthritis secondary to acetabular fracture. J Arthroplasty. 2011;26(7):1008-1013. doi: 10.1016/j.arth.2011.02.026
- Salama W, Ditto P, Mousa S, et al. Cementless total hip arthroplasty in the treatment after acetabular fractures. Eur J Orthop Surg Traumatol. 2018;28(1):59-64. doi: 10.1007/s00590-017-2021-x
- Solod EJ, Lazarev AF, Sakharnykh IN, Stoyukhin SS. New technologies of Acetabular Osteosynthesis. Medical alphabet. 2014; 11(2): 6-10. (In Russ.)
- Romanova SV, Pronskikh AA, Mamuladze TZ, et al. Classification of posttraumatic defects and deformations of the acetabulum. Literature review. Modern problems of science and education. 2022;(6-2). doi: 10.17513/spno.32116
- Toropov SS, Artyukh VA, Bozhkova SA. Possibilities of X-ray diagnostics in preoperative planning in chronic periprosthetic infection of the hip joint. Modern achievements of traumatology and orthopedics: collection of scientific articles. SPb.: RNIITO im. R.R. Vredena Publ.; 2018:244-247.
- Nikolaev N.S., Malyuchenko L.I., Preobrazhenskaia E.V., et al. Use of customized acetabular components for hip joint arthroplasty in posttraumatic coxarthrosis. Genij Ortopedii. 2019;25(2):207-213. doi: 10.18019/1028-4427-2019-25-2-207-213
- Kryukov EV, Brizhan LK, Buryachenko BP, Varfolomeev DI. The use of digital planning for hip replacementin the orthopedic department of the "Main military clinical hospital named of N.N. Burdenko" Ministry of Defense of the Russian Federation. Department of traumatology and orthopedics. 2017;3(29):95-99. (In Russ.)
- Zhang Y, Sun N, Zhu M, et al. The contribution of pore size and porosity of 3D printed porous titanium scaffolds to osteogenesis. Biomater Adv. 2022;133:112651. doi: 10.1016/j.msec.2022.112651
- Taniguchi N, Fujibayashi S, Takemoto M, et al. Effect of pore size on bone ingrowth into porous titanium implants fabricated by additive manufacturing: An in vivo experiment. Mater Sci Eng C Mater Biol Appl. 2016;59:690-701. doi: 10.1016/j.msec.2015.10.069
- Korytkin AA, Orlinskaya NY, Novikova YS, et al. Biocompatibility and Osseointegration of Calcium Phosphate-Coated and Non-Coated Titanium Implants with Various Porosities. Modern technologies in medicine. 2021;13(2):52-57. (In Russ.) doi: 10.17691/stm2021.13.2.06
- Pronskikh AA, Romanova SV, Lukinov VL, et al. Total Hip Arthroplasty in Patients With Post-Traumatic Bone Defects and Acetabular Deformities. Traumatology and Orthopedics of Russia. 2022;28(4):66-78. doi: 10.17816/2311-2905-2001
- Tikhilov RM, Shubnyakov II, Chiladze IT, et al. Choice of surgical approach for acetabular component's implantation using current classification for arthritis following acetabular fracture. Traumatology and orthopedics of Russia. 2011;17(2):37-43. (In Russ.)
- Moore MS, McAuley JP, Young AM, Engh CA Sr. Radiographic signs of osseointegration in porous-coated acetabular components. Clin Orthop Relat Res. 2006;444:176-183. doi: 10.1097/01.blo.0000201149.14078.50
- Wang H, Su K, Su L, et al. The effect of 3D-printed Ti6Al4V scaffolds with various macropore structures on osteointegration and osteogenesis: A biomechanical evaluation. J Mech Behav Biomed Mater. 2018;88:488-496. doi: 10.1016/j.jmbbm.2018.08.049
- Wang X, Xu H, Zhang J. Using personalized 3D printed Titanium sleeve-prosthetic composite for reconstruction of severe segmental bone loss of proximal femur in revision total hip arthroplasty: A case report. Medicine (Baltimore). 2020;99(3):e18784. doi: 10.1097/MD.0000000000018784
- Zanasi S, Zmerly H. Customised three-dimensional printed revision acetabular implant for large defect after failed triflange revision cup. BMJ Case Rep. 2020;13(5):e233965. doi: 10.1136/bcr-2019-233965
- Wyatt MC. Custom 3D-printed acetabular implants in hip surgery--innovative breakthrough or expensive bespoke upgrade? Hip Int. 2015;25(4):375-9. doi: 10.5301/hipint.5000294
- Ran Q, Yang W, Hu Y, et al. Osteogenesis of 3D printed porous Ti6Al4V implants with different pore sizes. J Mech Behav Biomed Mater. 2018;84:1-11. doi: 10.1016/j.jmbbm.2018.04.010
- Wang H, Su K, Su L, et al. Comparison of 3D-printed porous tantalum and titanium scaffolds on osteointegration and osteogenesis. Mater Sci Eng C Mater Biol Appl. 2019;104:109908. doi: 10.1016/j.msec.2019.109908
- Li K, Guo A, Ran Q, et al. A novel biocomposite scaffold with antibacterial potential and the ability to promote bone repair. J Biomater Appl. 2021;36(3):474-480?doi: 10.1177/0885328221994448
- Zheng Y, Han Q, Wang J, et al. Promotion of Osseointegration between Implant and Bone Interface by Titanium Alloy Porous Scaffolds Prepared by 3D Printing. ACS Biomater Sci Eng. 2020;6(9):5181-5190. doi: 10.1021/acsbiomaterials.0c00662
- Jing Z, Zhang T, Xiu P, et al. Functionalization of 3D-printed titanium alloy orthopedic implants: a literature review. Biomed Mater. 2020;15(5):052003. doi: 10.1088/1748-605X/ab9078
- Yang S, Jiang W, Ma X, et al. Nanoscale Morphologies on the Surface of 3D-Printed Titanium Implants for Improved Osseointegration: A Systematic Review of the Literature. Int J Nanomedicine. 2023;18:4171-4191. doi: 10.2147/IJN.S409033
- Wixted CM, Peterson JR, Kadakia RJ, Adams SB. Three-dimensional Printing in Orthopaedic Surgery: Current Applications and Future Developments. J Am Acad Orthop Surg Glob Res Rev. 2021;5(4):e20.00230-11. doi: 10.5435/JAAOSGlobal-D-20-00230


