Clinical and functional outcomes of acute distal tibia fractures treated with Ilizarov external fixation: a retrospective study
Автор: Dhawan M., Nandan B., Iqbal M.S., Singh S.K., Prasad M.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 4 т.31, 2025 года.
Бесплатный доступ
Introduction Distal tibia pilon fractures are complex injuries involving the tibial articular surface. Managing these fractures requires balancing stable fixation with soft tissue preservation. The Ilizarov technique offers a minimally invasive alternative to traditional open reduction and internal fixation (ORIF), allowing for gradual correction and early weight bearing. This study aimed to evaluate functional and radiological outcomes in patients with distal tibia fractures managed by limited open reduction and Ilizarov fixation. Materials and Methods The study was conducted in a tertiary care hospital's Department of Orthopaedics over two years. The inclusion criteria were patients aged >18 years with distal tibia fractures. Exclusion criteria included refracture, previous surgeries, and associated vascular injury. The study included 20 patients (18 males, 2 females) with a mean age of 39.2 ± 10.5 years. Most injuries (80 %) were due to road traffic accidents. Fracture patterns were classified according to the AO-OTA classification. The surgical procedure involved placing the patient supine under spinal anesthesia. Traction was applied, and fluoroscopy was used to assess reduction. A three-ring tibial Ilizarov frame was assembled and applied, with additional fixation for the calcaneum. The median time to full weight bearing was 26 days. Results At frame removal, all cases had ankle stiffness, but two months post-removal, 85 % of cases had full ankle range of motion. The median time to frame removal was 17.5 weeks, and the median time to consolidation was 22 weeks. Patellar tendon bearing cast was applied for 3 weeks followed by a PTB brace with foot extension for the next 4 weeks. Discussion The Ilizarov technique should be considered as a viable option, especially for complex fracture patterns or cases with compromised soft tissue envelopes not amenable to ORIF. Conclusion The Ilizarov technique represents a valuable approach for managing distal tibia pilon fractures, demonstrating improved clinical outcomes and minimal complications.
Ilizarov method, ankle fractures, pilon fractures, distal tibia fractures, clinical outcomes, functional outcomes
Короткий адрес: https://sciup.org/142245422
IDR: 142245422 | УДК: 616.718.56-001.5-089.227.84-089.168 | DOI: 10.18019/1028-4427-2025-31-4-463-470
Текст научной статьи Clinical and functional outcomes of acute distal tibia fractures treated with Ilizarov external fixation: a retrospective study
Distal tibia pilon fractures are notoriously complex injuries, involving the articular surface of the tibia. Managing these fractures requires a delicate balance between achieving stable fixation and preserving soft tissue integrity. The Ilizarov technique allows for gradual correction, axial alignment, and controlled distraction osteogenesis. Unlike traditional open reduction and internal fixation (ORIF), which can be challenging in the presence of compromised soft tissues, the Ilizarov method offers a minimally invasive alternative [1]. Advantages of minimized soft tissue disruption, customizable alignment control, ligamentotaxis with biological stimulation and early weight-bearing, all combined to make it an attractive option in the management of these injuries [2].
Our aim was to observe functional and radiological outcomes in patients with distal tibia fractures managed by limited open reduction and Ilizarov fixation with follow-up at the time of frame removal and three months after frame removal. Our primary objectives were to assess the functional outcomes using the Olerud and Molander ankle score (OMAS) [3], and ASAMI Functional criteria [4]; and radiological outcomes using Teeny – Wiss radiological scoring system [5], time to consolidation with ASAMI Bone criteria [4]. Pain was assessed by visual analog score (VAS). Secondary objectives included assessment of complications including pin-tract infection, pin loosening, vascular/nerve injury, axial deviation, knee and ankle joint stiffness, skin necrosis, foot drop and post-operative stiffness.
MATERIALS AND METHODS
The present study was conducted in a tertiary care hospital at the Department of Orthopaedics over a two-year period from January 2022 to December 2023. All patients were operated on by a single senior surgeon at the Sir Ganga Ram Hospital. Ethical clearance was obtained from the Institutional Ethics Committee prior to the start of the study and written informed consent was obtained from the study participants. The inclusion criteria for our study were age >18 years, a history of distal tibia fracture (open or closed). Exclusion criteria were refracture of the distal tibia, previous surgeries in the affected ankle and any associated vascular injury. The study population was selected among the patients who were admitted with distal tibia fractures, intra-articular or extra-articular and provided a written informed consent to the operative procedure.
We had a total of 20 patients in our study. There were 18 (90 %) males and 2 (10 %) females. Their ages ranged between 24–57 years with a mean of 39.2 ± 10.5 years and median of 39 (30.5–45) years. Most injuries were secondary to road traffic accidents (n = 16; 80 %), followed by a fall from a height (n = 4; 20 %). Most of the injuries presented closed at the outset (n = 12; 60 %), followed by grade I open (n = 6; 30 %) and grade II open (n = 2; 10 %) as per the Gustilo – Anderson classification for open fractures. We did not encounter any grade III open injuries. Occupations of the study subjects included students (n = 8, 40 %), farmers (n = 8, 40 %) and business owners (n = 4, 20 %). None of the subject cohort had any pre-existing risk factor for delayed union or nonunion in the form of diabetes mellitus, smoking, malnutrition, or usage of anti-inflammatory medications at time of enrollment in the study. Distribution of the fracture pattern as per AO-OTA classification is detailed in Figure 1.
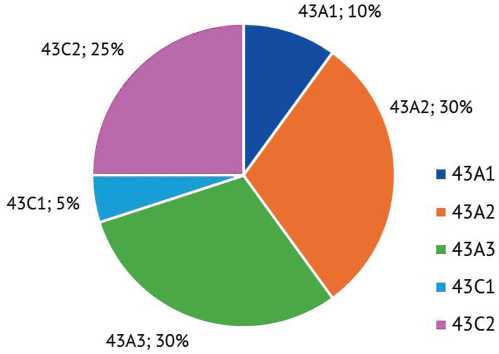
Pre-operative management Fig. 1 Distribution of fracture patterns as per AO-OTA classification
All patients presenting with an ankle injury were evaluated and resuscitated as per ATLS protocol, above knee splinting was performed, appropriate wound dressing was done for open injuries and radiographic imaging was carried out. Following imaging, fractures around the ankle joint were classified as per the OTA classification as 43-A, 43-B, and 43-C, based on the fracture configuration (Fig. 2). All subjects having an ankle fracture without significant comminution were subjected to an NCCT with 3D Reconstruction of the ankle for better understanding of the fracture pattern and planning of fixation. Ilizarov fixation was performed in all cases irrespective of blister formation or severe swelling, as wires and half-pins help in decompressing the compartment.
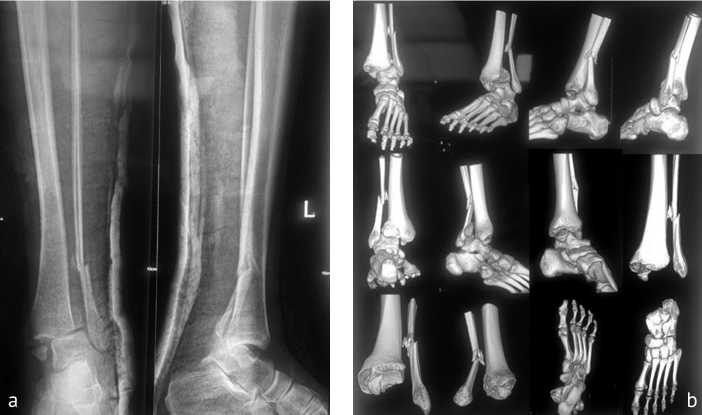
Fig. 2. Fracture images: a — AP and lateral X-rays featuring a 43-C ankle fracture dislocation as per OTA classification; b — 3D CT scan of the fracture
Surgical Management
The patient was placed supine on a radiolucent table and procedure was performed under spinal anesthesia. The limb was prepared from the iliac crest till the foot and placed over bolsters. Traction was achieved by an assistant holding the heel and forefoot. Fluoroscopy was used for assessment of reduction achieved after traction and ligamentotaxis. With traction on, fibula was first fixed with an intramedullary 1.8-mm Ilizarov wire inserted from the tip of the lateral malleolus under an image intensifier to achieve length. Fixation of the fibula indirectly reduced tibial fragments in most cases. Distal tibial fracture reduction was carried out either closed using axial traction and push-pull technique using 3-mm K-wire as joystick or limited open reduction either anteriorly or posteriorly, depending on reduction of the articular block. Wherever needed, 4-mm partially threaded cannulated screws were used for articular block reconstruction (Fig. 3). The metaphyseal zone of the injury was not opened to preserve biology. A three-ring tibial Ilizarov frame was assembled on the table using two full rings for diaphyseal fixation and one full ring for epiphyseal fixation. One 5/8th ring was applied in the calcaneum in lieu of a foot frame, for an ankle spanning construct to achieve ankle diastasis and stability. The upper two diaphyseal rings were fixed using two to three 1.8-mm smooth wires and sometimes reinforced with one 5-mm Schanz pin. The third epiphyseal full ring was fixed with three 1.8-mm olive wires passed distal to the fracture site parallel to the ankle joint line with an intervening angle of at least 30 degrees and with one wire to fix the ankle syndesmosis. The wires were duly tensioned after insertion (Fig. 4, 5). All cases which were open fractures, underwent a thorough wound debridement with saline, povidone iodine and hydrogen peroxide, followed by either primary closure or repeat debridement and delayed primary closure. None of our patients underwent any reconstructive procedure in the form of skin grafting or flaps.
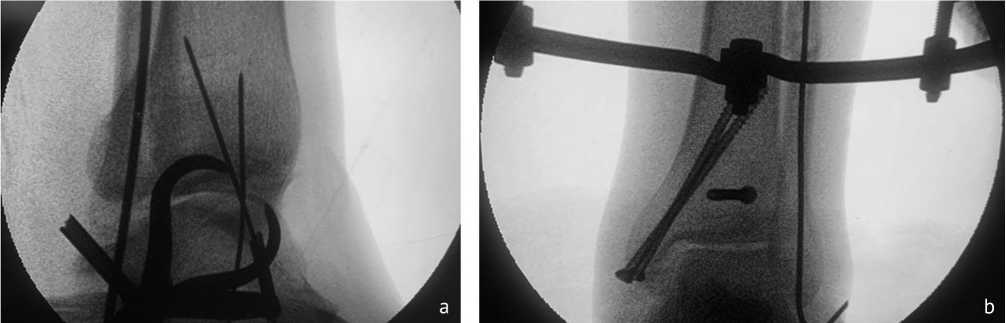
Fig. 3. Intraoperative images: a — lateral projection of the C-shaped arch of the fracture reduced by closed means and provisional fixation using K-wires; b — C-arm AP images of the fracture fixation using percutaneous means

Fig. 4. Clinical picture of the Ilizarov frame applied: a — medial view;
b — anterior view
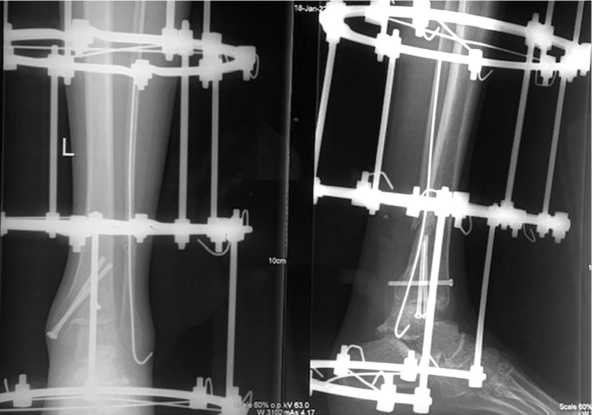
Fig. 5. Post-operative AP and lateral X-rays of the fracture fixation with the Ilizarov frame in situ
Post-operative management
Postoperatively, all patients were encouraged to perform active and passive toe and knee range of motion exercises. All wounds and pin-tracts were dressed using aseptic precautions. All patients started on Tab Aspirin 150 mg once a day for DVT prophylaxis. All patients were mobilized from post-operative day one, with those having OTA 43-A/B fractures allowed to bear weight as tolerated, and those with OTA 43-C fractures kept non-weight bearing for at least 8 weeks. Functional and radiological evaluation was done at 4 weeks, 8 weeks, at the time of frame removal and three months after frame removal. The end point for frame removal was determined by presence of bridging callus in at least three cortices in AP and lateral radiographs and by clinical impression of pain-free weight bearing following dynamization of the frame. Frame removal usually after 3–4 months was done in the operation theatre under sedation and a PTB (patellar tendon bearing) cast was applied for 3 weeks followed by a PTB brace with foot extension for the next 4 weeks.
Outcomes
The outcomes of the surgery were divided into functional and radiological outcomes. Functional outcome measures included assessment of active ankle range of motion, pain perception using Visual Analogue Scale (VAS) scores, ASAMI criteria for functional result and Olerud and Molander functional scoring system for ankle fractures. Radiological outcome measures were evaluated using Teeny – Wiss scoring criteria for radiological quality of reduction, time to bony consolidation and ASAMI criteria for bone result.
Statistical Analysis
Presentation of the categorical variables was done in the form of number and percentage. Quantitative data was presented as mean ± SD and as median with 25th and 75th percentiles (interquartile range). Data entry was done on a Microsoft Excel spreadsheet, and the final analysis was done using SPSS version 25 (SPSS Inc, Chicago, Illinois, USA).
RESULTS
All patients were mobilized from the first post-operative day using a walker support. The median time to full weight-bearing was 26 (21.75–30) days (range, 21–36 days). At the time of frame removal, all cases had stiffness in the operated ankle. At three months post-frame removal, 17 (85.00 %) cases had full ankle ROM while 3 (15.00 %) cases had a terminal restriction of dorsiflexion. The median value of frame removal of our study subjects 17.5 (16–20) weeks (range: 14–22). Functional outcomes were evaluated in the form
Table 1
VAS Scores at time of last follow up (three months post frame removal)
|
Variable |
Median (25th–75th percentile) |
Range |
|
VAS score |
2.5 (2–3) |
2–5 |
Table 2
ASAMI Functional Outcome Scoring system (three months post frame removal)
|
ASAMI functional outcome |
Number of patients |
Percentage |
|
Fair |
4 |
20.00 % |
|
Good |
10 |
50.00 % |
|
Excellent |
6 |
30.00 % |
|
Total |
20 |
100.00 % |
of VAS scores (Table 1), ASAMI Functional Outcome Scoring system (Table 2) and Olerud and Molander Ankle Scoring system (Fig. 6).
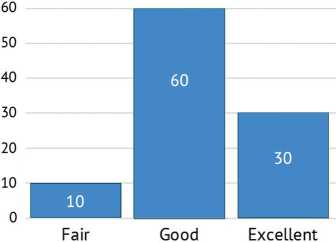
Fig. 6. Olerud and Molander Ankle Scoring system (three months post frame removal)
The median time to consolidation (weeks) of study subjects was 22 (20–24.5) weeks (range, 16–28 weeks). Radiological outcomes were evaluated with ASAMI Bone Outcome Scoring system (Table 3) and Teeny – Wiss Scoring System (Fig. 7).
Table 3
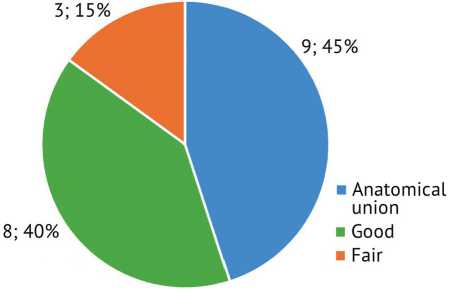
Fig. 7. Teeny – Wiss Scoring System (three months post frame removal)
ASAMI Bone Outcome Scoring system (three months post frame removal)
|
ASAMI bone outcome |
Number of patients |
Percentage |
|
Fair |
2 |
10.00 % |
|
Good |
10 |
50.00 % |
|
Excellent |
8 |
40.00 % |
|
Total |
20 |
100.00 % |
Additional procedures at the time of primary application of the Ilizarov fixator were done as follows: three cases required primary bone grafting at the tibial pilon fracture site for maintaining subchondral support for impaction fracture patterns. We encountered post-operative complications in 12 cases. Two cases developed features of Complex Regional Pain Syndrome Type-1 at frame removal, which were subsequently managed with medications. Eight cases developed pin-tract infection, despite adequate knowledge and application of pin-tract care; seven of whom were managed with local pin-site debridement and short course of oral antibiotics and one required frame re-application due to pin-tract infection and pin loosening in most of the pins. One patient developed a delayed union which was managed using compression and distraction at the fracture site (accordion maneuver) and local infiltration of autologous bone marrow concentrate injection and went on to complete union. None of our cases developed DVT, nonunion, malunion, limb length discrepancy or rotational malalignment and none of our cases required primary ankle arthrodesis or amputations.
DISCUSSION
Distal tibia fractures are a complex entity to treat [6]. Patients with these fractures are likely to develop complications post-intervention in this area with a relatively poor soft tissue envelope. A rise in rate of complications has been reported following internal fixation in this region compared with other anatomical sites. The application of Ilizarov fixator as a definite treatment for distal tibia fractures has profoundly changed their prognosis. Application of circular frame can be performed in all cases, irrespective of blister formation or severe swelling, as wires and half pins help in decompressing the compartment. By preventing soft tissue stripping needed for open reduction, the procedure minimizes soft tissue injury, decreases rate of infection, and allows early recovery. Our findings are consistent with existing literature in reporting an acceptable functional and radiological outcome following Ilizarov fixation for management of this entity.
Our study included 20 patients with a mean age of 39.2 ± 10.5 years, predominantly male (90 %). This demographic profile is consistent with other studies, such as W. Osman et al. [7] which reported a mean age of 47 years with 87 % male patients. However, our cohort was slightly younger than the study by V.P. Giannoudis et al. [8], which had a median age of 44 years (IQR 34–55).The predominance of high-energy trauma, particularly road traffic accidents (80 % in our study), aligns with global trends reported in the literature. This is similar to the findings of W. Osman et al., where 15 out of 30 fractures were due to road traffic accidents [7].
Our study utilized the AO/OTA classification, with a distribution of 43A, 43B, and 43C fractures. This is comparable to other studies, though some, like W. Osman et al. [7], used the Rüedi and Algower classification. V.P. Giannoudis et al. [8] reported 63 % intra-articular fractures in their series, which is similar to our findings of 65 % intra-articular fractures.
Bony union in our series was achieved in all except one patient in their initial frame and the patient with delayed union went on to achieve bony union following the accordion maneuver and local infiltration of bone marrow concentrate. The median time to consolidation in our study was 22 weeks, with frame removal at a median of 17.5 weeks. This is comparable to the range reported by other studies using the Ilizarov method for distal tibia fractures. For instance, J.J. Guo et al. [9] reported an average union time of 23.4 weeks in their series while W. Osman et al. [7] reported frame removal at a mean of 22 weeks. However, our time to union was shorter than that reported by V.P. Giannoudis et al. [8], who found a median time to union of 166.5 days (approximately 24 weeks). This difference could be due to variations in the definition of union, differences in patient populations, differences in weight-bearing protocols, rehabilitation, and follow-up. Previous meta-analyses also suggest union rates in our series compare favorably with patients treated for distal tibial fracture by internal fixation, with union occurring in 91–98 %. Such results are difficult to interpret due to the varied patient profiles and treatment methods undertaken, making pooled analysis difficult and its results potentially inaccurate [8].
The median time to full weight-bearing in our study was 26 days, which is notably earlier than some other studies. For instance, V.P. Giannoudis et al. [8] reported that weight-bearing was often restricted for the first 6–8 weeks in complex intra-articular fractures and T. Ramos et al. [10] reported weight-bearing at an average of 6 weeks postoperatively. This early mobilization is a significant advantage of the Ilizarov method, potentially contributing to faster rehabilitation [2].
Our study used the Olerud & Molander Ankle Scoring system for functional assessment, with 70 % of patients achieving excellent or good outcomes; these are comparable to other studies using external fixation methods. This is comparable to W. Osman et al. [7], who reported 73 % excellent or good results using the AOFAS score and slightly better than V.P. Giannoudis et al. [8], who reported 62 % good or excellent ankle scores at more than 6 months post frame removal [3]. However, they slightly outperform some internal fixation studies, such as the one by A. Korkmaz et al. [11], which reported 63 % excellent or good results. The ASAMI functional outcome scores, with 90 % excellent or good results, are particularly impressive and align with the upper range of outcomes reported in the literature for complex distal tibia fractures. The difference obtained in our study could be attributed to variations in scoring systems, patient populations, variations in surgical technique, such as the use of additional internal fixation or the specific configuration of the Ilizarov frame.
The Teeny – Wiss Scoring System results in our study, with 80 % of cases achieving good or excellent reduction, are comparable to or better than many studies using other fixation methods for complex distal tibia fractures. W. Osman et al. [7] reported excellent and good restoration of articular structure in 24 out of 30 cases.
Our overall complication rate (60 %) is higher than some reports in the literature, primarily due to pin tract infections (40 %). This is higher than the 33 % pin site infection rate reported by V.P. Giannoudis et al. [8]. However, our study had no cases of deep infection, osteomyelitis, or non-union, which is better than some reported series. For instance, W. Osman et al. [7] reported two cases of delayed union, which we did not encounter in our series. Our study may have included a higher proportion of complex fractures, leading to a higher complication rate but potentially better functional outcomes due to more meticulous management. Our study may also have used a broader definition of pin tract infections, leading to a higher reported rate.
Although we were able to assess the functional and radiological outcomes of distal tibia fractures based on available scientific literature, our study did have some limitations, notably:
-
1. Small sample size: The study included only 20 patients, which limits the statistical power and generalizability of the results.
-
2. Lack of a control group: The study did not include a control group or compare the Ilizarov method to other treatment options, making it difficult to determine the relative efficacy of this approach.
-
3. Heterogeneity of fracture types: The study included both intra-articular and extra-articular fractures, which may respond differently to treatment and complicate the interpretation of results.
-
4. Potential for recall bias: Some outcome measures were collected retrospectively, which could introduce recall bias in patient-reported outcomes.
Future research with larger sample sizes, control groups, and more comprehensive outcome measures would be beneficial to further evaluate the efficacy of the Ilizarov method for distal tibia fractures.
CONCLUSION
The Ilizarov technique represents a valuable approach for managing distal tibia pilon fractures. Our study findings align with existing evidence, demonstrating improved clinical outcomes and minimal complications. The higher complication rate but better functional outcomes in our study highlight the importance of meticulous technique and patient selection in achieving optimal results with this challenging injury. Surgeons should consider this technique as a viable option, especially when dealing with the cases of a complex fracture pattern or those with compromised soft-tissue envelope which are not amenable to ORIF.
Conflicts of Interest None to declare.
Sources of Funding None to declare.


