Complex diagnostic study of twenty-nine patients revised for periprosthetic hip joint reinfection and the role of the histological method in detection of osteomyelitis
Автор: Ermakov Artem M., Silanteva Tamara A., Naumenko Zinaida S., Kliushin Nikolai M., Malkova Tatiana A., Burtsev Alexander V.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 5 т.27, 2021 года.
Бесплатный доступ
Introduction Re-infection rates remain high after revision for periprosthtic joint infection (PJI). We conducted a complex diagnostic study of hip PJI and studied bone tissue involvement into the infectious process. Material and methods Twenty-nine patients treated for PJI were examined. Ten patients had acute, seven had late and 12 hematogenous infection (Tsukayama, 1996). Clinical, laboratory, microbiological, radiographic and histological methods were used for PJI detection. Results ESR exceeded the threshold in 16 and CRP in 23 cases. Pathogenic microorganisms were confirmed in 23 cases. Radiographic manifestations of periprosthetic bone destruction were seen in 14 patients with late and hematogenous infection. The histological study showed signs of osteomyelitis in 19 patients, including five cases with acute PJI. Histological study of periprosthetic and pseudosynovial membranes revealed PJI in 20 patients. The histological and microbiological tests together confirmed PJI in 27 cases (92 %). ROC analysis showed that the accuracy of CRP in the diagnosis of osteomyelitis exceeded that of ESR due to its higher sensitivity. Microbiological tests showed satisfactory sensitivity but low specificity. The radiographic study had an extremely low sensitivity and low specificity. Histology of membranes was quite sensitive and specific for the diagnosis of osteomyelitis but did not reach the level of bone histology. Conclusions Our complex diagnostic study has enabled to accurately characterize the septic process in revision arthroplasty. The histological findings show that osteomyelitis of different severity might develop in each PJI type. This fact may be a key factor for a surgeon in choosing a more reliable treatment option.
Arthroplasty, hip joint, periprosthetic infection, periprosthetic/pseudosynovial membrane, osteomyelitis, clinical laboratory tests, histology
Короткий адрес: https://sciup.org/142231545
IDR: 142231545 | УДК: 616.728.2-001.5-089.227.84-77-018.46-002.3: | DOI: 10.18019/1028-4427-2021-27-5-540-547
Текст научной статьи Complex diagnostic study of twenty-nine patients revised for periprosthetic hip joint reinfection and the role of the histological method in detection of osteomyelitis
Original article
Periprosthetic infection (PJI) is a devastating complication of major joint arthroplasty and requires urgent management. Several studies show that despite all preventive measures utilized, there has been no decrease in the PJI rates over time [1, 2]. The incidence of PJI is anticipated to grow proportionately to the growing number of total hip and knee arthroplasties (THA, TKA). PJI develops in one to three percent of cases after primary joint replacement and is among the top three causes of revision
arthroplasty [1–3]. Its management is not always successful due to aggressive and resistive character of infectious pathogens. Thus, re-infection rates after PIJ revision may rise to 15 % and even 50 % [1, 4–7]. Reasons of re-infection have not been sufficiently studied. The international bodies and consensus meetings agreed that the diagnostic means of implant-associated infection should include hematological, microbiological, cytological, radiological, and morphological methods of study [6–10].
However, the diagnostic algorithm for identifying PJI has been still under development due to objective difficulties [7, 10]. There is an opinion that re-infection may largely depend on underestimation of PJI that results in the erroneous choice of treatment tactics and revision operation [1, 11]. Bacteriological and histological findings of studying the biological material are of great diagnostic value for planning an appropriate therapy, especially in two-stage revision arthroplasty [3, 12]. It was shown that the histological method of studying intraoperative tissue samples is more sensitive in comparison with the bacteriological one [12, 13]. Moreover, microbiological identification of microorganisms is impossible in 10 % to 30 % of cases due to the difficulty of culturing and intake of antibiotics by patients before sampling [3, 14, 15].
Detection of osteomyelitis is of primary importance for decision making in PJI revision to choose between the three
options (debridement and implant retention, one-stage or two-stage revision). However, in contrast to the diagnostic algorithms for connective tissue study (joint fluid, and periprosthetic/pseudosynovial membranes) which have been developed and widely used in clinical practice, the morphological study of periprosthetic bone tissue has not been given due attention yet [11, 13]. This issue is very relevant since there is still no consensus regarding the detection of periprosthetic osteomyelitis and the criteria for its diagnosis [5, 16, 17].
We aimed to conduct a complex diagnosis of hip PJI in revision arthroplasty that included a histological study of bone tissue involvement into the infectious process. We hypothesized that signs of bone tissue destruction might be histologically seen not only in the late PJI stage but also in its acute phase when plain radiography is not capable to show them.
MATERIAL AND METHODS
Our study analysed a complex of diagnostic findings in a group of 29 patients that were referred to our bone infection clinic from other hospitals to be treated for hip PJI after primary THA in the period from 2016 to 2019 (Table 1).
Indications for hospitalization were pain and inflammation in the area of the previous operation, sinuses and wound discharge, and/or two positive pre-operative cultures after aspiration of the joint fluid. Exclusion criteria were patients with bilateral THA, purulent arthritis without implants, and cases of improper harvesting of tissues. Patients were included prospectively into the study and were grouped according to PJI classification of Tsukayama et al [18]. Subgroup 1 was patients with acute PJI; patients of subgroup 2 and subgroup 3 had late and hematogenous PJI, respectively. Table 1 shows demographic data, some clinical findings at admission and outcomes. Unhealed wounds, sinuses or both were present in 25 patients. Twenty patients had comorbidities associated with
the PJI risks. Informed consents for treatment and inclusion into the study were obtained from all patients. The study was approved by the ethics board of the institution.
Revision interventions were performed by one surgical team. Types of revision operations are presented in Table 1. One patient rejected revision THA in favour of resection arthroplasty [19].
All patients underwent a complex of diagnostic measures used by us in routine practice and recommended by the international consensus on periprosthetic infection [9, 20]. Hip joint radiography and fistulography were performed in the anteroposterior and lateral projections. Anteroposterior X-rays of the pelvis were taken at a focal length of one meter on RAYMAT system (Raymed, Switzerland) and Clearscope-1000 (TOSHIBA, Japan). Urografin was used as a contrast substance in fistulography. Severity of pain was rated subjectively.
Table 1
Demographic data, some clinical characteristics of patients and revision interventions
|
Subgroup |
1 (n = 10) |
2 (n = 7) |
3 (n = 12) |
|
Mean age, years (Me (95 % CI)) |
61.5 (33÷70) |
69 (44÷78) |
57 (38÷77) |
|
Male/female number |
4/6 |
2/5 |
7/5 |
|
Mean time of infection manifestation (Me (95 % CI)) |
21 (14÷28) days |
4 (1.2÷11) months |
47 (13÷84) months |
|
Wound/sinus |
10/1 |
0/6 |
2/7 |
|
Patients with associated diseases |
|||
|
Diabetes |
2 |
3 |
|
|
Renal pathology |
1 |
1 |
|
|
Immunocompromised conditions (HIV, viral hepatitis) |
2 |
2 |
|
|
Malignancy |
1 |
1 |
|
|
Obesity |
2 |
2 |
|
|
Anemia |
7 |
4 |
3 |
|
Systemic disorders |
2 |
1 |
1 |
|
Patients with cultured microorganisms |
|||
|
Monocultures |
7 |
5 |
7 |
|
Mixed cultures |
2 |
- |
2 |
|
No growth |
1 |
2 |
3 |
|
Staphylococcus species |
5 |
4 |
6 |
|
Revision surgeries and re-infection |
|||
|
Debridement |
5 |
||
|
One-stage |
1 |
1 |
3 |
|
Two-stage |
4 |
6 |
8 |
|
Resection arthroplasty |
1 |
||
|
Re-infection |
1 |
1 |
1 |
Notes: HIV – human immunodeficiency virus
The erythrocyte sedimentation rate (ESR) was determined with an automatic analyzer Roller 20pn (Alifax, Czech Republic). Concentration of C-reactive protein (CRP) in blood serum was measured with a Hitachi/BM 902 automatic biochemical analyzer (Hitachi, Japan) using reagent kits (suspension of latex particles sensitized with antibodies to human CRP), manufactured by BioSystems (Spain). Values of 54.5 mm/h for ESR and 23.5 mg/l for CRP were threshold values in the early post-operative period after THA [21], and the threshold values were 48.5 mm/h for ESR and 13.5 mg/l for CRP in late PJI [22].
Samples of bone tissue and of periprosthetic (PM) or neo-synovial membranes were harvested intraoperatively for microbiological and histological studies. The following nutrient media were used to isolate aerobic, facultative anaerobic and anaerobic bacteria, or fungi: nutrient agar containing 5 % sheep blood, yolk-salt agar, Levin medium, Sabouraud medium and Colombia agar. Tissue biopsies were homogenised; joint fluid samples were centrifuged and the sediment was studied. Plates for culturing on blood agar and on selective nutrient media were incubated in a thermostat at a temperature of 37°C for 24-48 hours. To isolate fungi, cultures were grown at a temperature of 30 °C for five days. AnaeroPack-Anaero Anaeroc gasgenerator (Mitsubishi, Japan) was used for the isolation of anaerobic microbial cultures under anaerobic conditions at 37 °C for 72 to120 hours, depending on the strain.
Samples of bone tissue harvested from the periprosthetic femur and acetabulum in 25 clinical cases and samples of periprosthetic/neo-synovial membranes in 28 clinical cases
were studied histologically. At least five pieces of tissues from one patient were fixed in 4 % neutral formalin. Bone samples were decalcified in the Richman-Gelfand-Hill mixture. Histological sections, 5 to 7 μm thick, were cut from embedded in paraffin tissue blocks and stained with hematoxylin and eosin. Light-optical microscopic investigation of histological preparations and digitilization of visual field images were performed using an AxioScope.A1 stereo microscope and an AxioCamICc5 camera, complete with Zenblue software (CarlZeiss MicroImaging GmbH, Germany).
The histological osteomyelitis evaluation score (HOES) was calculated to objectify the histopathological signs of osteomyelitis [16]. Histological types of periprosthetic or neo-synovial membranes were identified according to the consensus classification of Krenn et al [13]. The Feldman test was used for histological confirmation of the infectious process in periprosthetic tissues (more than five neutrophils in no less than five visual fields at microscopic magnification ×400) [23]. At least 10 visual fields in each tissue sample were examined.
One case from each subgroup was randomly chosen for scanning electron microscopy (SEM). Preparation and study of periprosthetic bone tissue fragments and of implant component surfaces for SEM was performed according to a certified method [24].
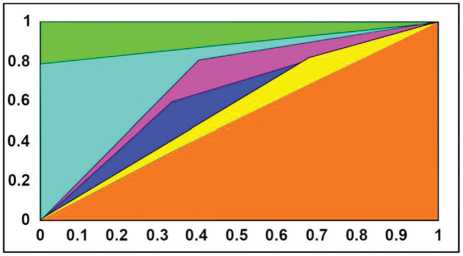
The AUC ROC test (area under the receiver operating characteristic curve) was used to assess the diagnostic methods for PJI and osteomyelitis detection [25]. The sensitivity and specificity of the methods were assessed binary relative to bone histology as a "gold standard" (Таble 3, Fig. 4).
RESULTS
ESR exceeded the threshold in 16 patients and CRP in 23 cases. Both ESR and CRP were elevated in 14 out of 29 cases. Elevated values in at least one of the laboratory tests were found in 25 patients.
Microbiological tests were negative in six individuals. Patients in subgroup 1 and subgroup 3 had a more diverse microflora: mixed bacterial cultures, methicillin-resistant staphylococci, enterococci and anaerobic bacteria of the Peptostreptococcus genus . One patient in subgroup 3 had slow developing mycelial prokaryotes of the Actinomyces genus . In subgroup 2, either monocultures of pathogens were isolated or bacterial growth was not detected. Various types of staphylococci were the dominant pathogens, coagulase-negative species being the most common. Microbiological tests revealed mostly monocultures of staphylococci ( S. aureus, S. saprophyticus, S. epidermidis ). Pathogenic strains of S. aureus were isolated in three out of six patients with a positive bacterial culture in subgroup 2 and all three had both a radiographic and histological confirmation of osteomyelitis and infected membranes.
Radiographic study did not reveal osteomyelitis in any patient of subgroup 1 (Table 2). Radiographic manifestations of periprosthetic bone tissue destruction were seen in 14 out of 19 patients of the other two subgroups (instability and implant components migration, osteolysis between the bone surface
and implant component measuring more than 2 mm, periosteal and endosteal bone response around the implant stem).
Histological evaluation of bone tissue samples available did not identify any stage of osteomyelitis only in six individuals (Table 2).
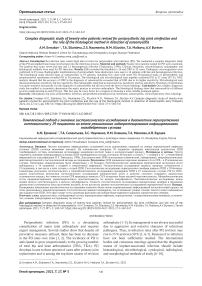
In subgroup 1, acute osteomyelitis was detected histologically in two patients (Fig. 1, a, b) and a subsided one in four patients. Osteomyelitis was confirmed in all patients of subgroup 2, mostly its chronic type, including chronic active (florid) stage (Fig. 1, c, d). Chronic osteomyelitis was also revealed in one patient of subgroup 3 with S. aureus (Fig. 1, e, f). Eleven patients out of 25 studied had histological signs of latent bone tissue infection, i.e. calmed or subsided osteomyelitis (Fig. 1, g, h).
Histological study of periprosthetic/pseudosynovial membranes (Fig. 2) showed that the infected type-II and type-III membranes were found in 20 out of 28 cases studied (Table 2).
Scanning electron microscopy of periprosthetic tissue samples from randomly selected patients supplemented the microbiological findings. In addition to the strains isolated and identified from culture media, other microbial cells were visualized directly on tissue samples and implant surface in two patients from subgroup 1 and subgroup 2 (Fig. 3, a, b). Mature biofilms of the pathogenic bacteria previously found by the standard method were seen in the tissues of a patient from subgroup 3 (Fig. 3, c).
Table 2
Radiographic and histological data on osteomyelitis and histological types of pseudosynovial/periprosthetic membranes in the patients studied
|
Subgroup |
Number of patients |
Radio-graphic signs |
Histological osteomyelitis stage / number of patients |
Histological membrane type / number of patients |
|||||||||
|
n/a |
absent |
acute |
chronic active |
chronic |
subsided |
n/a |
I |
II |
III |
IV |
|||
|
1 |
10 |
none |
1 |
3 |
2 |
0 |
0 |
4 |
1 |
1 |
3 |
3 |
2 |
|
2 |
7 |
5 |
0 |
0 |
0 |
3 |
2 |
2 |
0 |
2 |
4 |
1 |
0 |
|
3 |
12 |
9 |
3 |
3 |
0 |
0 |
1 |
5 |
0 |
3 |
5 |
4 |
0 |
|
Total |
29 |
14 |
4 |
6 |
2 |
3 |
3 |
11 |
1 |
6 |
12 |
8 |
2 |
Note: n/a – not available
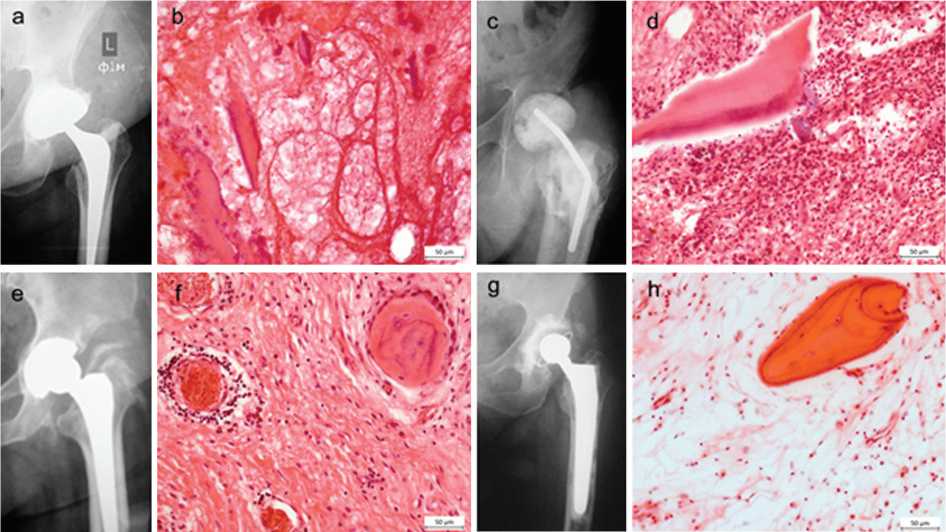
Fig. 1. Radiographic (left) and histological (right) osteomyelitic changes in the periprosthetic bone in acute PJI without radiographic signs of osteomyelitis (a) but with histological signs of acute osteomyelitis such as purulent swelling, necrosis of bone marrow and bone trabeculae (b); late PJI case with radiographic signs of osteomyelitis in the proximal femur, periostitis of the femoral cortex (c) and histological signs of chronic active osteomyelitis such as jagged bone sequestration surrounded by granulation tissue with micro-abscesses (accumulations of neutrophilic granulocytes), infiltration with lymphocytes and monocytes (d); patient (hematogenous PJI subgroup) without radiographic signs of osteomyelitis (e) but with histological signs of chronic osteomyelitis such as productive inflammation with infiltration mainly by lymphocytes and monocytes, and to a lesser extent by neutrophils, fibrosis, thrombosis of intraosseous microvessels, reactive endosteal osteogenesis (f); radiographic signs of osteomyelitis, osteolysis, destruction of the bone tissue of the femur at the bone/implant interface in a patient with hematgenous type of infection (g) and histological manifestations of subsided (calmed) osteomyelitis such as sluggish bonу remodelling, fatty bone marrow degeneration, weak infiltration by lymphocytes and monocytes (h). Paraffin sections, haematoxylin and eosin stain. Original magnification ×400; scale bar = 50 µm
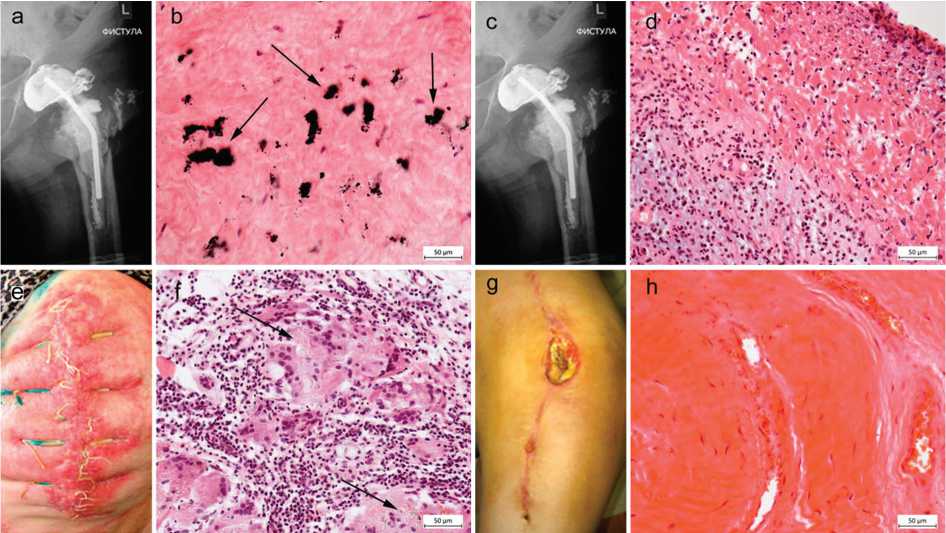
Fig. 2. Location of the inflammatory/infection process and histological features of neosynovial/periprosthetic membranes according to Krenn et al. The contrast agent is visualized in the joint cavity in the fistulogram, in the area of the lesser trochanter of the femur and washes the pelvic component of the articulating spacer, in the inguinal soft-tissue and on the medial surface of the femur (a); histological type-I membrane identified in a case of hematogenous PJI, characterized by small-cell loose fibrous connective tissue, rarely infiltrated by histiocytes and lymphocytes with inclusions (arrow) of metal wear particles (b). The contrast agent in the fistulogram is distributed in the joint cavity and under the elements of an unstable cement spacer (c); type-II membrane (late PJI case) featuring reactively and destructively altered edematous loose connective tissue which is abundantly infiltrated by inflammatory cells with dominant neutrophilic granulocytes (d). Hyperemia and swelling of the thigh soft tissues in the area of the surgical suture in acute PJI (e); type-III membrane presenting reactively-changed loose connective tissue with accumulation (arrows) of wear particles (polyethylene) surrounded by multinuclear giant cells and numerous mononuclear inflammatory cell elements; the number of neutrophils exceeds 5 in the vision field (f). Wound and a sinus with serous discharge in the thigh in a case of acute PJI (g); type-IV membrane featuring the connective tissue rich in collagen fibers, slightly edematous with severe hyperemia of blood vessels, not infiltrated by inflammatory cells (h). Paraffin sections, hematoxylin and eosin staining. Original magnification ×400; scale bar = 50 µm. Paraffin sections, hematoxylin and eosin staining. Original magnification ×400; scale bar = 50 µm
Data for construction of the ROC-curve in osteomyelitis detection
|
Methods |
TPR (SEN) |
SPE |
FPR (1-SPE) |
AUC ROC |
|
Histology of bone |
1.00 |
1.00 |
0 |
1.00 |
|
Histology of membranes |
0.83 |
1.00 |
0 |
0.92 |
|
CRP |
0.81 |
0.60 |
0.40 |
0.71 |
|
ESR |
0.63 |
0.67 |
0.33 |
0.65 |
|
Microbiology |
0.84 |
0.33 |
0.67 |
0.59 |
|
Radiography |
0.38 |
0.67 |
0.33 |
0.52 |
Notes: TPR – true positive rate; FPR – false positive rate; SEN – sensitivity; SPE – specificity; AUC ROC – area under ROC-curve
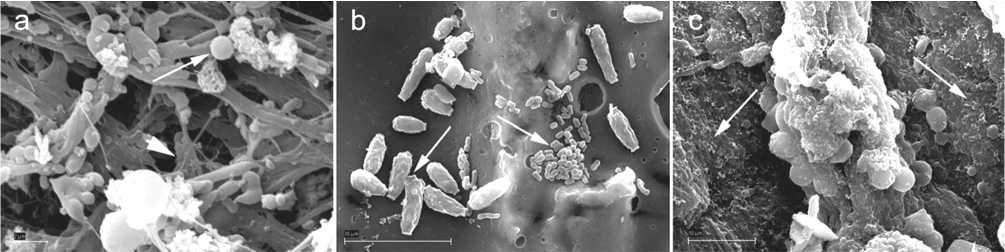
Fig. 3. Microorganisms on the surface of samples detected with SEM method. Associations (long arrow) of cocci microcolonies (bacteriological finding was S. aureus MRSA ) and hyphoid-like structures (short arrow), presumably fungi, in the periprosthetic bone tissue (a); biofilm formation of two unidentified types of microorganisms (arrows) on the surface of the femoral component (bacteriological finding was S. saprophyticus ) (b); mature biofilms (arrows) in the periprosthetic connective tissue membrane (bacteriological finding was E. faecalis ) (c). Electron scanograms, scale bar = 2 µm (а); = 10 µm (b, c)
ROC analysis revealed low accuracy of radiographic diagnosis for osteomyelitis, approaching to the probability of random selection of 0.5 (Table 3).
Among the laboratoty diagnostic indicators, the best result was obtained for CRP. The diagnostic accuracy of microbiological tests had low specificity despite its satisfactory sensitivity. Histology of periprosthetic and pseudosynovial membranes was found to be quite sensitive and specific in the diagnosis of osteomyelitis. Its diagnostic accuracy approached, but did not reach the level of bone histology (Fig. 4).
The re-infection rate in our study was 10.3 % due to underestimation of PJI in one case with mixed flora and subsided osteomyelitis in whom one-stage revision was used (subgroup 1), aggressive nature of S. aureus MRSA and chronic active osteomyelitis in the second case (subgroup 2), and rejection of two-stage revision by one more patient with E. faecalis and subsided osteomyelitis (subgroup 3). Re-infection developed within a month after the revision.
Таble 3
AUC ROC
V) c Ф
>
QT
FPR (1 - specificity)
□ Histology of bone
□ Histology of membranes
□ CRP
□ ESR
□ Microbiology
□ Radiography
Fig. 4. AUC ROC-curve (area under the receiver operating characteristic curve) for the methods used in the diagnosis of osteomyelitis. TPR – true positive rate; FPR – false positive rate
DISCUSSION
Infection remains a challenging complication of arthroplasties that is difficult to resolve. Our study revealed considerable PJI variations and heterogeneity of its clinical, laboratory and histological manifestations in the patients studied but each patient of our series, except one, featured several diagnostic findings that could verify PJI.
The generally accepted laboratory tests for diagnosis of periprosthetic inflammation are ESR and CRP [1, 9, 20]. Elevated values in at least one of these indicators were found in 86 % of our patients. It was established that they have sensitivity of not more than 75.0 % and low specificity [25]. Thus, their values within the normal range do not prove the absence of PJI [15, 27], what was also observed in our study. Normal ESR and CRP were reported in chronic low-grade PJI caused by low-virulent microorganisms. Another study found their values within the norm in 4 % of patients who underwent revision operations for hip and knee PJI [27].
Microbiological culturing has been considered the “gold standard” for diagnosing PJI in joint replacement [9, 20] According to several studies, five-year reinfection rate is 6 % after THA revision and is the same for both microbiologically negative and microbiologically positive groups of patients. It is indirect evidence that the microbiological method of infection diagnosis may not be so accurate [28]. Moreover, the literature sources show that bacteriological cultures may be negative in 15 to 20 % of PJI cases [15]. It was also shown that microbiological identification of PJI pathogens is not always correct in chronic osteomyelitis, and/or if antibiotic therapy is administered, or in the case of low-virulent bacteria [16]. Infectious microorganisms were confirmed in 79 % of our patients. According to our findings, various staphylococci were the dominant pathogens, coagulase-negative species being the most common. It is worth noting the “established” microbiocenosis of the inflammatory process featuring monocultures in most cases, including low-virulent strains of staphylococci (Staphylococcus saprophyticus) the role of which in implant-associated infection requires additional studies. However, the data obtained about the microbiocenosis are not enough to differentiate the studied patients by severity, location and prevalence of the inflammatory process in the affected joint.
The radiographic study of our patients revealed that the longer was the post-operative term after primary THA the more frequent and pronounced was bone destruction in the conditions of PJI. Bone destruction was not found with radiography in subgroup 1. However, radiographic bone tissue changes are not specific for PJI, especially in acute infection [29].
Histological investigation of periprosthetic tissues is seen as one of the most reliable methods [3, 7, 8, 14] and was recommended for PJI diagnosis [9, 20]. Moreover, the biopsy material studied histologically was found even more informative than the one studied microbiologically [12]. There is an opinion that arthrocentesis is mandatory in the diagnosis of PJI and the resulting samples should be examined both microbiologically and histologically [3]. However, given the additional costs and possible complications of invasive procedures, especially if patients are planned for two-stage revision, it is preferable to study the tissues harvested intraoperatively [11].
The incidence of occult PJI that was confirmed in the study of septic THA revisions justifies systematic intraoperative sampling [30]. Histological examination of periprosthetic tissues removed at revision, although not mandatory in many countries yet, has been considered instrumental in the classification, cell composition/ subtyping, and grading of the adverse biological events. However, in clinical practice, pseudosynovial membranes or periprosthetic membranes are commonly studied with histological methods [5, 13] while osteomyelitis is judged mainly by radiographic imaging [31]. The histological study of PMs showed signs of infectious inflammation in 20 out of 28 our patients (71 %).
We found that the histological study of periprosthetic bone tissue using the semi-quantitative HOES score [16] enabled to identify and more objectively differentiate the stages of osteomyelitis in 19 cases out of 25 samples studied. Thus, subsided osteomyelitis was found in four patients in subgroups 1 and the majority of patients in subgroup 3 while more pronounced signs of osteomyelitis prevailed in subgroup 2 (Table 2). The radiographic and histopathological diagnosis of periprosthetic osteomyelitis coinsided in 47 % only. Our data confirm the significance of histological bone destruction diagnosis in hip PJI. The evidence of osteomyelitic lesions detected by us in the periprosthetic bone proves the concept about the ways by which periprosthetic infection spreads from the joint cavity to the peri-articular tissues and from the bone metaphysis to the joint cavity [11].
The histological study of periprosthetic bone and/ or membranes was very informative. Thus, it revealed PJI in 24 of 29 patients (81 %). Infected membranes and osteomyelitiс changes were histologically seen together in 15 patients. A selective SEM study also added to the findings as it was able to reveal the microorganisms which were not identified microbiologically and showed the formation of microbial biofilms in the tissues and on the implant surface.
The histological and microbiological tests together confirmed PJI in 27 cases (92 %) of our clinical cases. The results obtained are consistent with the statement that the combination of bacteriological and histological methods has the highest diagnostic value in the diagnosis of hip PJI with a sensitivity of at least 87.5 %, specificity of 100 %, and accuracy of 95 %. [25]. Thus, the total number of infected cases confirmed with the complex of diagnostic measures recommended and utilized by us in this study was 28 patients (96 %) which is significantly higher than separate methods alone are able to detect [9, 20].
Unfortunately, histological study of periprosthetic tissues takes time and is not applicable for fast decision making. Therefore, low accuracy of routinely used methods for diagnosing periprosthetic osteomyelitis, shown by our preliminary ROC analysis, may be improved by additional tests and instrumental imaging techniques. These may include alpha defensin levels and leukocyte esterase, CT, MRI, sonography, nuclear medicine, or hybrid procedures [7, 32]. Most of these tools are available in clinical settings.
Our study confirms that current approach to the treatment of PJI in secondary arthroplasty should be similar to the treatment of chronic osteomyelitis [11]. It means that radical management involving proper debridement, excision of affected bone tissue and administration of proper antibiotics remains the most important clinical condition for prevention of re-infection and revision success [31]. Following these principles in PJI revision arthroplasty would provide low recurrence of infection [5, 11, 16, 30]. Moreover, risk factors such as age and associated conditions that aggravate the immunity and facilitate the development of infection should not be underestimated.
The patients of our diagnostic study were referred to our bone infection clinic for PJI management and were a random prospective consecutive series of cases. We acknowledge the limitations which are 1) a small group and its heterogeneity and 2) lack of histological findings in several cases due to improper collection or storage. Moreover, it was not always possible to harvest tissues from one and the same site as different techniques for PJI revision were used.
Our preliminary study investigated PJI with a complex of diagnostic tools. We did not aim to identify differences between the subgroups and investigate the risks of infection due to associated diseases. Our research focused on PJI and osteomyelitis detection with combined methods. It found that the diagnostic tools used for detection of periprosthetic osteomyelitis should be wider used. The study needs to be continued, especially in regard to the relationship of osteomyelitis and acute infection. Nevertheless, it revealed that osteomyelitic changes may appear in the periprosthetic bone early after primary THA. We believe that the histological findings of our study have direct clinical relevance. The surgeon should be aware that hidden osteomyelitis is possible in cases of acute PJI and hematogenous way of infection. Two-stage revision in doubtful and compromised cases would be then a better solution.
CONCLUSION
A complex of clinical, laboratory, microbiological, radiographic and histological methods of study in septic hip joint revision arthroplasty enables to accurately diagnose periprosthetic infection. The histological findings
show that osteomyelitis of different severity might develop in each PJI type. This fact may be a key factor for a surgeon in choosing a more reliable treatment strategy, especially in cases of acute post-operative periprosthetic infection.
Список литературы Complex diagnostic study of twenty-nine patients revised for periprosthetic hip joint reinfection and the role of the histological method in detection of osteomyelitis
- Osteomyelitis: Recent advances in pathophysiology and therapeutic strategies / M.C. Birt, D.W. Anderson, E. Bruce Toby, J. Wang // J. Orthop. 2016. Vol. 14, No 1. P. 45-52. DOI: 10.1016/j.jor.2016.10.004.
- Чрескостный остеосинтез в лечении больных хроническим остеомиелитом после эндопротезирования крупных суставов / Н.М. Клюшин, B.И. Шляхов, Б.Э. Чакушин, А.В. Злобин, С.И. Бурнашов, Ю.В. Абабков, А.Г. Михайлов // Гений ортопедии. 2010. № 2. С. 37-43.
- Diagnostic work-up strategy for periprosthetic joint infections after total hip and knee arthroplasty: a 12-year experience on 320 consecutive cases / D. Zajonz, L. Wuthe, S. Tiepolt, P. Brandmeier, T. Prietzel, G.F. von Salis-Soglio, A. Roth, C. Josten, C.E. Heyde, M. Ghanem // Patient Saf. Surg. 2015. Vol. 9. P. 20. DOI: 10.1186/s13037-015-0071-8.
- Значение клинико-рентгенологических исследований в диагностике и лечении больных с перипротезной инфекцией после эндопротезирования тазобедренного сустава / Н.М. Клюшин, А.М. Ермаков, Ю.В. Абабков, С.В. Кушнарев // Гений Ортопедии. 2017. Т. 23, № 3. С. 341345. DOI: 10.18019/1028-4427-2017-23-3-341-345.
- Evolving concepts in bone infection: redefining "biofilm", "acute vs. chronic osteomyelitis", "the immune proteome" and "local antibiotic therapy" / E.A. Masters, R.P. Trombetta, K.L. de Mesy Bentley, B.F. Boyce, A.L. Gill, S.R. Gill, K. Nishitani, M. Ishikawa, Y. Morita, H. Ito, S.N. Bello-Irizarry, M. Ninomiya, J.D. Brodell Jr., C.C. Lee, S.P. Hao, I. Oh, C. Xie, H.A. Awad, J.L. Daiss, J.R. Owen, S.L. Kates, E.M. Schwarz, G. Muthukrishnan // Bone Res. 2019. Vol. 7. P. 20. DOI: 10.1038/s41413-019-0061-z.
- 2018 International Consensus Meeting on Musculoskeletal Infection: Research Priorities from the General Assembly Questions / E.M. Schwarz, J. Parvizi, T. Gehrke, A. Aiyer, A. Battenberg, S.A. Brown, J.J. Callaghan, M. Citak, K. Egol, G.E. Garrigues, M. Ghert, K. Goswami, A. Green, S. Hammound, S.L. Kates, A.C. McLaren, M.A. Mont, S. Namdari, W.T. Obremskey, R . O'Toole, S. Raikin, C. Restrepo, B. Ricciardi, K. Saeed, J. Sanchez-Sotelo, N. Shohat, T. Tan, C.P. Thirukumaran, B. Winters // J. Orthop. Res. 2019. Vol. 37, No 5. P. 997-1006. DOI: 10.1002/jor.24293.
- Consensus document for the diagnosis of prosthetic joint infections: a joint paper by the EANM, EBJIS, and ESR (with ESCMID endorsement) / A. Signore, L.M. Sconfienza, O. Borens, A.W. J.M. Glaudemans, V. Cassar-Pullicino, A. Trampuz, H. Winkler, O. Gheysens, F.M.H.M. Vanhoenacker, N. Petrosillo, P.C. Jutte // Eur. J. Nucl. Med. Mol. Imaging. 2019. Vol. 46, No 4. P. 971-988. DOI: 10.1007/s00259-019-4263-9.
- Этиология острой перипротезной инфекции суставов и результаты ее хирургического лечения / Н.М. Клюшин, А.М. Ермаков, З.С. На-уменко, Ю.В. Абабков, А.С. Тряпичников, А.Н. Коюшков // Гений ортопедии. 2017. Т. 23, № 4. С. 417-422. DOI: 10.18019/1028-4427-201723-4-417-422.
- Parvizi J., Gehrke T.; International Consensus Group on Periprosthetic Joint Infection. Definition of periprosthetic joint infection // J. Arthroplasty. 2014. Vol. 29, No 7. P. 1331. DOI: 10.1016/j.arth.2014.03.009.
- Diagnosis of peripheral bone and prosthetic joint infections: overview on the consensus documents by the EANM, EBJIS, and ESR (with ESCMID endorsement) / L.M. Sconfienza, A. Signore, V. Cassar-Pullicino, M.A. Cataldo, O. Gheysens, O. Borens, A. Trampuz, K. Wörtler, N. Petrosillo, H. Winkler, F.M.H.M. Vanhoenacker, P.C. Jutte, A.W.J.M. Glaudemans // Eur. Radiol. 2019. Vol. 29, No 12. P. 6425-6438. DOI: 10.1007/s00330-019-06326-1.
- Tande A.J., Patel R. Prosthetic joint infection // Clin. Microbiol. Rev. 2014. Vol. 27, No 2. P. 302-345. DOI: 10.1128/CMR.00111-13.
- High diagnostic value of synovial biopsy in periprosthetic joint infection of the hip / B. Fink, A. Gebhard, M. Fuerst, I. Berger, P. Schäfer // Clin. Orthop. Relat. Res. 2013. Vol. 471, No 3. P. 956-964. DOI: 10.1007/s11999-012-2474-5.
- Revised histopathological consensus classification of joint implant related pathology / V. Krenn, L. Morawietz, G. Perino, H. Kienapfel, R. Ascherl, G.J. Hassenpflug, M. Thomsen, P. Thomas, M. Huber, D. Kendoff, D. Baumhoer, M.G. Krukemeyer, S. Natu, F. Boettner, J. Zustin, B. Kölbel, W. Rüther, J.P. Kretzer, A. Tiemann, A. Trampuz, L. Frommelt, R. Tichilow, S. Söder, S. Müller, J. Parvizi, U. Illgner, T. Gehrke // Pathol. Res. Pract. 2014. Vol. 210, No 12. P. 779-786. DOI: 10.1016/j.prp.2014.09.017.
- Holzmann T., Schneider-Brachert W. Mikrobiologische Diagnostik periprothetischer Gelenkinfektionen // Orthopade. 2015. Vol. 44, No 5. P. 344348. DOI: 10.1007/s00132-015-3087-y.
- C-reactive protein may misdiagnose prosthetic joint infections, particularly chronic and low-grade infections / D. Pérez-Prieto, M.E. Portillo, L. Puig-Verdié, A. Alier, S. Martínez, L. Sorlí, J.P. Horcajada, J.C. Monllau // Int. Orthop. 2017. Vol. 41, No 7. P. 1315-1319. DOI: 10.1007/s00264-017-3430-5.
- Histopathological Osteomyelitis Evaluation Score (HOES) - an innovative approach to histopathological diagnostics and scoring of osteomyelitis / A. Tiemann, G.O. Hofmann, M.G. Krukemeyer, V. Krenn, S. Langwald // GMS Interdiscip. Plast. Reconstr. Surg. DGPW. 2014. Vol. 3. Doc08. DOI. org/10.3205/iprs000049.
- Treatment algorithms for chronic osteomyelitis / G. Walter, M. Kemmerer, C. Kappler, R. Hoffmann // Dtsch. Arztebl. Int. 2012. Vol. 109, No 14. P. 257-264. DOI: 10.3238/arztebl.2012.0257.
- Tsukayama D.T., Estrada R., Gustilo R.B. Infection after total hip arthroplasty. A study of the treatment of one hundred and six infections // J. Bone Joint Surg. Am. 1996. Vol. 78, No 4. P. 512-523. DOI: 10.2106/00004623-199604000-00005.
- Modified Girdlestone arthroplasty and hip arthrodesis using the Ilizarov external fixator as a salvage method in the management of severely infected total hip replacement / N.M. Kliushin, Y.V. Ababkov, A.M. Ermakov, T.A. Malkova // Indian J. Orthop. 2016. Vol. 50, No 1. P. 16-24. DOI: 10.4103/0019-5413.173513.
- The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria / J. Parvizi, T.L. Tan, K. Goswami, C. Higuera, C. Della Valle, A.F. Chen, N. Shohat // J. Arthroplasty. 2018. Vol. 33, No 5. P. 1309-1314.e2. DOI: 10.1016/j.arth.2018.02.078.
- Alijanipour P., Bakhshi H., Parvizi J. Diagnosis of periprosthetic joint infection: the threshold for serological markers // Clin. Orthop. Relat. Res. 2013. Vol. 471, No 10. P. 3186-3195. DOI: 10.1007/s11999-013-3070-z.
- Serum biomarkers in periprosthetic joint infections / A. Saleh, J. George, M. Faour, A.K. Klika, C.A. Higuera // Bone Joint Res. 2018. Vol. 7, No 1. P. 85-93. DOI: 10.1302/2046-3758.71.BJR-2017-0323.
- The Rule of Histology in the Diagnosis of Periprosthetic Infection: Specific Granulocyte Counting Methods and New Immunohistologic Staining Techniques may Increase the Diagnostic Value / F. Boettner, G. Koehler, A. Wegner, T. Schmidt-Braekling, G. Gosheger, C. Goetze // Open Orthop. J. 2016. Vol. 10. P. 457-465. DOI: 10.2174/1874325001610010457.
- Challenging Diagnostics of Biofilm Associated Periprosthetic Infection in Immunocompromised Patient: A Clinical Case / Z.S. Naumenko, T.A. Silanteva, A.M. Ermakov, N.V. Godovykh, N.M. Klushin // Open Access Maced. J. Med. Sci. 2019. Vol. 7, No 5. P. 786-790. DOI: 10.3889/ oamjms.2019.180.
- Obuchowski N.A. Receiver operating characteristic curves and their use in radiology // Radiology. 2003. Vol. 229, No 1. P. 3-8. DOI: 10.1148/ radiol.2291010898.
- Diagnostic accuracy of arthroscopic biopsy in periprosthetic infections of the hip / F. Pohlig, H.M. Mühlhofer, U. Lenze, F.W. Lenze, C. Suren, N. Harrasser, R. von Eisenhart-Rothe, J. Schauwecker // Eur. J. Med. Res. 2017. Vol. 22, No 1. P. 6. DOI: 10.1186/s40001-017-0246-0.
- Seronegative infections in hip and knee arthroplasty: periprosthetic infections with normal erythrocyte sedimentation rate and C-reactive protein level / B.A. McArthur, M.P. Abdel, M.J. Taunton, D.R. Osmon, A.D. Hanssen // Bone Joint J. 2015. Vol. 97-B, No 7. P. 939-944. DOI: 10.1302/0301-620X.97B7.35500.
- Ibrahim M.S., Twaij H., Haddad F.S. Two-stage revision for the culture-negative infected total hip arthroplasty: A comparative study // Bone Joint J. 2018. Vol. 100-B, No 1 Supple A. P. 3-8. DOI: 10.1302/0301-620X.100B1.BJJ-2017-0626.R1.
- Mulcahy H., Chew F.S. Current concepts of hip arthroplasty for radiologists: part 2, revisions and complications // AJR Am. J. Roentgenol. 2012. Vol. 199, No 3. P. 570-580. DOI: 10.2214/AJR.12.8844.
- Periprosthetic joint infection in aseptic total hip arthroplasty revision / G. Renard, J.M. Laffosse, M. Tibbo, T. Lucena, E. Cavaignac, J.L. Rouvillain, P. Chiron, M. Severyns, N. Reina // Int. Orthop. 2020. Vol. 44, No 4. P. 735-741. DOI: 10.1007/s00264-019-04366-2.
- Panteli M., Giannoudis P.V. Chronic osteomyelitis: what the surgeon needs to know // EFORT Open Rev. 2017. Vol. 1, No 5. P. 128-135. DOI: 10.1302/2058-5241.1.000017.
- Zur Definition der Diagnose Osteomyelitis - Osteomyelitis-Diagnose-Score (ODS) / H.G. Schmidt, A.H. Tiemann, R. Braunschweig, M. Diefenbeck, M. Bühler, D. Abitzsch, N. Haustedt, G. Walter, R. Schoop, V. Heppert, G.O. Hofmann, M. Glombitza, C. Grimme, U.J. Gerlach, I. Flesch; Arbeitsgemeinschaft septische Chirugie der DGOUC10 // Z. Orthop. Unfall. 2011. Vol. 149, No 4. P. 449-460. DOI: 10.1055/s-0030-1270970.