Definitive fixation of open tibial fractures using the Ilizarov ring fixator: an analysis of functional outcomes
Автор: Radhakrishnan E., Duraisamy E.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 2 т.31, 2025 года.
Бесплатный доступ
Introduction Open tibial fractures are generally managed by wound debridement and temporary stabilisation with AO external fixators followed by delayed internal fixation provided the soft tissue cover is adequate and there is no infection. This study aims at analysing the factors influencing the outcome of treatment of open tibial fractures using external fixation with Ilizarov ring fixators as definitive method.Materials and methods Twenty eight patients of both sexes aged more than 18 years who presented with open tibial fractures were included as our study subjects. The open fractures were classified according to Gustilo-Anderson classification of open fractures. Skeletal stabilisation was done either with Ilizarov ring fixators primarily or with AO external fixators in whom within 5 days since the injury the Ilizarov ring fixators were applied after thorough debridement of wounds. Patients were followed up first 4 weeks after the definitive procedure, then after 6 weeks, 3 months, 6 months and 1 year. The results were analysed using Tuckers criteria.Results We achieved union in 25 patients without infection. Three patients were lost for follow-up. In majority of patients (48 %) union occurred in 24 weeks. In 10 patients we had pin site infections. The functional outcome was studied using Tucker’s Criteria according to which 5 patients (20 %) had excellent outcomes, 9 patients (33 %) had good outcomes, 8 patients (29 %) had fair outcomes and 3 (16 %) had poor outcomes.Discussion Limitation of the present study is the absence of a comparison group, though it was possible because of the nature of the injuries that these patients had while arriving at the trauma care facility. Another limitation is the follow-up period. We followed the patients for one year but if we followed the patents for longer periods we could have assessed the long-term prognosis.Conclusion The definitive treatment of open tibial fractures especially Type 3B fractures with the Ilizarov Ring Fixator system is found be optimal and cost-effective.
Open tibial fractures, ilizarov method, definitive fixation
Короткий адрес: https://sciup.org/142245091
IDR: 142245091 | УДК: 616.718.5-001.514-089.227.84-089.168 | DOI: 10.18019/1028-4427-2025-31-2-143-152
Текст научной статьи Definitive fixation of open tibial fractures using the Ilizarov ring fixator: an analysis of functional outcomes
With the increase in the number of automobiles and national highways, India ranks number two in the list of road traffic accidents among 207 countries as per World Road Statistics 2020 published by the International Road Federation in Geneva. In 2021, India recorded a mammoth 412,432 road traffic accidents. Tamilnadu, a state in the southern India where our hospital is located, recorded the highest number of road accidents in 2021 (55,680) among all the Indian states. This resulted in a greater number of open tibial fractures presented to the Emergency Department of hospitals across the state of Tamilnadu as tibia is the most common long bone fractured in humans and the least soft tissue coverage makes open fractures common in tibia. Hence it is needed to have an optimal and a cost-effective protocol to address these injuries. Though closed tibial fractures are commonly managed by internal fixation methods, there are no clear cut standard guidelines regarding management of open tibial fractures especially Type 3 injuries.
These fractures are generally managed by wound debridement and temporary stabilisation with AO external fixators followed by delayed internal fixation provided the soft tissue cover is adequate and there is no infection. The deep infection rate might be as high as 17 %, delayed union rate 14 % and the need for secondary bone grafting 17 % even if this protocol was followed [1]. Pin-site infection would preclude the use of intramedullary nail in tibial fractures following the use of AO external fixators [2]. There is a need to devise an optimal management protocol in the management of open tibial fractures so that the morbidity they cause decreases and the cost-effectiveness increases. This is more relevant in countries like ours where much of the healthcare costs are borne by the state and the chance of patients having adequate insurance cover is low. Hence this study aims at analysing the factors influencing the outcome of treatment of open tibial fractures using external fixation with Ilizarov ring fixators as definitive method using Tucker’s criteria [3].
METHODOLOGY
A total of 28 patients reported to the Emergency Department with open tibial fractures satisfying our inclusion criteria during the above mentioned study period. Three patients were lost for follow-up and so finally 25 patients were studied. ATLS protocol was followed in managing these patients. Open fractures were classified according to Gustilo-Anderson classification of open fractures [4]. Once the patients were hemodynamically stabilised and all the life threatening injuries were addressed radiological examination was carried out and skeletal stabilisation was done either with Ilizarov ring fixators primarily or with AO external fixators after thorough debridement of wounds. In those patients where AO external fixators were used initially, the fractures were revisited within five days and the Ilizarov ring fixator was applied. We followed accepted standards in applying Ilizarov ring fixators. We used a leg holder which we were able to construct using Italian arches, rings and threaded rods to keep the leg off the operation table which made the wires to be easily drilled though the bones and soft tissues (Fig. 1).

Fig. 1. Leg stand
After the fractures were stabilised with Ilizarov Ring Fixators, the patients were encouraged knee and ankle range of motion the next day of surgery. Patients were followed up first at 4 weeks after the definitive procedure, then at 6 weeks, 3 months, 6 months and at 1 year. Pin sites were cared and any pin-site infection was noted and classified according Checketts-Otterburn Classification [5] (Table 1). Partial weight-bearing was allowed once the wounds settled and progressed to full weight-bearing which depended on presence or absence of associated injuries and condition of the patient (Fig. 2). We considered removal of the fixator once the patient satisfied the clinical criteria of absence of pain at the fracture site at rest as well as on bearing weight with dynamization and radiological criteria of union evidenced by presence of bridging callus in at least three planes at the fracture site.
Table 1
Checketts-Otterburn classification of pin-site infections
|
Grades |
Characteristics of Infection |
Management |
|
Grade I* |
Slight discharge ,Redness around the pins (problem rather than infection) |
Improved pin-site care |
|
Grade II* |
Redness of the surrounding skin, pus at the pin site, pain and tenderness in the soft tissue |
Oral antibiotics, Improved pin-site care |
|
Grade III* |
Similar To Grade-II but fail to settle with oral antibiotics and improved pin site care |
The affected pin or pins are re-sited and external fixation can be continued |
|
Grade IV# |
Severe soft tissue infection involving several pins, sometimes with associated loosening of the pins |
External fixation should be abandoned |
|
Grade V# |
In addition to the soft tissue infection, in Grade V infections there is involvement of the bone. Radiographs will show areas of osteolysis and possibly sequestrum formation |
External fixation should be abandoned |
|
Grade VI# |
These infections occur after fixator removal. The pin track heals initially, but will subsequently break down and discharge at intervals. Radiographs shows new bone formation and sometimes sequestra |
Curettage of pin track |
* — minor infections; # — major infections.

Fig. 2. Weight-bearing measure
RESULTS
Twenty-five patients that fulfilled the inclusion criteria were included in our study, of which 22 patients (88 %) were males and only 3 patients (12 %) were females. Most of the patients were in their fourth decade of their age (48 %). The commonest mode of injury was road traffic accidents involving motorcycles (52 %) because most of the working class population in this part of the world generally use motorcycles for their daily commuting. In 72 % of the patients, the right leg was injured and in 22 patients (88 %) both tibia and fibula were fractured and only in 3 patients (12 %) we encountered an isolated tibia fracture. According to Gustilo – Anderson classification we had 13 Type 3A injuries (52 %), 5 Type 3B injuries (20 %), 6 Type 2 injuries (24 %) and only one Type 1 injury (4 %). We didn’t encounter Type 3C injuries in our study. Of these 25 patients, only two had intra-articular fractures (8 %). In our study 18 patients (72 %) had communited fractures and others were simple fractures. By AO classification of fractures, a majority fell under 42 C 1 (15 %), 42 C 2 (11 %) and 42 C 3 (11 %). Of these 25 patients, in 19 patients the fractures were stabilized temporarily with AO external fixators. This was to achieve hemodynamic stability, to address other injuries in the same patient and to plan for definitive management. In remaining 6 patients, Ilizarov ring fixators were used primarily. Of the 19 patients where AO external fixators had been used initially, the ring fixator was applied in 12 patients on the third day since injury and in 7 patients on the fourth day since injury. Thus, in all the 25 patients the ring fixator was applied within 5 days after injury. In 10 patients we had pin-site infections (Fig. 3, Table 2) which were managed appropriately and during the course of management pin removal and insertion at a different position was needed in 52 % of the fractures for want of flap cover. All patients were able to flex the knee up to 90 degrees as beyond that point the proximal most rings hindered any further movement (Fig. 4). One patient (4 %) had equinus contracture at the ankle which was corrected with physical therapy. At 8 weeks, 18 patients were able to bear full weight on the injured limb. We noticed that with proper education and motivation patients tolerate the fixator and were willing to carry on their routine activities with the fixator (Fig. 5).
Table 2

Fig. 4. 90° flexion with fixator on
Fig. 3. Pin-site infection
Pin-Site Infections Managed
|
Grade |
I |
II |
III |
IV |
V |
VI |
|
Number of Pin-Site Infected |
2 |
5 |
3 |
Nil |
Nil |
Nil |
Fig. 5. Patient feels comfortable with fixator
We achieved union in all the 25 patients without infection (Table 3). In majority of patients (48 %), union occurred after 24 weeks. The signs of clinical union appeared 4 weeks earlier than radiological union. We considered the probability of delayed union when no signs of union were noted radiologically even after 24 weeks since injury. This situation happened in 5 patients, and in 2 patients where diaphyseal fracture site non-union occurred, we did bone grafting following the standard procedure. Two patients needed bone marrow injection alone in metaphyseal fracture non-union. In one patient, we did excision of the non-union and carried out bone transport after corticotomy at the proximal tibia (Fig. 6). All these 5 fractures united after 48 weeks. We had no non-union or residual/deep infection at the end of 1 year follow-up period but two cases of limb shortening, one had 2.0-cm shortening and the other had 1.5-cm shortening. These were managed with shoe-rise alone and no additional procedure was required. We considered fixator removal once the fracture showed signs of union clinically and radiologically. We removed the fixator at the end of 24 weeks in 12 patients (48 %), 32 weeks in 8 patients (32 %) and 48 weeks in 5 patients (20 %) (Fig. 7–9).
Table 3
Period of Bony Union
|
S.No. |
Period For Union |
Noof Fractures |
Percentage |
|
1 |
< 4 weeks |
0 |
0 % |
|
2 |
4 weeks – 6 weeks |
1 |
4 % |
|
3 |
6 weeks – 3 months |
7 |
28 % |
|
4 |
3 months – 6 months |
12 |
48 % |
|
5 |
6 months – 1 year |
5 |
20 % |
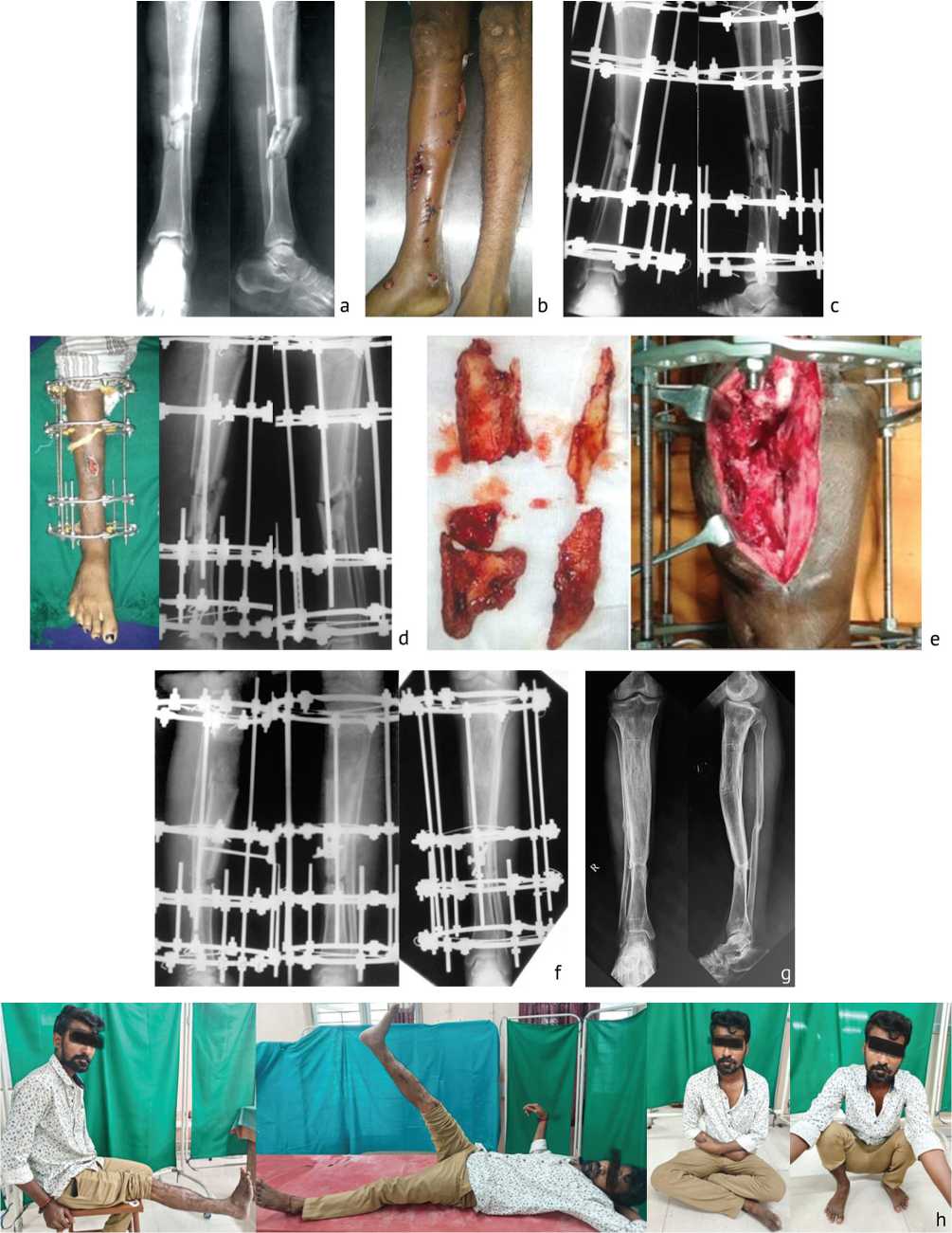
Fig. 6. Patient 1: a — segmental communited fracture, day 1; b — condition of the skin at presentation; c — definitive Ilizarov fixation of the fracture; d — patient at 10 weeks — wound open, no signs of union; e — resection of nonunion segment; f — corticotomy, distraction, consolidation; g — X-rays AP and lateral views post-fixator removal (well united and consolidated); h — clinical outcome — patient is comfortable in sitting cross-legged and squatting

Fig. 7. Patient 2 with communited proximal left tibia fracture: a — X ray AP and lateral views; b — post-operative X rays (from left to right — 1st month AP view;1st month lateral view; 3rd month AP view; 3rd month lateral view; 6th month AP view; 6th month lateral view); c — X ray and photo of the patient after 8 months (patient could squat and sit cross-legged)
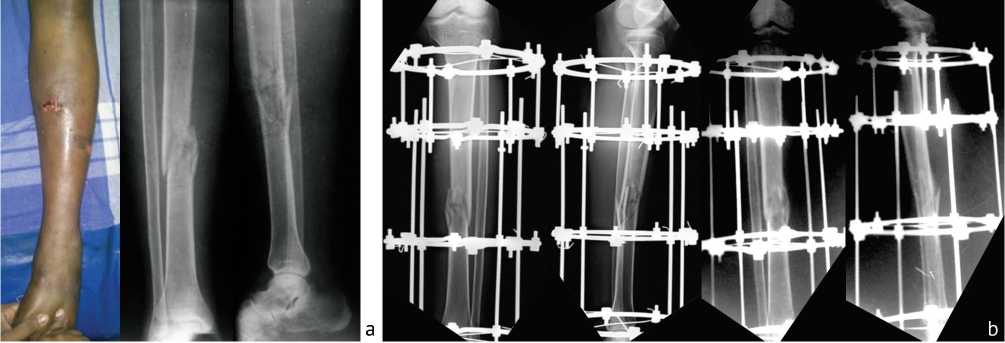
Fig. 8. Patient 3: Type 3A open injury: a — fracture in middle third of both left lower leg bones (please note the tense left leg with open wound); b — postoperative X Rays (from left to right — AP 6 weeks, lateral 6 weeks, AP 6 months lateral 6 months); c — post-operative X Rays and photos of the patient at 10 months after fixator removal. He was able to squat and sit cross-legged

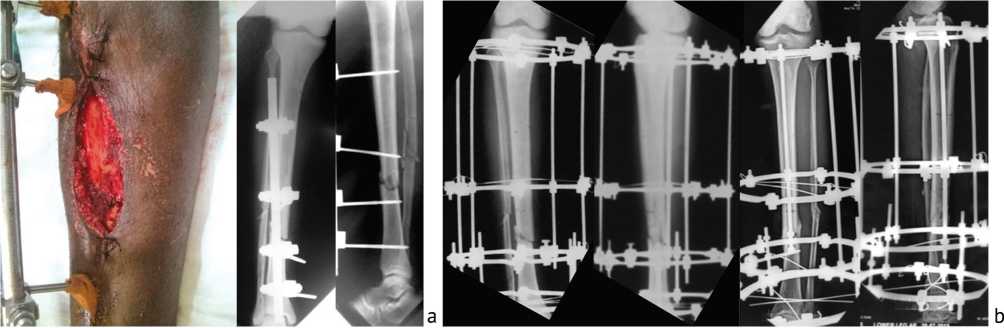

Fig. 9. Patient 4: a — Type 3B, open fracture-wound debridement and AO external fixator application; b — X Rays (from left to right — day 4 after injury AP and lateral views, 6 months after fixation AP and lateral views); c — patient was comfortable and working his gym routine
The functional outcome was studied using Tucker’s Criteria (Box 1) according to which 5 patients (20 %) had excellent outcome, 9 patients (33 %) had good outcome, 8 patients (29 %) had fair outcome and 3 (16 %) had poor outcome (Table 4).
Box 1Tucker’s Criteria
Excellent : Fracture union plus full knee extension with 125° knee flexion and 75 % of ankle motion when compared to normal side(if both sides are involved ankle motion above neutral with 30° flexion, no limb length discrepancy greater than 1 cm, angulation not greater than 7° in any plane, rotation not greater than 15° and no infection.
Good : Fracture union with one criteria missing
Fair : Fracture union with two criteria missing
Poor : Fracture union with three criteria missing
Table 4
Functional Outcome using Tucker’s Criteria
|
S. No |
Outcome |
No of cases |
Percentage |
|
1 |
Excellent |
5 |
20.52 % |
|
2 |
Good |
9 |
33.33 % |
|
3 |
Fair |
8 |
29.63 % |
|
4 |
Poor |
3 |
16.52 % |
DISCUSSION
The development of highways along with availability of high performance motor vehicles and rapidly increasing number of motor cycle users with general lack of awareness about road rules result in high velocity injuries in fast developing nations like India. Most of the available literature on open tibial fractures reveals a male preponderance in the age group of 30–40 years similar to our study [6, 7, 8, 9]. In general, the mainstay of management of open fractures is thorough debridement the principles of which were laid by Desault and Larry [10, 11] which are still relevant today. We did thorough debridement of all the wounds before stabilising the fractures regardless of whether we used AO or ring fixators primarily. A general protocol that is followed across many centres in management of open tibial fractures is thorough debridement, early antibiotics (within 1–3 hours since injury), hemodynamic stabilisation, primary internal fixation with intramedullary nails or temporary stabilisation with AO external fixators followed by secondary internal fixation with intramedullary nailing [12, 13, 14]. Complications like deep infection, delayed union and need for bone grafting is high even if this regimen is followed strictly [1]. Plate fixation in open tibial fractures did not yield favourable results in the past [15]. Limb Reconstruction System (LRS) was studied in open tibial fractures. M.Y. Patil et al. studied 54 patients with Type 3A and Type 3B open tibial fractures who were managed with LRS and stated that LRS was a simple and easy system which could be used for all open tibial fractures but cautioned that their study was limited as it did not have a control group [16]. In our view the LRS, though offers stability and provision of bone transport, is costly and not versatile as it would be difficult with LRS to achieve compression of fracture fragments in comminuted fractures. These would be possible with the Ilizarov ring fixator using drop wires and posts. The Ilizarov ring fixator shows optimal biomechanical properties such as low axial stiffness on axial loading and high axial stiffness to bending loading which promote bone healing [17]. It has axial elasticity and is inherently dynamic. Conventional large pin fixators and LRS could be dynamized but jamming of telescopic rods is often a problem since they are not inherently dynamic. Not many studies are there regarding the use of Ilizarov ring fixators in definitive management of open tibial fractures. N. Wani et al. in their study of 60 patients with Type 2, Type 3A and Type 3B open fractures of the tibia concluded that the Ilizarov external fixator could be recommended as primary modality of fixation in open tibial fractures despite technical difficulties and possible of pin-site infection [18]. The most common complication in their study was pin site-infection (32 patients). We had pin site-infection in 10 patients that were managed appropriately.
The principle of distraction histogenesis could be used to treat soft tissue defects simultaneously while addressing the bone problem. In their series of 34 patients with open tibial fractures treated primarily and definitively with the Ilizarov ring fixator, G. Hosny and M. Fadel used soft tissue distraction system successfully in four patients [19]. In open tibial fractures without bone loss or infection its advantages are less tissue trauma and minimal or no surgical bleeding unlike with the use of internal fixation methods. The Ilizarov method allows the surgeon to treat bone loss and infection simultaneously [20]. In the presence of diaphyseal bone defect with infection the Ilizarov method offers good results [21]. Fortunately, in our study we did not have infected diaphyseal bone defects. Bone defects might be treated with alternative methods like vascularised fibular grafts, free fibular transfers or Papineau technique [22, 23] but these methods need prolonged pre-and post-procedure antibiotic therapy, no mechanism to correct deformities and do not allow the patient to bear weight during treatment. Even though bony union might be achieved by alternative methods, the bone that is formed needs years of remodelling to get the biomechanical structure and radiological appearance as that one formed by bone transport using Ilizarov distraction histogenesis. In our series we had one patient who needed a corticotomy and bone transport to achieve bone union. The mean time of bone union ranged from 21 weeks to 34 weeks in most of the series [18, 19, 20, 21] which is comparable to the present study.
Limitation of the present study is the absence of a comparison group, though it was possible because of the nature of the injuries that the patients had while arriving at the trauma care facility. Another limitation is the follow-up period, we followed the patients for one year but if we followed the patents for longer periods we could have assessed the long-term prognosis.
CONCLUSION
The definitive treatment of open tibial fractures especially Type 3B fractures with the Ilizarov Ring Fixator system is found be optimal and cost-effective. The Ilizarov Ring Fixator is a versatile tool which allows the orthopaedic surgeon to treat fracture, infection and bone loss simultaneously. Since it is inherently dynamic, weight-bearing is possible even during the treatment period. It yields excellent and good results in the conditions where internal fixation methods would be counterproductive.
Conflicts of Interest None.
Funding None.


