First dorsal metacarpal artery flap in soft tissue reconstruction of recurrent thumb squamous cell carcinoma
Автор: Pauline Yap, Arman Zaharil Mat Saad, Wan Azman Wan Sulaiman, Siti Fatimah Noor Mat Johar, Nurul Syazana Mohamad Shah
Журнал: Сибирский онкологический журнал @siboncoj
Рубрика: Случай из клинической практики
Статья в выпуске: 3 т.22, 2023 года.
Бесплатный доступ
Background. Subungual squamous cell carcinoma (SCC) of thumb is a rare disease. However, it is the most common malignancy affecting the nail bed. Early recognition is crucial and important for prompt diagnosis and effective treatment. Often this tumour needs to be treated surgically with wide local resection, which results in a defect in the thumb. If not handled appropriately, such defects render restriction in functionality of the involved thumb as well as a poor aesthetic outcome. In the worst-case scenario, it may result in a poor function of involved hand. Thus, reconstruction of the involved thumb is necessary. The main aim of reconstruction is to regain the hands’ function and preserved the thumbs’ sensation. Secondarily, to have an aesthetically pleasing hand. Our hands carry out delegate job and important duty for daily function. Especially, the thumb working together with the other fingers to carry out the hand function as one unit. Loss of thumb function affects the whole performance of the hand. Case descriptions. We report a case of recurrent subungual squamous cell carcinoma of thumb, which had wide local resection and subsequently underwent soft tissue coverage with an islanded first dorsal metacarpal artery (FDMA) perforator flap. One month after surgery, the patient was able to regain a good functional outcome of the hand. In this report, we discussed the procedures that had been done. Conclusion. The patient regained full functional hand after reconstruction with preserved sensation over distal thumb. The aesthetic outcome is satisfactory. The FDMA perforator flap is a very pliable and robust flap for reconstruction of distal thumb defect.
Surgical flap, thumb, squamous cell carcinoma, perforator flap, nail diseases
Короткий адрес: https://sciup.org/140300177
IDR: 140300177 | УДК: 616.717.91-006.61-036.65-089 | DOI: 10.21294/1814-4861-2023-22-3-162-167
Текст научной статьи First dorsal metacarpal artery flap in soft tissue reconstruction of recurrent thumb squamous cell carcinoma
Squamous cell carcinoma (SCC) of the nail bed is considered a rare disease even though subungal SCC is the most common malignancy affecting the nail bed [1]. It is more likely found in men than in women especially at the age of 50s [2]. First dorsal metacarpal artery (FDMA) perforator flap was first described by Hilgenfeldt in 1950 and redefined by Holevich in 1963 [3–5]. It was popularized by Lie and Posch but then Foucher included neural structures into the flap and named it as a kite flap. Thus, it is also called Foucher's flap [3]. It is based on the neurovascular structure of first dorsal metacarpal artery (FDMA), venae comitantes or larger subcutaneous vein and superficial radial nerve.
Case report
A 62-year-old gentleman who had left thumb squamous cell carcinoma (SCC) diagnosed 2 years ago. Initially started as a small subungual lesion which extended to the tip of left thumb. The lesion was painful and had contact bleeding. He underwent first surgery for excisional biopsy and removal of nail in another tertiary centre. Unfortunately, the histopathological result reported as SCC. He did not undergo adjuvant therapy. The lesion recurred 4-months after surgery. He was referred to our centre for further management. On assessment, there was a small subungual lesion size of 1.0×0.5 cm at the nail bed. The pulp of the thumb was normal. MRI showed no evidence of local bone involvement. Subsequently, he had wide local excision and soft tissue coverage with islanded first dorsal metacarpal artery fasciocutaneous flap. The surgery was successful, the flap was healthy prior to discharge. He was seen in our clinic 1-month after surgery and the flap was healthy. Range of motion of thumb was normal and sensation was intact. Full thickness skin graft (FTSG) was fully taken well on the index finger.
He underwent wide local excision of the left thumb. The entire nailbed was excised together with dorsal bony part of distal phalanx. There was a defect size of 2.5×2.5 cm at the tip of the left thumb. The wound bed had exposed bone over distal phalanx (Fig. 1). Intraoperatively, course of the first dorsal metacarpal artery was traced with doppler device and marked. Subsequently, the islanded skin of the first dorsal metacarpal artery flap with rectangular shaped 4×2 cm was designed (Fig. 2). Posterior to the islanded skin, curvilinear incision marking was made continued from the proximal part of the islanded skin flap bordering

Fig. 1. Initial defect. Left thumb defect size of 2.5×2.5 cm with exposed part of the bony distal phalanx
Рис. 1. Исходный дефект большого пальца левой руки, размером 2,5× 2,5 см, с обнаженной костью дистальной фаланги

Fig. 2. The flap design and course of the first dorsal metacarpal artery. The skin flap size of 4×2cm rectangular shape was designed. The FDMA traced with doppler ultrasound and marked Рис. 2. Разметка кожного лоскута прямоугольной формы, размером 4×2 см. Первая тыльная пястная артерия промаркирована с помощью ультразвуковой допплерографии
the FMDA pedicle along the 2nd metacarpal bone to the first web space (Fig. 2). The islanded skin flap was raised from distally in a plane superficial to the paratenon to ensure good graft bed (Fig. 3).
Proximal to the islanded flap, an incision is made along the skin marking along the second metacarpal bone. The first interosseous muscle fascia is incised, the intermuscular septum was preserved and the fasciocutaneous flap was raised. The skin along the pedicle was not de-epithelized. The superficial radial nerve was identified and preserved (Fig. 4). Around 1 cm of subcutaneous tissue is left surrounding the pedicle to carefully not to injure the pedicle. A curvilinear skin incision was made at the proximal part of the defect at the thumb up to the first webspace in a subcutaneous plane creating a space for the FDMA pedicle as the skin over the pedicle was preserved. The flap then was rotated and transposed to the thumb’s defect (Fig. 5).
Secondary defect of the donor site was covered with thin layer of full thickness skin graft (FTSG) harvested from the left inner arm. A cast was placed on the volar surface of the hand to limit flexion and abduction of the thumb to avoid compression and straining of the pedicle. The surgery was successful, the flap was healthy prior to discharge. He was seen in our clinic 1-month after surgery. The flap was healthy. Range of
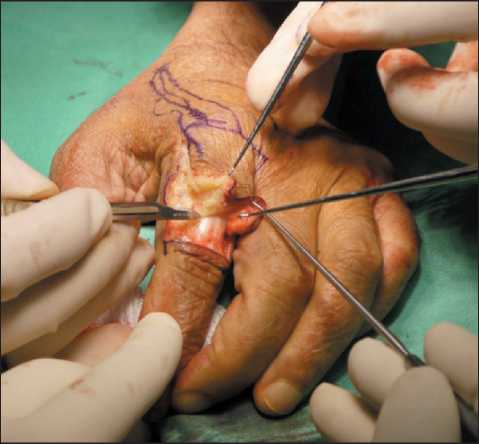
Fig. 3. Paratenon preserved for better graft bed Рис. 3. Паратенон сохранен для лучшего приживления лоскута

Fig. 4. The fasciocutaneous flap was raised up to subfascial layer. The skin over the pedicle was preserved. The superficial radial nerve was identified and preserved. Pedicle is traced proximally to facilitate good arc of rotation
Рис. 4. Кожно-фасциальный лоскут поднят до субфасциального слоя. Кожа над ножкой сохранена. Поверхностный лучевой нерв идентифицирован и сохранен. Ножка прослеживается проксимально, что обеспечивает адекватной поворот лоскута

Fig.5. A curvilinear skin incision was made at the proximal part of the defect at the thumb up to the first webspace in a subcutaneous plane creating a space for the FDMA pedicle as the skin over the pedicle was not de-epithelized. The flap then was transposed to the left thumb
Рис. 5. Криволинейный разрез кожи в проксимальной части большого пальца с созданием подкожного тоннеля для ножки лоскута, включающей первую дорсальную пястную артерию.
Затем лоскут был перенесен на большой палец левой руки

Fig. 6. 1-month after surgery. Good functional outcome and aesthetic appearance of thumb achieved and secondary defect well healed.
Рис. 6. Через 1 мес после операции достигнут хороший функциональный результат и эстетический вид большого пальца
motion of thumb was normal and the sensation was intact. FTSG was fully taken well on the index finger (Fig. 6). Aesthetic appearance is satisfactory.
Discussion
Our thumb contributes 40 % of the hand function. Generally, the aim of thumb reconstruction is to restore adequate length for opposition, mobility and stability for opposition, flexion and pinch, sensibility for protective function and adequate dexterity, and its aesthetics. Other than that, providing adequate and durable soft-tissue coverage is very important in thumb reconstruction. However, it is rather difficult to achieve all of these. Therefore, the priority is to restore its function. It is very important because without adequate functional restoration and sensation of thumb, our hand will not be able to provide tripod pinch, fine motor dexterity and cylinder grasp.
The options of thumb reconstruction depend on the size of defect and zone of the defect and any bony part exposed. Small defect of thumb less than 1 cm2 without any bony exposure usually can be healed by secondary intention. This can preserve sensation of the thumb and omit donor site morbidity. However, prolonged wound care would be needed and may be painful. Full thickness skin grafts from the hypothenar eminence, wrist or groin crease could be an option for small defects without any bony exposure. However, skin graft would be insensate.
Larger defects more than 2 cm2 with loss of volar pad, exposed bony component and tendon may need vascularized coverage. Commonly, these defects could be reconstructed with Moberg flap. However, this flap may require up to 45 degrees of interphalangeal joint flexion to obtain coverage and tendency to develop a complication of long-term flexion contracture and joint stiffness [6]. Defect of more than 2.5 cm2 could be covered using heterodigital flaps for instance, crossfinger flap and FDMA flap. Cross-finger flap is a good choice especially for defects involving the whole palmar surface of the thumb distal to the interphalangeal joint. Littler neurovascular island flap is commonly used in reconstruction of the thumb pulp.
Recently it has become increasingly popular of using Quaba flap in reconstruction of defects on the dorsum of the hand. This technique was based on Quaba perforator which is a perforator of dorsal communicating branch of the common digital artery and the dorsal metacarpal artery [7]. The difference between FDMA flap from Quaba flap is that Quaba flap utilized Quaba perforator as a pivot point and its flaps pedicle while FDMA flap included Quaba perforator in its main pedicle. Quaba flap is also a versatile flap. It can be based on antegrade circulation from the DMA or retrograde from the palmar system or digital artery. This flap had been reported to be used in reconstruction over the dorsal hand defect and the web space defect [7, 8]. This flap could be possible in use of reconstruction of the proximal dorsal part of the thumb. However, it has not been reported.
It would be difficult to reach the distal part of the thumb due to the limited arch of rotation created by the distance between the Quaba perforator and first web space before reaching the distal thumb. Though, there were successful cases of thumb reconstruction using perforator flap based on the princeps pollicis artery [9]. But, the findings on the outcome of this technique were limited. More studies should be done on techniques of reconstruction of thumb in order to compare the superiority in functionality and cosmesis of these techniques.
In our case, the patient had a defect distal to the interphalangeal joint with exposure of bony structure. Our main goal of reconstruction was to restore the soft tissue coverage and maintain the length of the thumb. Thumb defect distal to the interphalangeal joint would not cause any functional deficit as the interphalangeal joint is functional, thus rarely need length restoration [10]. The exposed bony phalangeal bone would not take a graft. Therefore, we need vascularized coverage in this case. We have chosen FDMA flap because the defect was mainly over the dorsal aspect of the distal thumb and this was a sensate flap. FDMA flap donor site was on the dorsal aspect of the index finger thus it was the most suitable for the ease of transposition and rotation.
FDMA flap had a major advantage as the secondary defect virtually did not result in functional loss. The vascular pedicle was not skeletonized to preserve the vena comitantes and ensure good venous outflow. We have decided to make an incision connecting the defect to the donor site to minimize venous congestion of the flap over tunnelling. This technique minimized the injury to the pedicle and flap congestion. The functional outcome of soft tissue coverage was very good in our patient. The patient was satisfied with the functional and aesthetic outcome of the surgery. A recent study also has shown the outcome of thumb reconstruction using FDMA island flap was good, with an average static two-point discrimination test of 10.4 mm and complete cortical reorientation in 40 % of cases. The incomplete reorientation in the remaining patients did not interfere with their normal daily activities [5, 11]. Previous studies had proven that it provides excellent functional and aesthetic outcome, moreover, render minimal donor site morbidity [11, 12]. We concluded that FDMA flap is a good choice for reconstruction of thumb defect. It offers sensate, pliable and versatile coverage for small to moderate sized defects of a thumb’s defect.
Conclusion
FDMA flap offers a versatile, sensate and pliable coverage for reconstruction of thumb defect. Moreover, it also provides good functional and aesthetic outcome. Reconstructive surgeon shall consider FDMA flap into an option for reconstruction of especially dorsal thumb defect.
Список литературы First dorsal metacarpal artery flap in soft tissue reconstruction of recurrent thumb squamous cell carcinoma
- Sever C., Kulaci Y., Oksuz S. Subungual squamous cell carcinoma masquerading as an onychomycosis. J Clin Anal Med 2012; 3(2): 231-3.
- Inkaya E., Sayit E., Sayit A.T., Zan E., Bakirtas M. Subungual squamous cell carcinoma of the third finger with radiologic and histopathologic findings: A report of case. J Hand Microsurg 2015; 7(1): 194-8.
- Small J.O., Brennen M.D. The first dorsal metacarpal artery neurovascular island flap. J Hand Surg Br. 1988; 13(2): 136-45. https://doi.org/10.1016/0266-7681_88_90122-2.
- Germann G., Palm-Broking K. First dorsal metacarpal artery island flap. Master Techniques in Orthopaedic Surgery: Soft Tissue Surgery. 2008; 277-88.
- Prabhu M., Powar R., Sulhyan S.R. FDMA Flap: A Versatile Technique to Reconstruct the Thumb. Int J Pharma Med Biol Sci. 2013; 2(4): 8-14.
- Heitmann C., Levin L.S. Alternatives to thumb replantation. Plast Reconstr Surg. 2002; 110(6): 1492-503; quiz 1504-5. https://doi.org/10.1097/01.PRS.0000029362.01985.80.
- Bailey S.H., Andry D., Saint-Cyr M. The dorsal metacarpal artery perforator flap: a case report utilizing a quaba flap harvested from a previously skin-grafted area for dorsal 5th digit coverage. Hand (NY). 2010; 5(3): 322-5. https://doi.org/10.1007/s11552-009-9254-z.
- Perera N.K., Rozen W.M., Niumsawatt V., Ek E.W. First Web Space Reconstruction Using a Dorsal Metacarpal Artery Perforator Flap: A Further Application of the Quaba Flap. Plast Reconstr Surg. 2014; 133(1): 74-6. https://doi.org/10.1097/01.prs.0000436804.58165.9a.
- Hou C., Chang S., Lin J., Song D. Digital Artery Perforator Flap. Surgical Atlas of Perforator Flaps. 2015; 103-22. https://doi.org/10.1007/978-94-017-9834-1_16.
- Muzaffar A.R., Chao J.J., Friedrich J.B. Posttraumatic thumb reconstruction. Plast Reconstr Surg. 2005; 116(5): 103-22. https://doi.org/10.1097/01.prs.0000182650.17230.2a. Erratum in: Plast Reconstr Surg. 2006; 117(1): 349.
- Ghoraba S.M., Mahmoud W.H. Outcome of Thumb Reconstruction Using the First Dorsal Metacarpal Artery Island Flap. World J Plast Surg. 2018; 7(2): 151-8.
- Muyldermans T., Hierner R. First dorsal metacarpal artery flap for thumb reconstruction: a retrospective clinical study. Strategies Trauma Limb Reconstr. 2009; 4(1): 27-33. https://doi.org/10.1007/s11751-009-0056-1.


