PCI VS CABG for patients with CTO: contemporary techniques and outcome-single center experience
Автор: Abbas W., Zarif B., Azmy A.
Журнал: Cardiometry @cardiometry
Рубрика: Report
Статья в выпуске: 22, 2022 года.
Бесплатный доступ
CTOs are common findings on coronary arteriograms [1]. CTOs were defined as 100% coronary occlusion present for at least three months and found in almost 20% of all angiograms of patients with angina. The choice of therapy for patients undergoing coronary angiography and found to have CTOs was studied in The Canadian Multicenter Chronic Total Occlusions Registry [2]. Almost half the patients with CTOs were treated medically, and 25% underwent CABG (CTOs bypassed in 88%). PCI was performed in 30%, with a 70% success rate. While more patients with CTOs have historically been treated with CABG than PCI, technical advancements in PCI of CTOs may be expected to drive more patients with CTOs towards being treated with PCI [3].
Pci, cabg, cto, coronary arteriogram
Короткий адрес: https://sciup.org/148324412
IDR: 148324412 | DOI: 10.18137/cardiometry.2022.22.121127
Текст научной статьи PCI VS CABG for patients with CTO: contemporary techniques and outcome-single center experience
Imprint
Walid Abbas, Bassem Zarif, Ahmed Azmy. PCI VS CABG for patients with cto: contemporary techniques and outcome-single center experience. Cardiometry; Issue 22; May 2022; p. 121-127; DOI: 10.18137/cardiometry.2022.22.121127; Available from:
The literature reveals that CTOs are more often treated with CABG than PCI [4]. This has been recently confirmed in the SYNTAX registry and trial [5]. However, the literature on the surgical outcome of CTO’s is quite limited. CABG is a treatment for angina, and while limited, the published data suggest that CABG for CTOs reduces angina. However, the only randomized trial data is from a small subgroup in SYNTAX, finding more successful CTO revascularization with CABG than PCI. Non-randomized data from SYNTAX also show that CTO patients with complete revascularization have fewer events than patients with incomplete revascularization.
Patients and methods
Study Design and Patient Data
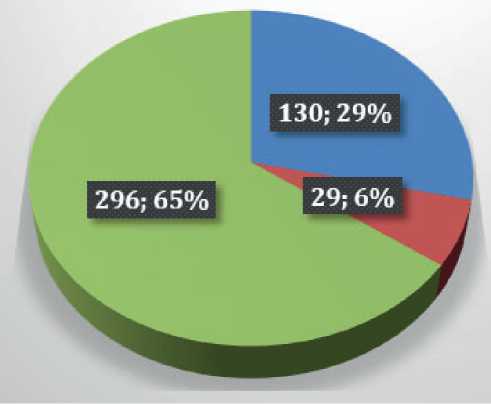
This retrospective cohort study was coted between Dec 2016 till Dec 2019; the heart team diagnosed 455 patients CTO. The studied groups of patients included left anterior descending occluded according to CTO criteria; those patients were 159 patients. Some of them were deemed surgical candidates based on risk stratification (EUROSCORE) and accepted for surgical coronary revascularization, others who were still symptomatic were offered CTO/PCI, and the rest received guidelines directed medical therapy; all patients who were selected for this study were evaluated based on SYNTAX and EUROSCORE
All preoperative, in-hospital, and post-discharge data were collected from the medical records. Definitions were obtained from STS definitions; for example, a Recent myocardial infarction was defined as a myocardial infarction that occurred 1 to 7 days before surgery. Old myocardial infarction was described as a myocardial infarction that occurred more than seven days before surgery. Perioperative myocardial infarction (PMI) was defined as new electrocardiographic or echocardiographic changes with creatine kinase MB more than 100 ng/ml.
The Institutional Review approved this study. Board National Heart Institute, consent was waived.
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics 23 software (IBM Corp, Armonk, NY). Normally distributed continuous variables are expressed as the mean _ SD, and skewed continuous variables are defined as the median with the range. Non-parametric variables are expressed as frequencies and percentages. Differences with p values of less than .05 were considered statistically significant.
Results
Retrospective observational At NHI between December 2016-December 2019. Including 159 patients
Issue 22. May 2022 | Cardiometry | 121
with CTO and CCS. The decision for revascularization was as per the heart team’s decision after reviewing patient characteristics, risk factors, anatomical complexity, and surgical risk. 130 patients were advised for CABG, and 29 for PCI-CTO.
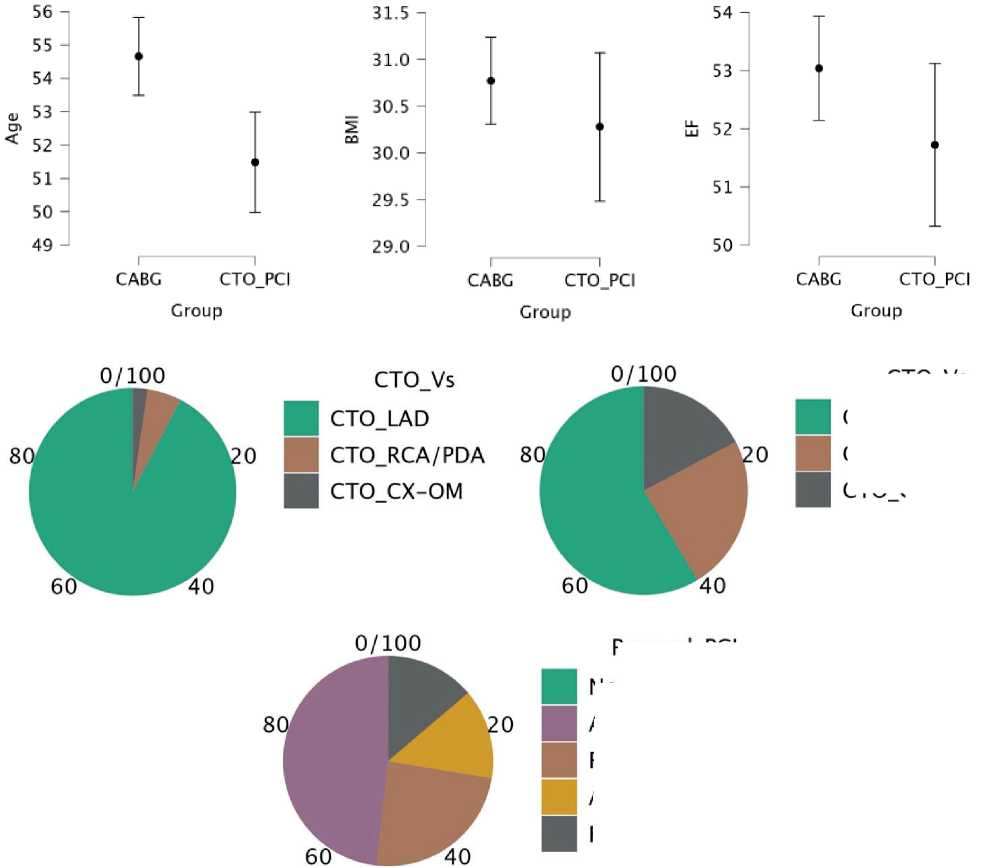
Patients’ characteristics
The preoperative characteristics of the studied groups showed non-significant differences in the prevalence of Diabetes Miletus, Hypertension, Dyslipidemia, COPD, Cerebrovascular disease, Renal Impairment, Peripheral vascular disease, While the differences were significant regarding the prevalence of smoking and heart failure among both groups. These data are illustrated in table (1).
|
Group |
ChiSquare |
Sig |
|||
|
CABG |
CTO_ PCI |
||||
|
Count |
Count |
||||
|
DM |
No |
66 |
10 |
0.112 |
0.15 |
|
Yes |
64 |
19 |
|||
|
HT |
No |
84 |
22 |
0.245 |
0.28 |
|
Yes |
46 |
7 |
|||
|
Dyslipidemia |
No |
54 |
10 |
0.483 |
0.53 |
|
Yes |
76 |
19 |
|||
|
Smoking |
No |
81 |
24 |
0.035 |
0.04 |
|
Yes |
49 |
5 |
|||
|
COPD |
No |
98 |
26 |
0.093 |
0.13 |
|
Yes |
32 |
3 |
|||
|
cerebrovascular disease |
No |
125 |
27 |
0.469 |
0.61 |
|
Yes |
5 |
2 |
|||
|
Renal_Imp |
No |
126 |
27 |
0.329 |
0.3 |
|
Yes |
4 |
2 |
|||
|
HF |
No |
128 |
26 |
0.014 |
0.04 |
|
Yes |
2 |
3 |
|||
|
Peripheral_VD |
No |
125 |
27 |
0.469 |
0.61 |
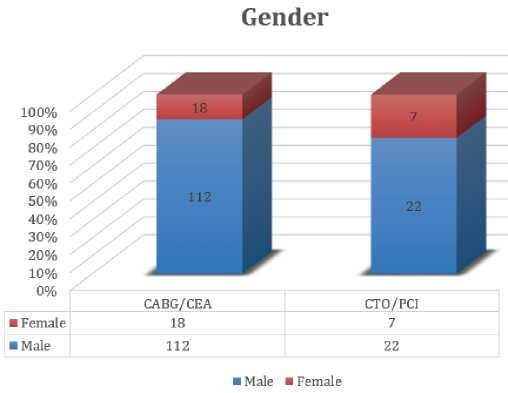
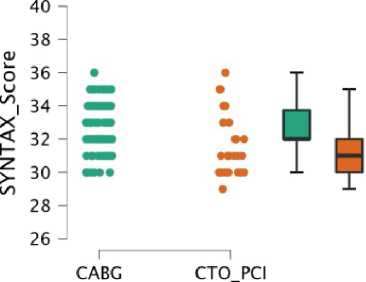
Mean age for CABG group 54.6 ± 6.8 years. CABG group 86% males, 49% diabetic, 64% hypertensive, 37% smokers, BMI for CABG was 30.7 ± 2.7, 24% COPD, 3.8% has a history of CVA, 3% has CKD, 1.5% has a history of HF, EF in CABG was 53.03 ±5.19%, 3.8% has PAD. 78.4% have angina CCS 3ormore. 12% has the previous PCI. 57% has moderate syntax, 43% has high syntax. 7.6% have LM disease. 77% has 3VD. 92.3% has a single CTO, 5.4% has 2-vessels CTO, 2.3% has a 3-ves-sel CTO. The target vessel in CABG was LAD in 92%, RCA 5.3%, LCX 2.3%. The average CCS anginal class before CABG was 2.8 ±0.45. Mean SYNTAX in CABG was 32.5 ±1.3. Mean EURO score for CABG 2.69 ±0.8. CTO segment length in CBAG 4.003 ±0.78
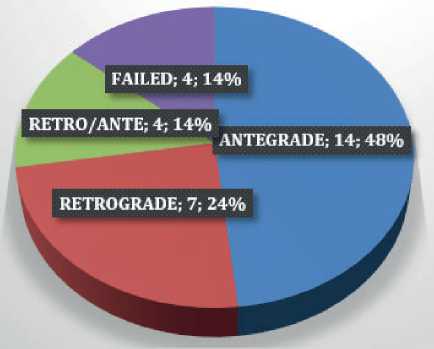
The average age in PCI-CTO was 51.4 ± 4.1 years. 75.8% males, 65% diabetic, 24% hypertensive, 17% smokers, BMI for PCI was 30.2 ±2.1, 10% COPD, 6.8 % has a history of CVA, 6.8% has CKD, 10.3% has a history of HF, EF in PCI was 51.7 ± 3.8%, 6.8has s PAD. 62% has CCS angina 3 or more. 31% have the previous PCI. 76% has moderate syntax, 24% has high syntax. 6.8% have LM disease. 48.2% has 3VD. 58.6% has single CTO, 24%.1 % has 2 CTOs, 17.2% has 3 CTOs. Target vessel was LAD in 58.6%, RCA 24.1%, LCX in 17.2%. Average CCS angina before PCI class was 2.6 ±0.49, Mean SYNTAX in PCI 31.4 ±1.8
Mean EURO score for PCI 3.7 ±0.67, CTO segment in PCI 2.56 ±0.52, Antegrade 48%, Retrograde 24%, combined 13%, failed in 13%.
|
t |
df |
p |
Mean Difference |
SE Difference |
|
|
Sex |
-1.376 |
157 |
0.171ᵃ |
-0.103 |
0.075 |
|
BMI |
0.914 |
157 |
0.362 |
0.492 |
0.538 |
|
DM |
-1.590 |
157 |
0.114ᵃ |
-0.163 |
0.102 |
|
HTN |
1.159 |
157 |
0.248ᵃ |
0.112 |
0.097 |
|
Dyslipidemia |
-0.697 |
157 |
0.487 |
-0.071 |
0.101 |
|
Smoking |
2.119 |
157 |
0.036ᵃ |
0.205 |
0.097 |
|
COPD |
1.681 |
157 |
0.095ᵃ |
0.143 |
0.085 |
|
Cerebrovascular |
-0.721 |
157 |
0.472 |
-0.031 |
0.042 |
|
CKD |
-0.973 |
157 |
0.332 |
-0.038 |
0.039 |
|
HF |
-2.489 |
157 |
0.014ᵃ |
-0.088 |
0.035 |
|
PAD |
-0.721 |
157 |
0.472 |
-0.031 |
0.042 |
|
Angina_Cl |
1.986 |
157 |
0.049ᵃ |
0.187 |
0.094 |
|
EF |
1.286 |
157 |
0.200ᵃ |
1.314 |
1.022 |
|
Prev_PCI |
-2.540 |
157 |
0.012ᵃ |
-0.187 |
0.074 |
|
SYNTAX category |
1.895 |
157 |
0.060ᵃ |
0.189 |
0.100 |
|
SYNTAX_Score |
3.706 |
157 |
< .001ᵃ |
1.082 |
0.292 |
|
EUROSCORE |
-6.234 |
157 |
< .001 |
-1.034 |
0.166 |
|
LM |
0.146 |
157 |
0.884 |
0.008 |
0.055 |
|
3VD |
3.174 |
157 |
0.002ᵃ |
0.286 |
0.090 |
|
CTO_Length |
9.339 |
157 |
< .001ᵃ |
1.434 |
0.154 |
|
CTO_Vs |
-5.033 |
157 |
< .001ᵃ |
-0.486 |
0.097 |
|
Group Statistics |
|||||
|
Group |
N |
Mean |
Std. Deviation |
Sig. (2-tailed) |
|
|
SYNTAX_ Score |
CABG |
130 |
32.53 |
1.31 |
0.0050 |
|
CTO_PCI |
29 |
31.45 |
1.84 |
||
|
EURO SCORE |
CABG |
130 |
2.69 |
0.83 |
0.0001 |
|
CTO_PCI |
29 |
3.72 |
0.68 |
||
Hospital Course
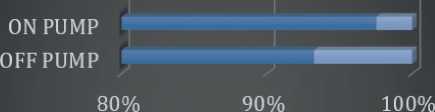
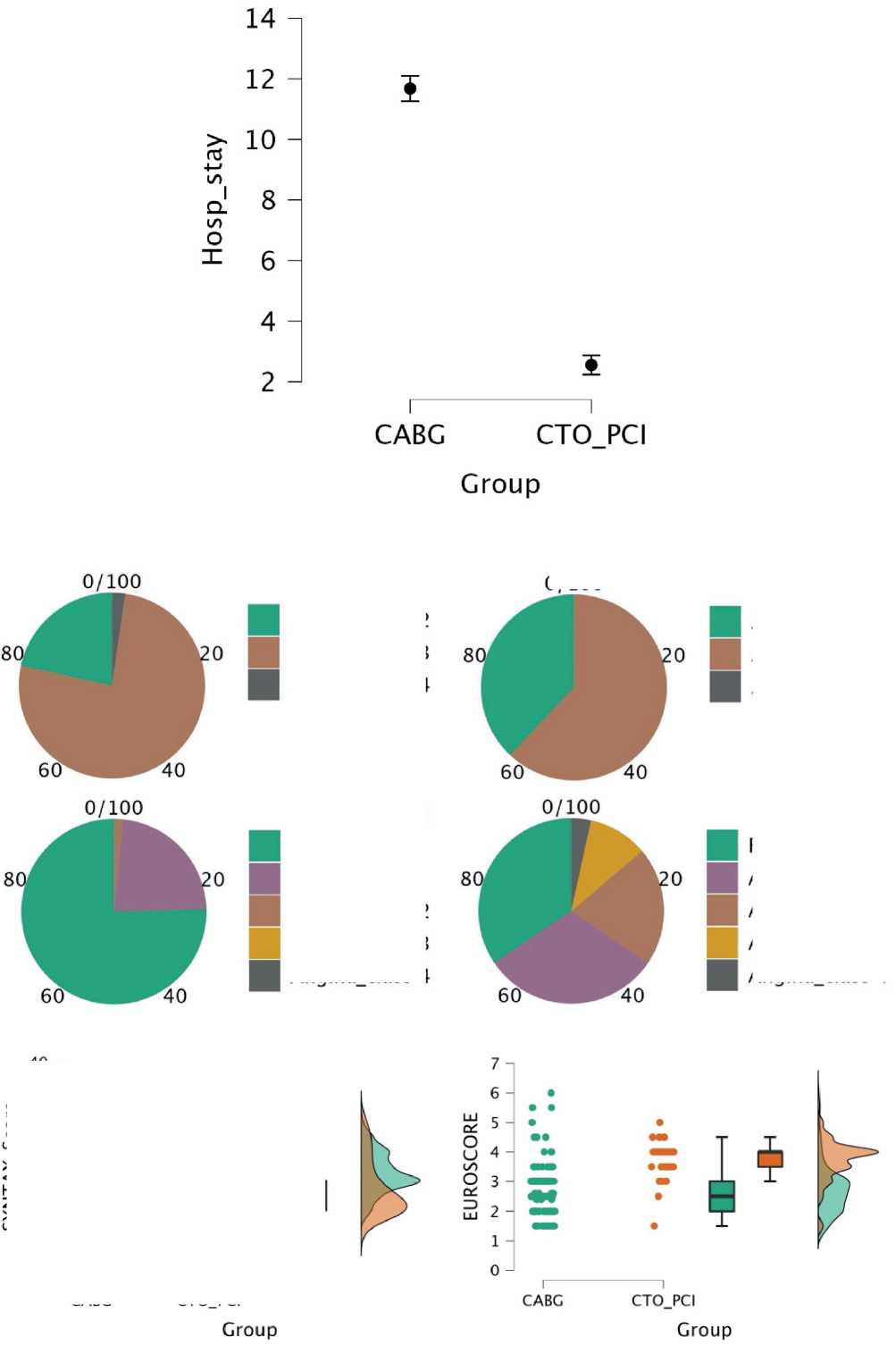
Procedure time CABG 312.3 ±25.3 min . Mean hospital stay CABG 11.67 ±17.8 . Procedure time PCI 94.5±17.9. Mean hospital stays for PCI 2.55 ±0.87 . PCI to 1 vessel 48%, 2V 24%, 3V 13.7%, 4Vs 13.7%. Off-pump CABG was used in 31%. LIMA graft was used in 100%
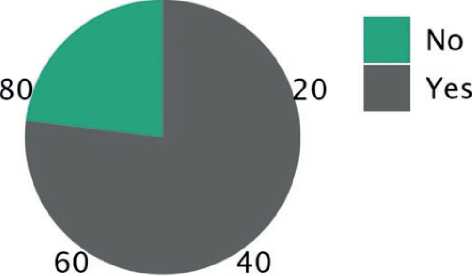
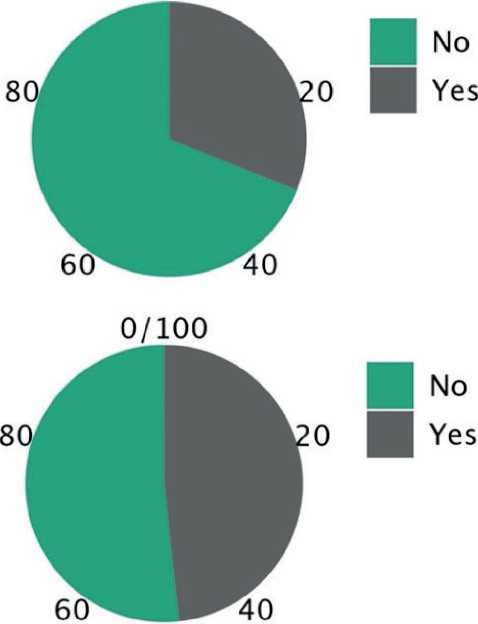
1year-outcomes
Post CABG CCS average 0.26±0.47 vs. Post PCI CCS average 1.17±1.1. Post CABG no or minimal angina in 98.3%. Post PCI CCS no or minimal angina 65% (P<0.001). 1y MACE post CABG 6.1% Vs 1Y MACE post PCI 31% (P 0.108). Repeated revascularization 1.5% for CABG vs Repeated Revascularization after PCI 6.8% (P 0.097). 1Y mortality post CABG 7.6%. 1Y mortality post PCI 3.44% (P0.4)
|
t |
df |
p |
|
|
OR_time |
43.837 |
157 |
< .001 |
|
Hosp_stay |
19.839 |
157 |
< .001ᵈ |
|
Angina_post |
-6.880 |
157 |
< .001ᵈ |
|
Repeat_Rev |
-1.670 |
157 |
0.097ᵈ |
|
MACE |
-1.617 |
157 |
0.108ᵈ |
|
Morbid |
-4.099 |
157 |
< .001ᵈ |
|
Mortality |
0.811 |
157 |
0.419 |
Discussion
The heart team decided more toward CABG for patients with a higher SYNTAX score, 3 VD, longer CTO segments, and a higher number of CTO lesions. Heart team decision was more toward PCI in patients with higher EURO scores and history of CVA. The procedural time was significantly longer in CABG. Hospital stay was longer with CABG.
Contemporary techniques were commonly used in both strategies (LIMA, BITA, off-pump), (Antegrade and retrograde recanalization in PCI with a failure rate of 13%.
Both techniques were associated with significant relief of angina. CABG was associated with a higher possibility of having no or minimal angina at one year (P<0.001).
One year MACE was numerically higher in the PCI group. Repeated revascularization was numerically higher in the PCI group.
Conclusion
In patients with moderate or high Complex anatomy and CTO, surgical or percutaneous revascularization is feasible. CABG is more effective in angina relief. PCI is associated with a shorter hospital stay and a higher possibility of repeated revascularization.
Limitations:
-
• Retrospective observational data
-
• Small number of patients recruited
-
• Short term follow-up
-
• Lack of medical limb
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Conflict of Interest
The authors declare no conflict of interest.
Funding
Authors of the present study didn’t receive any private or governmental
Supplementary data
CABG/CEA
|
OFF PUMP |
ON PUMP |
|
|
OPEN/CEA |
83 |
40 |
|
■ PULL/OUT |
6 |
1 |
■ OPEN/CEA ePULL/OUT
|
MORTALITY |
CABG/CEA 10 (7.6 %) |
CTO/PCI 1 (3.4%%) |
P-VALUE 0.69 |
||||
|
MACE |
9(6.9%) |
4(13.7%) |
0.10 |
||||
|
ANGINA CLASS |
98/NO |
30/CLASS 2 |
2/CLASS 2 |
10/NO |
9/CLASS 2 |
6/CLASS 2 |
0.0001 |
|
REPEAT REVASCUL- RIZATION |
2(1.5%) |
2(6.8%) |
0.09 |
||||
CTO LAD
Recanal PCI
CTO Vs
CTO_RCA/PDA
CTO CX-OM
Non_App Antegarde Retrograde Ante_Retro Failed
EUROSCORE
4.0 -| т
3.5 - -
3.0 -
2.5 -
CABG CTO_PCI
Croup
33.0 -
32.5 - J
о
Й 32.0 - i
X
<
H 31.5 - (,
31.0 -
30.5 -
CABG CTO_PCI
Croup
4.5 -
4.0 - g1 3.5 - 2.5 - 2.0 - I CABG CTO_PCI Group 350 - 300 - * щ 250- E 4 200 - QC ° 150 - 100 - $ 50 - CABG CTO_PCI Group CABG group: Previous PCI 0/100 PCI group: previous PCI 0/100 0/100 Angina_CI Angina_class 2 Angina_class 3 Angina_class 4 Angina before CABG Angina before PCI-CTO AnginaCl Angina_class 2 Angina class 3 Angina_class 4 0/100 Angina_post Free Angina_classl Angina_class 2 Angina_class 3 Angina class 4 Angina_post Free Angina_classl Angina_class 2 Angina_class 3 Angina_class 4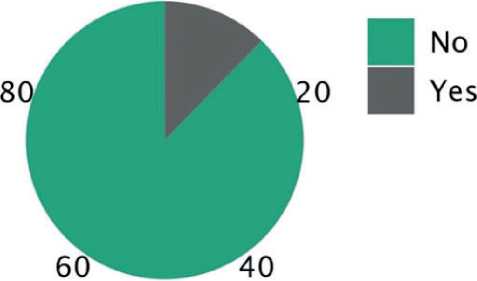

Список литературы PCI VS CABG for patients with CTO: contemporary techniques and outcome-single center experience
- Christofferson RD, Lehmann KG, Martin GV, Every N, Caldwell JH, Kapadia SR. Effect of chronic total coronary occlusion on treatment strategy. Am J Ca rdiol. 2005; 95: 1088-91.
- Fefer P, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012; 59: 991-7.
- Brilakis ES, et al. Developments in coronary chronic total occlusion percutaneous coronary interventions: 2014 state-of-the-art update. J Invasive Cardiol. 2014; 26: 261-6.
- Strauss BH, Shuvy M, Wijeysundera HC. Revascularization of chronic total occlusions: time to reconsider? J Am Coll Cardiol. 2014; 64: 1281-9.
- Farooq V, et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol. 2013; 61: 282-94.


