Поражение нервной системы при СOVID-19
Автор: Белопасов Владимир Викторович, Яшу Яссин, Самойлова Екатерина Михайловна, Баклаушев Владимир Павлович
Журнал: Клиническая практика @clinpractice
Рубрика: Обзоры
Статья в выпуске: 2 т.11, 2020 года.
Бесплатный доступ
В статье на основе имеющихся публикаций систематизированы сведения об основных формах поражения периферической и центральной нервной систем, их клинических проявлениях при СOVID-19. Обсуждаются методы диагностики (лабораторные, инструментальные и лучевые) и лечебная тактика при разных нозологических формах - от краниальных мононевропатий до острой воспалительной полинейропатии Гийена-Барре и тяжелых поражений головного и спинного мозга в виде острой геморрагической некротизирующей энцефалопатии и миелопатий. С точки зрения патогенеза, неврологические нарушения при COVID-19 могут быть обусловлены «цитокиновым штормом», гипоксемией, нарушениями гомеостаза (энцефалопатия критических состояний), нейротропностью и нейровирулентностью SARS-CoV-2 (изолированное поражение черепных нервов, очаговые и диффузные поражения ЦНС), а также смешанным воздействием перечисленных факторов. COVID-19 влияет на течение хронических неврологических заболеваний, особенно, связанных с нейроиммунными нарушениями. Все перечисленное определяет необходимость мультидисциплинарного подхода к лечению COVID-19 и его осложнений с обязательным участием специалиста-невролога.
Новая коронавирусная инфекция, вирусное поражение головного и спинного мозга, энцефалопатия критических состояний
Короткий адрес: https://sciup.org/143172674
IDR: 143172674 | DOI: 10.17816/clinpract34851
Текст научной статьи Поражение нервной системы при СOVID-19
Каждое заболевание имеет свою историю развития, клинические симптомы, течение, исход. Ставшая реальностью и катастрофой сего- дняшнего дня для многих стран мира атипичная пневмония, вызванная новым зоонозным бетако-ронавирусом SARS-CoV-2, характеризуется высокой степенью неблагоприятных осложнений клиническая; 20
Том 121 № 0 2
СПИСОК СОКРАЩЕНИЙ
ACE2 — ангиотензинпревращающий фермент 2
CAM-ICU (Confusion Assessment Method-Intensive Care Unit) — метод оценки спутанности сознания для отделения интенсивной терапии
DRS (Delirium Rating Scale) — шкала тяжести делирия
DRS-R-98 (Delirium Rating Scale-R-98) — шкала тяжести делирия R-98
DWI (Diffusion Weighted Imaging) — диффузионно-взвешенные изображения (режим МРТ)
FCoV (Feline Coronavirus) — коронавирус кошек
FLAIR — (Fluid attenuated inversion recovery) — режим МРТ
GM1 — ганглиозид GM1
GQ1b — ганглиозид Q1b
HCoV- HKU1 (Human coronavirus HKU1) — коронавирус человека HKU1 HCoV- NL63 (Human coronavirus NL63) — коронавирус человека NL63 hCoV-229E (Human coronavirus 229E) — коронавирус человека 229Е HCoV-NL63 (Human coronavirus NL63) — коронавирус человека NL63 HCoV-OC43 (Human coronavirus OC43) — коронавирус человека OC43 ICDSC (Intensive Care Delirium Screening Checklist) — контрольный список оценки спутанности сознания для отделения интенсивной терапии
Ig (immunoglobulin) — иммуноглобулин
IgA (immunoglobulin A) — иммуноглобулин класса A
IgG (immunoglobulin G) — иммуноглобулин класса G
IgM (immunoglobulin M) — иммуноглобулин класса M
IL (interleukin) — интерлейкин
JHMV — штамм JHM вируса гепатита мыши
MERS (Middle East respiratory syndrome) — ближневосточный респираторный синдром
MERS Co-V (Middle East respiratory syndrome-related coronavirus) — коронавирус ближневосточного респираторного синдрома
MHV (mouse hepatitis viruses) — вирус гепатита мыши
MHV-4 — штамм 4 вируса гепатита мыши
MHV-A59 — штамм A59 вируса гепатита мыши
NMDA (N-methyl-D-aspartic acid) — N-метил-D-аспарагиновая кислота
NMDAR (N-methyl-D-aspartic acid receptor) — рецептор N-метил-D-аспарагиновой кислоты
NT-proBNP — N-терминальный пропептид натрийуретического гормона
Nu-DESC (The Nursing Delirium Screening Scale) — шкала скрининга делирия
RAR (rapid adapting receptors) — быстро адаптирующиеся рецепторы
RASS (Richmond Agitation-Sedation Scale) — шкала возбуждения-седации Ричмонда
SARS (Severe acute respiratory syndrome) — тяжелый острый респираторный синдром (ТОРС)
SARS-CoV (Severe acute respiratory syndrome-related coronavirus) — коронавирус тяжелого острого респираторного синдрома (ТОРС)
SARS-CoV-2 (Severe acute respiratory syndrome-related coronavirus 2) — новый коронавирус тяжелого острого респираторного синдрома-2
Th (T helper cells) — Т-хелпер
TMPRSS2 (Transmembrane protease, serine 2) — мембраносвязанная сериновая протеаза
ГЭБ — гематоэнцефалический барьер
ИВЛ — искусственная вентиляция легких
КТ — компьютерная томография
МРТ — магнитно-резонансная томография
ПЦР — полимеразная цепная реакция
РНК — рибонуклеиновая кислота
СOVID-19 (CoronaVirus Disease 2019) — коронавирусная инфекция 2019 года
ЦНС — центральная нервная система
ЦСЖ — цереброспинальная жидкость
ЭМГ — электромиография
ЭЭГ — электроэнцефалограмма и летальности, причинно связанных не только с нарушением газообмена в легочных альвеолах, прогрессирующей дыхательной недостаточностью, гипоксией, но и декомпенсацией функционирования, структурным поражением многих органов и систем, обеспечивающих жизнедеятельность организма больного, в том числе головного и спинного мозга.
Анализ многочисленных публикаций, посвященных новой коронавирусной инфекции (СOVID-19), с использованием баз данных PubMed, Scopus и Google Scholar свидетельствует о том, что в патологический процесс могут вовлекаться оболочки, сосуды, паренхима мозга. Возникающие под воздействием проникшего через гематоэнцефалический барьер (ГЭБ) в центральную нервную систему (ЦНС) вирусного агента клеточные реакции в зависимости от состояния Т- и В-клеточного иммунитета заболевшего могут протекать бессимптомно, моносимптомно либо вызывать клинические проявления менингита, энцефалита, энцефалопатии. Поражение черепных, периферических нервов, скелетных мышц проявляется моно- и полиневропатиями, мышечной утомляемостью, миалгиями, рабдомиолизом [1–10].
В продромальном (5–7 дней) и остром периодах при наличии сухого кашля, лихорадки, дыхательной недостаточности больные предъявляют жалобы на подавленность, утомляемость, упадок сил, снижение активности, невозможность сосредоточения, нарастающую тревогу, ощущение стягивания, болезненность мышц, головную боль без тошноты, рвоты, несистемное головокружение, неустойчивость при ходьбе, расстройство обоняния, вкуса. При обследовании во время госпитализации удельный вес миалгий и утомляемости в зависимости от возраста и выраженности респираторного синдрома составляет от 14,4 до 100%, инсомнии — 30,5%, головокружения — 9–7%, атаксии — 0,5–1%, головной боли — 3,4–41%, нарушений обоняния и вкуса — 19,7% (гипосмии 1,8–30,0%; гипогевзии — 5,6%, дисгевзии — 8,5%; агевзии — 1,7%) [1, 10–13]. Среди инфицированных большую часть составляют лица пожилого и старческого возраста с сердечно-сосудистой и цереброваскулярной патологией. Нарушения психики представлены когнитивными, соматизиро-ванными расстройствами тревожно-фобического (8,5–28,8%) и депрессивного (9,5–16,5%) спектра [14], их причинами становится дистресс, связанный с заболеванием, изоляцией, пребыванием в палате интенсивной терапии, реанимационном отделении, развитием осложнений, страхом ухода из жизни. Низкая стрессоустойчивость, деморализация, осознание некурабельности заболевания могут привести к суициду [15–17]. По данным системного обзора [16], неврологические нарушения, которые могут возникать до появления симптомов инфицирования и в последующие периоды течения заболевания, выявляются у 25% больных и требуют оказания неотложной помощи. К ним относятся ажитация, панические атаки, спутанность сознания, психомоторное возбуждение, дезориентация, делирий, сомноленция, оглушение, сопор, кома, эпилептические приступы, церебральные дисгемии [14, 18–20]. Из известных форм сосудистой патологии на долю инфаркта мозга приходится 5–31%, на геморрагический инсульт — до 6%, тромбоз венозных синусов и вен — по 0,5% [21–23]. Развитие спутанности, потери сознания у 8–15% больных может быть причинно связано помимо острого нарушения мозгового кровообращения с регионарным воспалением, венозным застоем, отеком, гипоксией мозга, повышением интракраниального давления, возникновением неконвульсивного эпилептического статуса [24–26]. В генезе судорожных приступов важная роль отводится индукции цитокинов, нейротоксичности, активации рецепторов глутаматергической трансмиссии, гипокальциемии, гипоксемии [27, 28]. Носительство вируса, проникновение его в нейроны коры головного мозга не инициирует развития эпилептиформной активности, не влияет на клинические характеристики и частоту приступов у больных эпилепсией. Важное, но не определяющее значение для эпилепти-зации нейронов имеет структурно-функциональная дезорганизация в очаге поражения, вызванная воспалительным процессом в острой стадии заболевания, спровоцированного SARS-CoV-2 [29]. Частота данного осложнения при СOVID-19 не превышает 1%. Однако при поступлении в стационар больного эпилепсией имеется риск не только провокации или учащения приступов, но и развития эпилептического статуса [30–33].
ФОРМЫ НЕВРОЛОГИЧЕСКИХ НАРУШЕНИЙ Острый менингоэнцефалит
Впервые описан у мужчины в возрасте 24 лет, жителя г. Ухань (Китай), находившегося на амбулаторном лечении по поводу гриппа [34]. Начало заболевания острое. На фоне лихорадки, не купируемой антипиретиками, появилась головная боль, сменившаяся на 9-й день энцефалитической реакцией в виде транзиторных билатеральных тонико-клонических судорог и потери сознания (кома 1,6 баллов, по шкале комы Глазго). При неврологическом осмотре выявлялась ригидность затылочных мышц, очаговые симптомы отсутствовали. Цереброспинальная жидкость (ЦСЖ) — ликворное давление 320 mmH2O, цитоз 12 в µl (10 – монону-клеары); тест на коронавирус РНК SARS-CoV-2 положительный, в крови, мазке из носоглотки — отрицательный. Антитела к простому герпесу 1-го типа и Varicella zoster в образцах сыворотки крови не определены. По результатам компьютерной томографии (КТ) признаки отека головного мозга не визуализировались, в легких (правой верхней и обеих нижних долях локальные тени, фокусы уплотнения по типу «матового стекла», характерные для СOVID-19 пневмонии); по данным магнитно-резонансной томографии (МРТ) в режимах Т2, DWI и FLAIR — гиперденсивность стенки правого бокового желудочка, мезиального отдела височной доли, гиппокампа. Проводимое лечение (искусственная вентиляция легких, внутривенное введение ацикловира, цефтриаксона, ванкомицина, кортикостероидов, а также леветирацетама для купирования судорог и фавипиравира через назогастральный зонд в течение 10 сут) дало положительный результат.
Аналогичный случай представлен M. Ye с со-авт. [ 35 ]: при схожести симптомов, данных оценки ЦСЖ, результатов КТ легких и мозга, при положительном результате теста на SARS-CoV-2 доказать у наблюдаемого пациента мужского пола в возрасте 28 лет присутствие коронавируса в ликворе не удалось. Высказано предположение, что это связано с быстрой его элиминацией из ЦСЖ и, соответственно, низким титром, о чем свидетельствует отсутствие анти-SARS-CoV-2 IgM и IgG. По окончании курса лечения, включающего ингаляцию кислорода, инфузию маннита, введение арбидола через зонд, достигнуто полное выздоровление больного — вирус при двукратной оценке мазков из носоглотки не обнаружен. Диагноз поставлен клинически, МРТ головного мозга не проводилось.
На основании оценки имеющихся данных [36– 38] можно заключить, что результаты неврологического обследования, лабораторной и лучевой диагностики взрослых больных cопоставимы. Исключением являются случаи, когда причиной гипертермии и менингоэнцефалита становится другой возбудитель. C. Lovati с соавт. [39] опубликовал наблюдение развития воспалительного поражения головного мозга в период вспышки СOVID-19 в Италии, ассоцированного с вирусом простого герпеса (Herpes simplex virus 1-го типа). Присутствие его в ликворе, характерные изменения при нейровизуализации (МТР) и отрицательных результатах тестирования на SARS-CoV-2 (кровь, ликвор) не вызывают сомнения в правильности диагноза.
У детей до 16 лет, инфицированных SARS-CoV-2, неврологические осложнения не возникают [40], только некоторые из них предъявляют клиническая; 20
тактика ™
жалобы на головную боль. Однако единственное описание развития менингоэнцефалита у ребенка 11 лет [41] заставляет по-иному оценить заключение, сделанное авторами. Речь пойдет о необычном случае. Согласно анамнестическим данным, у больного в отсутствии повышения температуры и катаральных признаков, но при наличии выраженной утомляемости внезапно развился эпилептический статус, купированный антиконвульсантами. Очаговой симптоматики также не наблюдалось. Характерных для воспалительного процесса и отека мозга признаков при КТ головы обнаружить не удалось, на электроэнцефалограмме (ЭЭГ) зарегистрирована медленная активность дельта-диапазона в лобных долях. В ликворе примесь крови (эритроциты — 921, лейкоциты — 16, содержание белка и глюкозы — норма), результат теста из носоглотки SARS-CoV-2 положительный. Через 6 дней без этиотропной терапии наступило выздоровление. Это вызывает сомнение в формулировке диагноза. Такие преходящие клинические проявления и изменения в ликворе возможны при атипично протекающем субарахноидальном кровоизлиянии вследствие частичного разрыва интракраниальной артериальной аневризмы. Проведение спиральной КТ- и МРТ-ангиографии с целью уточнения диагноза позволяет рассеять возникшие сомнения. В равной степени это касается и исследования ЦСЖ на наличие коронавируса [34, 42]. Примером может служить наблюдение M. Al-Olama с соавт. [43]. Причиной повторного обращения больного к врачу на 4-й день заболевания стали головная боль, общемозговые проявления в виде заторможенности, нарушения ориентировки во времени и месте, сомноленции, рвоты, возникшие на фоне повышения температуры, миалгии, сухого кашля, диареи. Результаты амбулаторного обследования (ПЦР тест на SARS-CoV-2, физикальные данные) были отрицательные, КТ грудной клетки при поступлении в стационар без особенностей. Неврологический осмотр не выявил отклонений. Анализ крови: лейкоцитоз, высокое содержание глюкозы, прокальцитонина, D-димера. Мазок из носоглотки: наличие SARS-CoV-2. КТ головного мозга: интралобарная, субдуральная гематома, субарахноидальное кровоизлияние, отек мозга, масс-эффект, накопление контраста оболочками мозга. КТ-ангиография исключила наличие тромбоза синусов, вен, аномалий развития церебральных сосудов. Диагностирован геморрагический менингоэнцефалит, при анализе ЦСЖ во время операции тест на коронавирус положительный.
Способность проникать в ликвор и головной мозг обнаруживают не только SARS-CoV-2, но и другие коронавирусы человека и животных (OC43, 229E, MERS и SARS) [44 –47], но реально поражение оболочек и паренхимы мозга возникает крайне редко [48–51]. Оценить частоту встречаемости данного осложнения, ориентируясь только на публикации, невозможно. Глубокому анализу обычно подвергаются клинические, лабораторные и инструментальные данные, результаты аутопсий, отражающие состояние и развитие воспалительного процесса в верхних и нижних дыхательных путях, легких. Целенаправленное патоморфологическое исследование состояния головного мозга еще впереди. Все усилия медицинского персонала повсеместно и в первую очередь направлены на сохранение здоровья и жизни больных. Поэтому и в связи с ограниченными возможностями использования специальных методов исследования (люмбальная пункция, ЭЭГ, КТ, МРТ) у врача для постановки диагноза в этих условиях остаются только его клиническое мышление и профессионализм. Вместе с тем проведение полноценного обследования при доминировании в клинической картине психопатологических нарушений, отсутствии менингеальных и очаговых симптомов позволяет идентифицировать не воспалительную, а аутоиммунную природу их возникновения. Увеличение в ликворе интерлейкина 6 (IL6), антител к NMDA глутаматному рецептору (N-methyl-D-aspartic acid — N-метил-D-аспа-рагиновая кислота) определенно свидетельствует о возможности развития у больных COVID-19 пара-инфекционного анти-NMDAR-энцефалита [52]. Внутривенное введение иммуноглобулина и применение высоких доз дексаметазона даже при отмене антипсихотической терапии дает положительный результат.
Участие аутоиммунных механизмов в демиелинизации белого вещества головного мозга предполагается и при воздействии коронавируса на нейроглию [53]. Главным образом это касается случаев отсутствия плеоцитоза в ликворе. Апоптоз, гибель олигодендроцитов, активация провоспалительных цитокинов (гамма-интерферона, IL1, IL6, IL12, трансформирующего ростового фактора бета) [8, 54] способствуют развитию иммуноопосредованного поражения определенных, наиболее подверженных эксайтотоксичности церебральных структур, что морфологически проявляется в виде лейкоэн- цефалита. Иммунокоррекция вначале курсового лечения в виде плазмафереза [37] при отсутствии признаков активной инфекции обеспечивает регресс общемозговой и очаговой неврологической симптоматики.
Острый геморрагический энцефалит/ некротизирующая энцефалопатия
Одна из форм вторичного поражения головного мозга известна неврологам, патологоанатомам, инфекционистам и педиатрам на протяжении более ста лет как острый геморрагический энцефалит (лейко-, полиоэнцефалит), некротический геморрагический энцефаломиелит (болезнь Харста). Как самостоятельное заболевание было выделено после эпидемии гриппа, охватившей многие страны Европы и Россию в 1918–1919 годах. Его типичные проявления развивались вслед за стремительным повышением температуры в считанные часы, дни, преимущественно у детей и молодых людей. В последующие годы регистрировались только единичные случаи. При уточнении этиологии установлена роль других нейроинфекций (энтеровирусов, парагриппа, герпеса, коронавирусов hCoV-229E, OC43, NL63, HKU1, MERS Co-V, SARS-CoV) [55-61]. Развитие острой геморрагической некротизирующей энцефалопатии возможно и при СOVID-19 [62–65]. У больных с клиническими признаками инфицирования верхних дыхательных путей (кашель, одышка) возникают головная боль, поведенческие нарушения (дезориентировка, двигательное беспокойство, непонимание и игнорирование речи окружающих), потеря сознания, гиперкинезы, судороги. Очаговые и оболочечные симптомы имеются не всегда. При нейровизуализации (КТ, МРТ головного мозга) выявляется симметричное распространенное или ограниченное поражение белого вещества височной доли, островка, базальных ганглиев, таламуса с признаками кровоизлияния (от множественных рассеянных микрогеморрагий до сливных), размягчение мозга, что типично для некротической энцефалопатии. Реже страдают ствол мозга, мозжечок. В отдельных зонах повреждения наблюдается накопление контраста в коре, пиаарахноидальных оболочках, по ходу извилин, в паренхиме полушарий мозга в виде «кольца».
Нейровизуализационные признаки лейкоэнцефалопатии с множественными юкстакортикальны-ми и каллозальными микрогеморрагиями обнаруживаются преимущественно у больных с низкими показателями сатурации (менее 80%) со стабиль- ной гемодинамикой, отсутствием нарушений свертываемости крови. Базальные ганглии, в отличие от гипоксико-ишемической энцефалопатии, остаются интактными [66, 67].
Превалирование очаговых симптомов над мозговыми, мультифокальность, выявляемая при нейровизуализации и неврологическом осмотре, билатеральное поражение зрительных нервов, белого вещества в полушариях мозга, торакальных сегментах спинного мозга, положительная ПЦР на SARS-CoV-2, лимфоцитарный плеоцитоз в ликворе, гиперпротеинарахия, олигоклональ-ные IgG, положительный эффект иммунокоррекции (пульс-терапия метилпреднизолоном, внутривенно IgG) — доказательная база, позволяющая диагностировать редкое для взрослых демиелинизирующее осложнение, классифицированное в неврологии как острый диссеминированный энцефаломиелит [68, 69]. При морфологической оценке помимо геморрагических петехиальных и небольших сливных кровоизлияний видны очаги некроза, аксонального повреждения, потери миелина, лакунарные инфаркты, периваскулярные воспалительные инфильтраты, изменения, характерные для поражения мелких сосудов в виде артериолосклероза и эндотелиита [70]. В стволе, базальных ядрах, сером веществе спинного мозга, лептоменинксе они отсутствуют, что отличает данную форму патологии от острой некротической геморрагической и гипоксико-ишемической энцефалопатии.
Еще один вариант вызванной коронавирусом патологии мозга, сходный по патогенезу, морфологической картине с описанной выше формой, но отличный по исходу, объему, локализации, обратимости, — острая геморрагическая задняя обратимая энцефалопатия [71]. Диагностируется у больных с головной болью, нарушенным сознанием, судорогами, поведенческими расстройствами без выраженных метаболических и соматических осложнений с использованием методов нейровизуализации (КТ, МРТ). Типичный паттерн — субкортикальный вазогенный отек, билатеральное, чаще симметричное поражение белого вещества затылочных, височных долей, подкорковых ядер, кроме таламуса, а также наличие множественных микрогеморрагий в коре, мозолистом теле. При проведении КТ-ангиографии и венографии изменения в сосудистом русле в виде стеноза, окклюзии и нарушения кровотока отсутствуют. Ликвор не изменен либо возможны протеинархия, ксантохромия.
<линическая’2п20
п эакти ка Том 11 №2
Геморрагический компонент при первичном обследовании (КТ) визуализируется не всегда [72]. На ЭЭГ регистрируются неспецифические изменения в виде медленноволновой или эпилептиформной активности в височных отведениях [73]. Результаты стандартного тестирования образцов крови и ЦСЖ на вирусы гриппа А, В, простого герпеса, ветряной оспы, цитомегаловируса, респираторно-синцитиального вируса, лихорадки Западного Нила отрицательные; в мазках, полученных из носоглотки, обнаруживается SARS-CoV-2, в ЦСЖ — не выявляется [29, 62, 66, 67, 71, 74].
Патоморфологическая картина представлена отеком, симметричным поражением белого вещества, воспалительными инфильтратами в периваскулярных пространствах, нервной ткани, образованными полинуклеарами, лимфоцитами, сливными фокусами кровоизлияния в подкорковых узлах, экссудативно-пролиферативными изменениями в стенках сосудов и нервной ткани [75, 76].
Вирус SARS-CoV-2 в связи с инициированием «цитокинового шторма» может обусловить развитие гемофагоцитарного лимфогистиоцитоза, клинические и нейровизуализационные проявления которого имитируют острую некротическую энцефалопатию при СOVID-19 [45 , 54, 66, 77], сепсисе [78, 79], полиорганной недостаточности [ 80 ], коагу-лопатическом кровотечении вследствие диссеминированного внутрисосудистого свертывания [81; собственные наблюдения]. Терапия назначается согласно протоколам ведения больных, находящихся в критическом состоянии. Положительный исход возможен не всегда.
Краниальные мононевропатии
Проникновение коронавирусов в организм человека происходит воздушно-капельным, воздушно-пылевым и контактным путями, поэтому в первую очередь поражаются эпителиальные клетки слизистых оболочек глаза, полости носа, рта, верхних и нижних дыхательных путей, иннервация которых обеспечивается терминальными ветвями и рецепторным аппаратом обонятельного, тройничного, лицевого, языкоглоточного и блуждающего нервов. РНК SARS-CoV-2 обнаруживаются в конъюнктивальном мешке, слезной жидкости, слюне, мокроте, мазках полости рта, носоглотки, промывных водах бронхов, паренхиме легкого при аутопсии [82–85]. Возможность развития глазной патологии в виде повреждения переднего сегмента глаза, оптической невропатии была уста- новлена при обследовании больных, инфицированных 229E, HCoV-NL63, SARS-CoV-2 [84, 86–88], более того, конъюнктивит/кератоконъюнктивит может быть первым, в том числе у медперсонала, и единственным симптомом СOVID-19 [89–91]. Китайский офтальмолог Ли Вэньлян из Уханя стал жертвой пандемии, заразившись от больного глаукомой, носителя SARS-CoV-2 [92]. При наличии лихорадки и пневмонии признаки воспаления (фотофобия, слезотечение/эпифора, гиперемия, отек/ хемоз) конъюнктивы встречаются чаще, но им не всегда уделяется должное внимание [82]. Тяжелые проявления в виде увеита, васкулита, хореоидита, отслойки сетчатки описаны у кошек, умерших от FCoV [93]. В экспериментальных условиях нейротропные штаммы вируса гепатита мыши (MHV-A59, JHMV), а также бетакоронавирусы вирусов могут инициировать развитие дегенерации сетчатки, неврита зрительного нерва, энцефаломиелита у мышей, крыс, свиней [94–96]. Некоторые исследователи [97, 98] на основании полученных моделей считают вероятным участие коронавирусов в генезе рассеянного склероза. Было установлено, что аутореактивные лимфоциты могут перекрестно реагировать как с эпитопами коронавируса HCoV-OC43 зараженных мышей, так и с миелином человека [62].
Слизистые оболочки носа и полости рта, по сравнению с конъюнктивой и роговицей глазных яблок, более уязвимы [99]. Вирусы поступают в носоглотку не только при дыхании, но и из конъюнктивального мешка со слезой через слезно-носовой канал в нижнюю носовую раковину [12, 100–102]. Уже в дебюте заболевания больные могут предъявлять жалобы на боль в лице, заложенность носа без ринореи, изменения в восприятии запахов и вкуса [103–105]. Более того, внезапная потеря обоняния может наступать при хорошем самочувствии и благополучном течении заболевания [105]. Так, нарушение обонятельной функции, согласно данным проведенного опроса, проявилось у 357 (85,6%) из 417 выздоровевших от COVID-19 пациентов, при этом у большинства из них (88,2%) такое нарушение возникло одновременно или после проявления общеинфекционных симптомов, а у 11,8% — при их отсутствии. Потеря обоняния произошла у 284 (79,6%), хуже стали различать запахи 73 (20,4%) пациента. В течение первой недели после выписки из стационара восприятие выздоровевших восстанавливалось: при гипосмии — у всех, при аносмии — у 67,8% [103]. Эти данные были подтверждены C. Hopkins с соавт. [106] при обследовании еще большего контингента больных (2428 человек). В выборке из 60 пациентов, но при использовании количественного теста на идентификацию запаха Пенсильванского университета (University of Pennsylvania Smell Identification Test, UPSIT), обоняние оказалось сохранным только у 1 [107], в другом исследований [108] аносмия выявлена в 68% случаев COVID-19. При целенаправленном опросе не могли ощущать, дифференцировать запахи до 2/3 респондентов [109].
Наряду с указанными формами расстройства оценки обоняния могут проявляться в виде иллюзий, искаженного восприятия, обонятельных галлюцинаций (паросмии — 32,4%, фантосмии — 12,6%) [103, 110]. Нарушение обоняния, описанное и при других коронавирусных инфекциях, но никогда не рассматриваемое как клинически значимый для постановки диагноза признак [111, 112], в настоящее время предлагается признать в качестве надежного биомаркера COVID-19-инфекции [107, 113 , 114].
О нарушении вкуса сообщают многие исследователи [1, 107, 108, 115]. На основании опроса выделяют несколько клинических форм — агевзию (1,4–5,6%), гипогевзию (47,5%) и дисгевзию (21,1%). Другие ветви лицевого нерва, за исключением n. lingvalis, обеспечивающего восприятие соленого, кислого, горького, сладкого на передних 2/3 языка, остаются интактными. «Мишенью» коронавирусов являются: (а) хеморецепторы сосочков языка, эпителиальные клетки слизистых оболочек полости рта, глотки; (б) афферентные нервные волокна краниальных нервов; (в) при виремии и ретроградном распространении — кора височной доли, ствол мозга [15, 99, 115]. Мимические мышцы лица страдают крайне редко [116]. Одной из причин может стать коинфекция [117]. Степень возникающих расстройств варьирует от незначительной (бессимптомные пациенты, у которых нарушения вкуса обнаруживаются при тестировании) до выраженной (лихорадящие, с респираторным синдромом) [118]. В 23,6–41,7% случаев развивается дисфункция не только вкусовой, но и обонятельной системы [101, 104, 119–120]. Специфичность ее поражения высокая — значительно выше, чем у больных с респираторными заболеваниями, вызванными риновирусом, вирусом Эпштейна–Барр, гриппа, некоторыми коронавирусами [121]. Выявляемость хемочувствительных расстройств (от 19,4 до 88%) у пациентов с COVID-19 зависит от качества и полноты их обследования. Восстановление восприятия вкусовых ощущений происходит с той же полнотой и в те же сроки, как при нарушении обоняния, но у отдельных больных (34%) возникшие изменения сохраняются [119].
<линическая’2п20
п эакти ка Том 11 №2
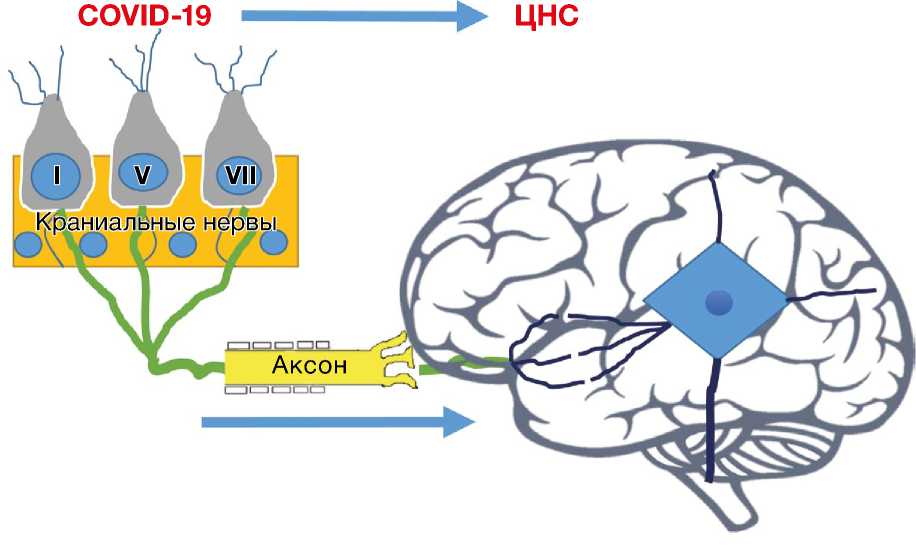
Рис. 1. Инвазия SARS-CoV-2 в структуры мозга
ретроградно перемещаться по блуждающему нерву [131, 132] (рис. 1). У инфицированных интраназально SARS-CoV мышей высокие уровни вирусной РНК обнаруживаются в таламусе и стволе мозга со 2–4го дня после инокуляции, летальный исход наступает к концу недели до развития клеточного иммунного ответа [133]. В связи с этим логично считать [65, 134 ], что тяжелый острый респираторный дистресс-синдром при инвазии SARS-CoV-2 не только связан с повреждением пневмоцитов и альвеолярных клеток легкого, но и с нейротропным влиянием вируса на дыхательный центр продолговатого мозга.
Синдром Гийена–Барре
Первый вариант — иммуноопосредованный — связан с демиелинизацией нервных волокон (мие-линопатия) [3, 135–145], второй — с аксональным их повреждением (аксонопатия) [138, 140, 144, 146, 147], третий — с дизавтономией и неадекватной секрецией антидиуретического гормона [148].
Клинические проявления, нейрофизиологические и лабораторные данные аналогичны таковым при других вирусных и бактериальных инфекциях, включая некоторые типы коронавирусов [149–151]. Развитие симптомов (нарастающая слабость, парапарез нижних конечностей) происходит на протяжении суток с наличием или без предшествующих признаков острого респираторного заболевания, но в ряде случаев первоначально возникает потеря вкуса и обоняния. К 3–4-му дню выраженность двигательных нарушений достигает максимума. При осмотре больного выявляется выпадение коленных и ахилловых рефлексов, снижение тактильной и болевой чувствительности в виде «носок». В ЦСЖ определяются повышенное содержание белка (124 mg/dL при норме 8–43) при неизменном цитозе (белково-клеточная диссоциация), отсутствие антител к ганглиозидам GM1 и GQ1b. Данные нейроэлек-трофизиологического исследования типичны для демиелинизирующей полинейропатии (удлинение дистальной латенции, значительное снижение скорости проведения по двигательным волокнам, отсутствие F-волны, Н-рефлекса). При визуализации с гадолинием на МРТ определяются утолщение, накопление контраста в корешках спинного мозга, лицевого нерва [138, 142, 145, 152], оболочках по передней поверхности ствола и верхнешейных сегментов спинного мозга [153]. Диагностика острой моторно-сенсорной аксональной полиневропатии базируется на электромиографических критериях (уменьшение амплитуды, отсутствие дистального М-ответа, увеличение резидуальной латентности при нормальной или незначительно сниженной скорости проведения по нервам). Поражение черепно-мозговых нервов выражается развитием про-зопареза/прозоплегии изолированно [154, 155] или в сочетании с бульбарными нарушениями. Обращает внимание, что клинические проявления миели-но- и аксонопатий предшествуют появлению соматических жалоб (сухой кашель, одышка, повышение температуры до 38°C) или возникают с интервалом 5–10 дней. О причинной связи с коронавирусной инфекцией СOVID-19 свидетельствуют данные лучевой диагностики (КТ легких), наличие лимфопении в крови, положительный ПЦР-тест SARS-CoV-2 при оценке мазков из носоглотки. В ЦСЖ идентифицировать возбудитель не удается [140, 156]. Проведение активной неспецифической этиотропной (прием арбидола, лопинавира, ритонавира) и патогенетической (внутривенное введение иммуноглобулина G в дозе 0,4 г/кг в сутки) терапии обусловливает нейтрализацию вируса, полный или частичный регресс неврологических и висцеральных проявлений [144, 157]. У больных с прогрессирующим течением заболевания, тяжелым респираторным синдромом, сахарным диабетом, длительным пребыванием на ИВЛ прогноз не всегда благоприятен, возможен летальный исход [137].
Помимо VII, IX, X пар могут страдать III, IV, VI черепно-мозговые нервы, мозжечок, мозжечковые ножки, верхний, грудной отделы спинного мозга. Их поражение формирует картину атипично протекающих иммуноопосредованных вариантов краниальной и периферической моторносенсорной полиневропатии. У одной пациентки из 9 описанных больных имелся асимметричный неполный парез глазодвигательных мышц в сочетании с утолщением оболочек зрительных нервов (по данным МРТ), у остальных — аносмия, агевзия, клинические проявления синдрома Миллера–Фишера, для которого типична триада симптомов — наружная/межъядерная офтальмоплегия, атаксия, арефлексия [140, 158–160]. До развития неврологических симптомов все отмечали повышение температуры, общую слабость, сухой кашель, жидкий стул. Тесты на наличие коронавируса в ЦСЖ и смыве из ротоглотки были положительными, в ликворе — белково-клеточная диссоциация, повышенное, но не всегда, содержание IgG-антител к ганглиозиду GQ1b [140, 158]. Несмотря на возможность данных антител влиять на состояние нервно-мышечного синапса, патологической утомляемости мышц не наблюдается. Наружная офтальмоплегия как моносимптом возникает крайне редко [161].
Преходящая диплопия, ассоциированная с наличием антител к ацетилхолиновым рецепторам, описана А. Perez с соавт. [162]. При пандемии больные с миастенией, синдромом Ламберта–Итона, другими нервно-мышечными заболеваниями [163–165] относятся к лицам с высоким риском заражения, отягощения соматического статуса, развития и прогрессирования дыхательной недостаточности. Повышение экспрессии внутриклеточных цитокинов и продукции тканевых антител, а также применение сульфата магния, глюкокортикостероидов, интерферонов, гидроксихлорохина, азитромицина, некоторых антибиотиков, деполяризующих миорелаксантов, антиконвульсантов, транквилизаторов, психотропных средств — далеко не все причины миастенического криза при COVID-19 [163, 166, 167].
Стволовой энцефалит (ромбэнцефалит) характеризуется подострым развитием прозо-, глоссопареза, глазодвигательных, мозжечковых, сенсорных нарушений в виде альтернирующей плечеконечностной гипестезии [168]. Объем движений, сила, мышечный тонус, рефлексы не изменены. Симптомы ирритации нейронов бульбарной группы (икота, тахипноэ) присоединяются на фоне имеющихся общеинфекционных проявлений (повышение температуры, кашель, диарея). Снижение сатурации, наличие признаков пневмонии при КТ, положительный тест на COVID-19 не оставляют сомнений в инфицировании коронавирусом. При исследовании ликвора обнаружены плеоцитоз, про-теинархия, бактериальная флора не выявлена, ПЦР на SARS-CoV-2 не проведена. На МРТ-изображени-ях отчетливо видны очаговые изменения в белом веществе ствола мозга, нижней ножке мозжечка, верхнешейных сегментах спинного мозга. Те же методы исследования были ранее использованы для диагностики атипичного варианта стволового энцефалита Бикерстаффа (подтипа синдрома Миллера–Фишера) [169, 170].
Случай, описанный J. Kim с соавт. [150], свидетельствует, что при заражении бетакоронавирусом возможно одновременное вовлечение в патологический процесс центральной и периферической нервной систем в виде развития воспалительной полиневропатии и стволового энцефалита Би-керстаффа. Число публикаций, освещающих эту проблему, постоянно растет, отражая значимость ее для практических неврологов [151].
Более тяжелой и труднокурабельной патологией является изолированное поражение спинного мозга в виде острого поперечного миелита [171]. Аналогичные проблемы приходится решать медперсоналу при лечении и реабилитации больных, находящихся на ИВЛ, в связи с малосимптомным развитием у них полиневропатии и/или миопатии критических состояний [172, 173].
<линическая’2п20
п эакти ка Том 11 №2
Цереброваскулярные осложнения
Причинами развития ишемического инсульта при COVID-19 являются артериальная гипотензия, ишемия, воспаление миокарда, нарушения сердечного ритма, реологии и свертывающей системы крови, возникающие у больных с тяжелой, молниеносной пневмонией и/или с острым респираторным дистресс-синдромом. Предрасполагающие факторы, они же предикторы, — пожилой и старческий возраст, патология сердца (миокардит, инфаркт миокарда, кардиомиопатия), фибрилляция предсердий, интубация, ИВЛ, нестабильность системной гемодинамики, эндотелиальная дисфункция, прокоагулянтная активность, резкое возрастание уровня мозгового натрийуретического пептида B-типа, его предшественника NT-proBNP, сердечных тропонинов, D-димера, фибрина, наличие атеросклеротических бляшек, локального или тандемного стеноза магистральных артерий шеи и головы [174–181]. Разнообразие патогенетических механизмов определяет гетерогенность клинических форм инсульта. В генезе эмболического инсульта (кардиоэмболический подтип) главенствующая роль принадлежит поступлению в сосудистую сеть головного мозга эмболического материала из камер сердца при эндотелиальном воспалении, нарушении сократительной способности миокарда, тахисистолической форме мерцательной аритмии [182, 183]. Соматическое обследование и данные аутопсии свидетельствуют о максимальной представленности этих форм патологии у инфицированных SARS-CoV-2 больных. Развитие окклюзии магистральных экстракраниальных или интракраниальных сосудов происходит на фоне тяжелой пневмонии, иммобилизации больного, активации процесса тромбообразования, резистентности к гепарину и антиагрегантной терапии [184–187]. Риск возникновения ишемического инсульта, тран-зиторных ишемических атак, тромбоза синусов и вен головного мозга при респираторных инфекциях возрастает в несколько раз [20, 179]. Сочетание венозных и артериальных тромботических осложнений — характерная черта критических состояний [6, 181]. Установлена связь многоочагового поражения мозга с васкулокоагулопатией и антифосфолипидными антителами (к кардиолипину, β2-гликопротеину I, IgA и IgG) [188, 189]. При аутопсии церебральные инфаркты обнаруживаются у 15,4% больных, инфаркт миокарда — у 19,2% [183]. Использование современных методов визуализации повышает уровень выявляемости тром- боза церебральных сосудов (артерий и вен) [67, 190–193], сердца, легочной артерии, глубоких вен конечностей, но в ряде случаев при отрицательных данных первой оценки возникает необходимость в повторном исследовании [194]. О наличии гиперкоагуляции свидетельствуют снижение активированного частичного тромбопластинового времени крови, увеличение протромбинового индекса, значительное возрастание уровня D-димера, фибрина — наиболее значимого маркера локального и системного тромбоза [185, 195].
Облигатные для ишемического инсульта очаговые симптомы развиваются до (редко) или в ближайшие дни от начала заболевания [4, 10, 172, 179, 196]. Их семиотика зависит от области локализации нарушенного кровоснабжения. По данным КТ, КТ-перфузии, МРТ, МРТ-ангиографии вскрытия умерших, образование инфарктов мозга связано с окклюзией внутренней сонной, средней мозговой, позвоночной, основной или задней мозговой артерии (эмболический, атеротромботический подтип инсульта) [21, 67, 186, 194, 196, 197]. Прогноз определяется не столько размером ишемии (исключение — обширные инфаркты), сколько особенностями течения основного заболевания [176, 184, 187, 198]. Анализ обращений в скорую помощь (2010–2020 гг.) не подтвердил первые впечатления об уменьшении числа больных с острыми нарушениями мозгового кровообращения. Транзиторные ишемические атаки и инсульты развиваются независимо от того, инфицирован больной или нет. Заболевание COVID-19 является значимым фактором риска возникновения цереброваскулярных осложнений. Их неблагоприятный исход наблюдается при нарастании гипоксемии, развитии сепсиса, синдрома полиорганной недостаточности, диссеминированного внутрисосудистого свертывания [185 , 199]. Лечение и реабилитация больных с ишемическими инсультами проводится согласно принятым международным и республиканским протоколам терапии цереброваскулярных заболеваний с использованием системного тромболизиса, механической тромбэктомии и мер предупреждения заражения медицинского персонала. Описан случай заражения больного от лечащего врача [172, 179, 185, 200–202]. Те же правила и рекомендации следует соблюдать при диагностике (КТ, МРТ, допплерография, ангиография), выполнении хирургических вмешательств [203, 204].
В инициации геморрагических осложнений, в частности геморрагического инсульта, первостепенное значение отводится нарушениям гемостаза, проницаемости гемовазального барьера при воспалительной васкулопатии и неконтролируемой артериальной гипертензии [65, 205]. Присутствие вируса SARS-CoV-2 в ЦСЖ с помощью ПЦР не констатируется [67, 206], при SARS-CoV-1 его удалось обнаружить как в ликворе, так и в мозге [130, 198].
Особенностью клинических проявлений интрацеребрального кровоизлияния, геморрагического инфаркта при тромбозе внутримозговых синусов является преобладание общемозговых симптомов над очаговыми [184, 185, 207]. Отрицательные результаты КТ-, МРТ-обследования не исключают обнаружения эритроцитов и ксантохромии в ликворе. Выполнение люмбальной пункции при негативных данных нейровизуализации обязательно! Наличие высокой температуры, симптомов раздражения мозговых оболочек делает необходимым проведение дифференциального диагноза с инфекционным менингитом [206], но, к сожалению, в условиях пандемии нозологическая форма возникающих осложнений определяется часто без люмбальной пункции и исследования ликвора. Правильный диагноз становится очевидным только после проведения аутопсии.
Энцефалопатии критических состояний
Большая часть больных, находящихся в палатах интенсивной терапии и реанимационных отделениях, имеют фоновые заболевания, по поводу которых они на протяжении многих лет до поступления в больницу получали лечение в поликлиниках и терапевтических стационарах. Наличие коморбид-ных форм патологии при COVID-19 определяет не только выбор лекарственных средств, но и прогноз, исход осложнений, возникающих на любом этапе их развития, что важно для проведения персонализированной терапии, адекватной ситуации [208]. В группу высокого риска входят больные хроническими заболеваниями легких (бронхит, хроническая обструктивная болезнь легких), сердечно-сосудистой системы (гипертоническая болезнь и симптоматическая артериальная гипертензия, ишемическая болезнь сердца, кардиомиопатия), почек, нервной, мышечной системы, а также с сахарным диабетом, онкопатологией [209]. Основными причинами смерти больных являются обусловленные «цитокиновым штормом» острый респираторный дистресс-синдром, сочетание дыхательной и сердечной недостаточности, септический шок, множественные тромбозы вследствие коагулопатии, полиорганная недостаточность [210–213]. Каскад взаимосвязанных и взаимно усугубляющих друг друга патологических процессов оказывает отрицательное влияние на головной мозг, инициируя нарушения микроциркуляции и функционирования нейрональной сети, проводящих путей, синаптического аппарата на корковом, подкорковом и стволовом уровнях. Реакция церебральных структур на вирусную инвазию, прогрессирующую гипоксию, ишемию тканей неспецифична, определяется включением компенсаторных резервов и адекватностью патогенетической терапии. Недостаточность, отсутствие эффективного реагирования саногенети-ческих механизмов, организационные, диагностические, лечебно-тактические ошибки по неведению становятся причинами нарушения соматического и/ или психоневрологического статуса. Характерные для энцефалопатии симптомы в виде изменения поведения, понимания речи, обнубиляции, пом-рачнения сознания (сопор, кома), эпилептических приступов/статуса, психомоторного возбуждения, бреда, дезориентировки во времени, окружающей обстановке, но не в личности (гиперактивный, «тихий» делирий), могут возникнуть на любом этапе заболевания, но чаще при неэффективности терапии, являясь предвестником летального исхода [14, 24, 26, 29, 207, 213–215]. У половины больных старше 60 лет, находящихся в стационаре, и у 80% пациентов на фоне проведения ИВЛ развивается делирий [214]. Его возникновение возможно до появления признаков респираторной инфекции, при их наличии — во время лечения (> 20%), в палате интенсивной терапии, реанимационном отделении (> 50%), из них у 1/2 — в гипоактивной форме [215–218]. Прогностическая значимость психотических нарушений примерно в 75% случаев , к сожалению, не оценивается должным образом медперсоналом. То же относится и к провоцирующим факторам — изоляции (социальной, физической, сенсорной), когнитивным нарушениям, длительной иммобилизации, респираторной поддержке, назначению антихолинергических препаратов, гип-нотиков, бензодиазепинов, антипсихотиков, кроме указанных в рекомендациях (дексмедетомидин по 0,2–1,4 мкг/кг в час, галоперидол не более 6 мг/сут) [173, 215, 219, 220]. Использование психометрических шкал (RASS, DRS, DRS-R-98, ICDSC, CAM-ICU, Nu-DESC, CAM-ICU), обладающих высокой чувствительностью и специфичностью, позволяет своевременно диагностировать тип делирия, определить степень его тяжести, эффективно в короткие сроки купировать угрожающее жизни больного осложнение, характеризующее дисфункцию нейроме-
<линическая’2п20 п эакти ка Том 11 №2
диаторных систем (снижение уровня ацетилхолина и мелатонина, повышение дофамина) [221–223].
Судорожный синдром представлен различными типами приступов — генерализованным/мультифо-кальным миоклонусом, частыми билатеральными тонико-клоническими судорогами, конвульсивным, бессудорожным эпилептическим статусом [29, 46, 224, 225]. При анализе причин их развития необходимо учитывать не только роль гипоксии, воспаления, метаболических, водно-электролитных нарушений, но и прекращение больным лечения в связи с отсутствием принимаемых постоянно антиконвульсантов, их заменой, несовместимостью с назначенными по поводу COVID-19 препаратами, а также другими причинами или изменением их фармакокинетики на фоне полиорганной патологии [31–33, 222, 226–229].
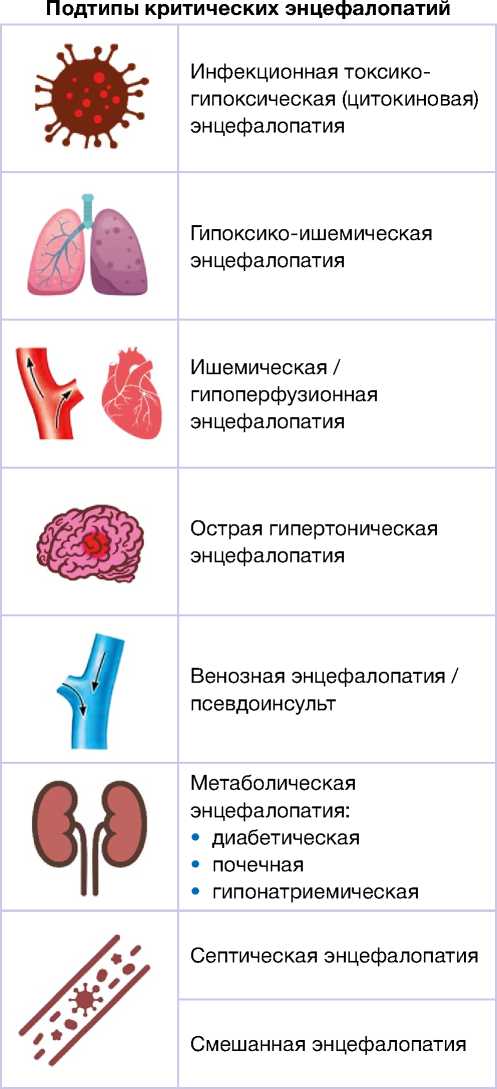
Форма и клинические проявления церебральной дисфункции индивидуальны для каждого больного, первопричиной служат соматические, иммунные, гемодинамические, реже метаболические нарушения, цитокиновая «буря», сепсис [229–231] (табл. 1). При осмотре пациента признаки, свидетельствующие о наличии очагового неврологического дефицита, обычно не определяются. По данным КТ, МРТ, структурные изменения в белом и сером веществе головного мозга отсутствуют [199, 229], за исключением случаев ангиита (васкулита), лейкоэнцефалопатии, острой некротической энцефалопатии/геморрагического, параинфекци-онного NMDAR-энцефалита [52, 232–234]. Частыми находками являются лобно-височная гипоперфузия, перивентрикулярный отек, сдавливание боковых желудочков мозга, стертость границ между корой и белым веществом, сужение/исчезновение субарахноидальных пространств, базальных цистерн. Данные морфологического исследования свидетельствуют о схожести поражения нейронов, олигодендроглии, эндотелия кровеносных сосудов при всех формах энцефалопатий, независимо от их генеза [235]. На ЭЭГ регистрируются неспецифические изменения [199]. Ликвор не изменен, тест на коронавирус обычно отрицателен, но на аутопсии его присутствие в нейронах мозга выявить вполне возможно [45, 46, 229, 236]. Разрушительное, порой необратимое действие на структуры мозга (паренхиму, базальные ядра, ромбэнцефалон) и питающие их сосуды оказывают цитокиновое воспаление и стремительное накопление в клетках ферритина [237]. При нейровизуализации и аутопсии в этих случаях, помимо цитотоксического, вазогенного
Таблица 1
отека, обнаруживаются периваскулярные клеточные инфильтраты, пролиферация макро- и микроглии, очаги демиелинизации, кровоизлияния, некроз, расплавление вещества мозга. Максимальные изменения находят в диэнцефальной области, таламусе, височных долях, а также в структурах, наиболее уязвимых к гипоксии-ишемии. Избирательное поражение серого и белого вещества в виде отечной некротической геморрагической энцефалопатии — не уникальное явление, свойственное только COVID-19: аналогичное поражение мозга описано при микробных и вирусных инфекциях, сепсисе, шоке, гемофагоцитарном лимфо-гистоцитозе, болезни Стилла, остановке сердца, длительном апноэ, пролонгированной реанимации, перинатальной тяжелой гипоксии, телэнцефаль-ном глиозе у новорожденных [77, 78, 237, 238]. Выход из длительной комы при любой форме энцефалопатии чреват развитием тяжелых когнитивных, двигательных, речевых нарушений.
НЕЙРОИНВАЗИВНОСТЬ
И НЕЙРОВИРУЛЕНТНОСТЬ ВИРУСА SARS-CoV-2
Оценка клинических исследований и экспериментальных данных свидетельствует о том, что возбудители острых респираторных инфекций — бетакоронавирусы МЕRS-CoV, SARS-CoV и SARS-CoV-2 — имеют тропность не только к эпителиоцитам легких, но при вирусемии могут вызывать поражение других органов и систем [175, 236, 239–242]. Очередность проникновения в клетки конкретного органа определяется эффективностью его систем защиты и организма человека в целом. Великий французский микробиолог Луи Пастер в начале ХХ в. прозорливо заметил: «Микроб ничто, почва все» [243]. Это объясняет, почему у одних заболевание протекает асимптомно, у других — в легкой форме, а у многих, преимущественно пожилых, отягощенных хроническими заболеваниями, — тяжело и даже стремительно, заканчиваясь летальным исходом. Симптомы поражения периферической и центральной нервной системы могут предшествовать инфекционным, возникать, согласно анамнестическим данным, одновременно или на фоне развития и прогрессирования дыхательной и/или сердечно-сосудистой недостаточности. Но есть особенность, не свойственная другим респираторным вирусным инфекциям: у подавляющей части больных дисфункция краниальных нервов, иннервирующих носоглотку и полость рта, предшествует церебральным расстройствам. Другая особенность заключается в том, что потеря сознания, кома и клинические проявления острого респираторного синдрома могут возникнуть при отсутствии лихорадки, пневмонии и симптомов поражения верхних дыхательных путей. Многие вирусы и бактерии внедряются в организм человека через слизистые оболочки глаз, носа, носоглотки, но не все поражают рецепторный аппарат, терминальные ветви краниальных нервов, структуры ЦНС. Например, при лепре головной мозг и легкие остаются интактны- ми, при гриппе, коронавирусной инвазии основной мишенью являются верхние и нижние дыхательные пути.
В литературе рассматривается несколько причин поражения нервной системы:
-
• прямое избирательное воздействие вируса на краниальные нервы и ткань мозга;
-
• выработка вирусом нейротоксинов;
-
• активация вирусом нейромедиаторов воспаления;
-
• перемещение вируса в эндотелий церебральных сосудов, внедрение в структуры мозга;
-
• вторичное повреждение вследствие развития острого, подострого аутоиммунного процесса.
При контактном, воздушно-капельном заражении вирусы, внедряясь и размножаясь в эпителиальных клетках носовой полости, носоглотки, по аксонам терминальных ветвей «мигрируют» в нейроны I, V, VII пары черепно-мозговых нервов (рис. 2) [244]. Преградой на их пути к оболочкам и структурам головного мозга становится локальный иммунный контроль на территории взаимодействия вируса с рецепторами ангиотензинпревращающе-го фермента (ACE2) и TMPRSS2. С помощью белка шипов S SARS-CoV-2 фиксируется к клеткам, фу-рин и TMPRSS2 протеаза способствуют его проникновению внутрь [45, 85, 245, 246]. Возникшие на стадии инициации апоптоза нарушения обоняния и вкуса у большей части больных обратимы. В связи с большей экспрессией гена ACE2 в нижних дыхательных путях агрессии SARS-CoV-2 становятся подвержены легкие [247, 248]. При недостаточной активации автономного клеточного и гуморального ответа, мутации G758R в белке S, модифицирующей вирусное распространение и нейровирулентность, вирусы и вторичные продукты их жизнедеятельности (токсины) могут проникнуть через гематоэнцефалический барьер в сосудистую систему, оболочки, кору головного мозга, базальные ганглии, ствол мозга [249–251]. Преимущественно страдают сосуды микроциркуляторного русла, обеспечивающие кровоснабжение зрительных бугров, субкортикальных, перивентрикулярных областей белого вещества больших полушарий, что находит подтверждение при нейровизуализации в виде некроза (энцефалолизиса), макро- и микрокровоизлияний, лейкоэнцефалопатии (поражении мозолистого тела, белого вещества лобных и височных долей). О преодолении вирусом гематоэнцефалического барьера свидетельствуют данные аутопсии (обнаружение РНК SARS-CoV-2 в паренхиме мозга и ликворе с помо-
<линическая’2п20 п эакти ка Том 11 №2
Рис. 2. Поражение сенсорных ветвей n. vagus , базальных ядер и ствола мозга при COVID-19
Краниальн
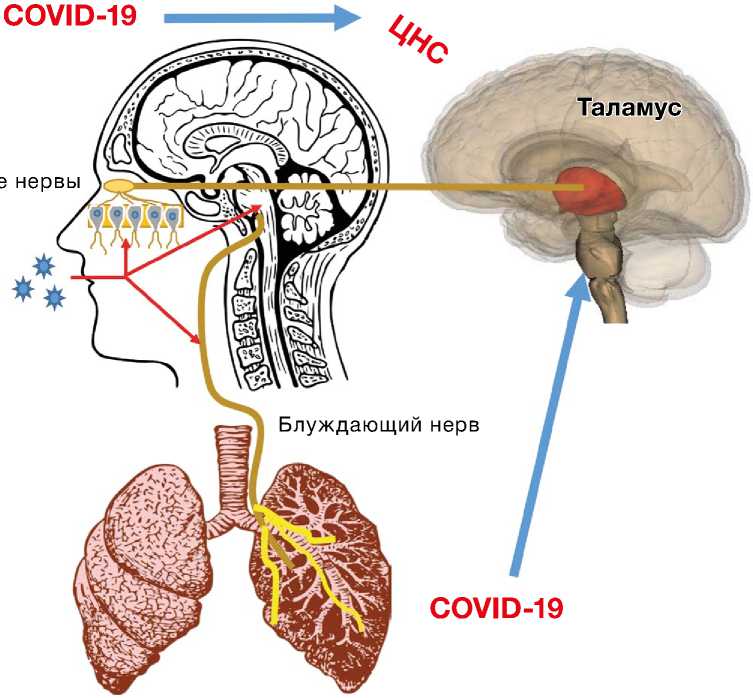
щью ПЦР) [45, 46, 252, 253]. Аналогичная динамика развития патологического процесса и, поразительно, в те же сроки, как и у людей, наблюдается при заражении экспериментальных животных коронавирусами другого типа. В частности, при назальном вдыхании, инокуляции HCoV-OC43, MERS-CoV-13, SARS-CoV, SARS-CoV-34 вирусы были обнаружены через несколько суток сначала в обонятельной луковице, затем последовательно в грушевидной (обонятельной) коре, таламусе, стволе, спинном мозге [254, 255]. Прерывание распространения вируса путем абляции на уровне обонятельной луковицы делало невозможным его инвазию в мозговые нейроны [256]. Продвижение к «мишени» по краниальным и блуждающему нерву осуществляется по аксону и дендритам ретроградно, антероградно, транссинаптически [27, 65, 257–259]. Возникающие при коронавирусной нейроинвазии морфологические и клинические проявления, органные и системные, независимо от типа вируса, вида животного, имеют сходство с теми, что наблюдаются при атипичной пневмонии MERS, остром респираторном синдроме SARS, COVID-19 в том числе. Это касается не толь- ко форм поражения головного, спинного мозга, периферических нервов, нервно-мышечного аппарата, но и структурных изменений, выявляемых при нейровизуализации и аутопсии [9, 10, 245, 260–265].
Если клеточные механизмы защиты тканей и интерфероны на начальном этапе инфицирования не срабатывают, происходит локальное, а затем и системное усиление продукции хемокинов и анти-воспалительных цитокинов, негативной стороной действия которых является цитопатическое повреждение клеток «мишени» вследствие аутоантигенной агрессии [27, 266]. Возникший воспалительный «цитокиновый шторм» вызывает иммунопатоген-ное повреждение тканей и органов [2, 80, 130, 171, 267–269]. Клиническим проявлением тканевой альтерации на начальном этапе становятся катаральные симптомы, лихорадка, утомляемость, миалгии, повреждение альвеолярных эпителиальных клеток легкого (падение сатурации, респираторный синдром), кардиомиоцитов (кардиалгия, аритмии), лептоменикса (менингеальные симптомы), глии и нейронов мозга (психические нарушения, эпилептические приступы, потеря сознания из-за прогрессирования цитотоксического и вазогенного отека мозга). Вторичное повреждение коры, белого вещества больших полушарий, мозжечка, базальных ядер связано с гипоксией, ишемией мозга, изменениями метаболизма при пневмонии, анемии, остром миокардите, кардиомиопатии, вариабельности систолического артериального давления, сепсисе, шоке, гипергликемии, водно-электролитном дисбалансе. Причиной цереброваскулярных осложнений являются эндотелиальная дисфункция, внутрисосудистая коагуляция, кардиальная, артерио-артериальная эмболия, гипертонические кризы, срыв ауторегуляции церебральных сосудов, малые и фатальные кровоизлияния при проведении лекарственной терапии. Острый респираторный дистресс-синдром — следствие не только воспалительной клеточной инфильтрации, отека, фиброза легких, но и гиперактивности нейронов дыхательного центра. Критическое состояние и смерть могут быть ассоциированы с первичным поражением легочной ткани и ствола мозга [131, 132, 258, 266, 270]. Проникновение вирусов в ядра (n. solitarius, n. ambiguus) и комплекс Бетцингера дыхательного центра, получающих информацию от хеморецепторов о содержании в крови O2, CO2, регулирующих глубину, ритм дыхания, возможно по сенсорным волокнам блуждающего нерва и микроциркуляторной сети [129]. Причем в низкой концентрации коронавирусы при интраназальном введении животным попадают только в мозг [271]. При вирусемии РНК и белки MERS-CoV, SARS-CoV, SARS-CoV-2 определяются в верхних дыхательных путях, легких, стволе мозга, таламусе, гипоталамусе, гиппокампе, корковых извилинах лобной, височной доли, гипофизе, щитовидной, паращитовидной железе, внутренних, репродуктивных органах, потовых железах, спинномозговой жидкости [10, 263, 268, 272]. Для фиксации в нервных окончаниях, глиальных клетках, нейронах SARS-CoV-2 использует рецепторы ACE2 и фермент TMPRSS2, экспрессия которых обнаружена в эндотелии сосудов и мозге [85, 134, 251, 269]. Носители мутаций в гене, кодирующем белок RANBP2 (Ran Ran Binding Protein 2), составляют группу риска развития острой некротической энцефалопатии, ассоциированной с респираторной инфекцией [273, 274].
Генетическая предрасположенность, гибель олигодендроцитов, нервных клеток и их отростков, активация микроглии, цитокинов (фактор некроза опухоли альфа, IL4, IL10), аутосенсибилизирован- ных клонов (CD4+, Th1, Th17 клеточного иммунного ответа), молекулярная мимикрия — значимые факторы инициации демиелинизации в центральной и периферической нервной системе во время инфицирования и пребывания больного в стационаре [275]. Многообразие механизмов, вовлечение различных структур определяет разнообразие клинических форм в широком диапазоне — от лейкоэнцефалопатии, энцефалита, поперечного миелита до основных и атипичных вариантов синдрома Гий-ена–Барре. Представленная «палитра» осложнений не зависит от типа коронавируса, возраста, наличия у больного предшествующих коморбидных форм патологии.
Еще одна не менее важная проблема — вирусная нейроинвазия — способствует развитию обострений и прогрессированию приобретенных (миастения, рассеянный склероз, оптикомиелит, воспалительные, аутоиммунные, парапротеинемические хронические полиневропатии), наследственных демиелинизирующих, метаболических, нейродеге-неративных и нервно-мышечных заболеваний [165, 276–281]. Ее решение требует объединения общих усилий врачей и исследователей во всех странах мира. Первые шаги уже сделаны [6, 282–284]: Европейской академией неврологии создана многопрофильная целевая группа EANcore COVID-19 для разработки рекомендаций по диагностике и лечению больных COVID-19; с мая 2020 года при поддержке национальных обществ ведется международный реестр стандартизированной информации обо всех проявлениях, осложнениях заболевания, их исходах, течении в последующие годы. Актуальность и практическая значимость международного сотрудничества с участием отечественных неврологов в этой области знаний очевидны.
ЗАКЛЮЧЕНИЕ
Спектр неврологических нарушений при COVID-19 весьма широк — от краниальных мононевропатий, клинически проявляющихся в виде аносмии, агевзии/дисгевзии и др., до острой воспалительной полинейропатии Гийена–Барре и тяжелых поражений головного и спинного мозга в виде острой геморрагической некротизирующей энцефалопатии и миелопатий. С точки зрения патогенеза, неврологические нарушения при COVID-19 могут быть обусловлены гипоксемией, нарушениями гомеостаза (энцефалопатия критических состояний), нейротропностью и нейровирулентностью SARS-CoV-2 (изолированное поражение клиническая; 20
Том 121 № 0 2
черепных нервов, очаговые и диффузные поражения ЦНС), «цитокиновым штормом», а также смешанным воздействием перечисленных факторов. COVID-19 влияет на течение хронических неврологических заболеваний, особенно связанных с ней-роиммунными нарушениями. Все перечисленное определяет необходимость мультидисциплинарно-го подхода к лечению COVID-19 и его осложнений с обязательным участием специалиста-невролога.
ИСТОЧНИК ФИНАСИРОВАНИЯ
Часть аналитического обзора, выполненная Е.М. Самойловой, была сделана при финансовой поддержке гранта РФФИ 19-29-01090.
Список литературы Поражение нервной системы при СOVID-19
- Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):1-9. DOI: 10.1001/jamaneurol.2020.1127
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. DOI: 10.1016/S0140-6736(20)30183-5
- Dalakas MC. Guillain-Barré syndrome: The first documented COVID-19-triggered autoimmu-ne neurologic disease: More to come with myositis in the offing. Neurol Neuroimmunol Neuroinflamm. 2020;7(5):e781. DOI: 10.1212/NXI.0000000000000781
- Sellner J, Taba P, Öztürk S, Helbok R. The need for neurologists in the care of COVID-19 patients. Eur J Neurol. 2020;. DOI: 10.1111/ene.14257
- Jin M, Tong Q. Rhabdomyolysis as potential late complication associated with COVID-19. Emerg Infect Dis. 2020;26(7):1618-1620. DOI: 10.3201/eid2607.200445
- Román GC, Spencer PS, Reis J, et al. The neurology of COVID-19 revisited: a proposal from the environmental neurology specialty group of the world federation of neurology to implement international neurological registries. J Neurol Sci. 2020;414:116884.
- DOI: 10.1016/j.jns.2020.116884
- Sepehrinezhad A, Shahbazi A, Negah SS. COVID-19 virus may have neuroinvasive potential and cause neurological complications: a perspective review. J Neurovirol. 2020;26(3):324-329.
- DOI: 10.1007/s13365-020-00851-2
- Robinson CP, Busl KM. Neurologic manifestations of severe respiratory viral contagions. Crit Care Explor. 2020;2(4):e0107.
- DOI: 10.1097/CCE.0000000000000107
- Vonck K, Garrez I, De Herdt V, et al. Neurological manifestations and neuroinvasive mechanisms of the severe acute respiratory syndrome Coronavirus Type 2. Eur J Neurol. 2020;.
- DOI: 10.1111/ene.14329
- Tsai ST, Lu MK, San S, Tsai CH. The Neurologic Manifestations of Coronavirus Disea-se 2019 Pandemic: A Systemic Review. Front Neurol. 2020;11:498. doi: 10.33 9/fneur.2020.00 498.
- Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720.
- DOI: 10.1056/NEJMoa2002032
- Giacomelli A, Pezzati L, Conti F, et al. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross sectional study. Clin Infect Dis. 2020;ciaa330.
- DOI: 10.1093/cid/ciaa330
- Liguori C, Pierantozzi M, Spanetta M, et al. Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection. Brain Behav Immun. 2020;S0889-1591(20)30876-X.
- DOI: 10.1016/j.bbi.2020.05.037
- Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611-627.
- DOI: 10.1016/S2215-0366(20)30203-0
- Мосолов С.Н. Проблемы психического здоровья в условиях пандемии COVID-19 // Журнал неврологии и психиатрии им. С.С. Корсакова. - 2020. - Т.120. - №5. - С. 7-15.
- DOI: 10.17116/jnevro20201200517
- Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34-39.
- DOI: 10.1016/j.bbi.2020.04.027
- Galea S, N. The mental health consequences of COVID-19 and physical distancing. The need for prevention and early intervention. JAMA Intern Med. 2020.
- DOI: 10.1001/jamainternmed.2020.1562
- Colizzi M, Bortoletto R, Silvestri M, Mondin F. Medically unexplained symptoms in the times of Covid-19 pandemic: A case-report. Brain Behav Immun Health. 2020;5:100073. 10.1016/ j.bbih.2020.100073.
- DOI: 10.1016/j.bbih.2020.100073
- Asadi-Pooya AA, Simani L.Central nervous system manifestations of COVID-19: A systematic review. J Neurol Sci. 2020;413:116832.
- DOI: 10.1016/j.jns.2020.116832
- Ahmad I, Rathore FA. Neurological manifestations and complications of COVID-19: A literatu-re review. J Clin Neurosci. 2020;77:8-12.
- DOI: 10.1016/j.jocn.2020.05.017
- Li Y, Wang M, Zhou Y, et al. Acute cerebrovascular disease following COVID-19: a single, retrospective, observational study. Lancet. 2020.
- DOI: 10.2139/ssrn.3550025
- Mahammedi A, Saba L, Vagal A, et al. Imaging in neurological disease of hospitalized COVID-19 patients. An Italian multicenter retrospective observational study. Radiology. 2020:201933.
- DOI: 10.1148/radiol.2020201933
- Guillan M, Villacieros-Alvarez J, Bellido S, Perez-Jorge Peremarch C. et al. Unusual simultaneous cerebral infarcts in multiple arterial territories in a COVID-19 patient. J.Thromb Res. 2020 Jun 9;193:107-109.
- DOI: 10.1016/j.thromres.2020.06.015
- Lu L, Xiong W, Liu D, Liu J. et al. Newonset acute symptomatic seizure and risk in Coronavirus Diseases 2019: A retrospective multicenter study. Epilepsia. 2020;61(6):e49-e53. 10.1111/ epi.16524.
- DOI: 10.1111/epi.16524
- Le Guennec L, Devianne J, Jalin L, Cao A, Galanaud D, Navarro V, Boutolleau D, Rohaut B, Weiss N, Demeret S. Orbitofrontal involvement in a neuroCOVID-19 patient. Epilepsia. 2020.
- DOI: 10.1111/epi.16612
- Fasano A, Cavallieri F, Canali E, Valzania F. First motor seizure as presenting symptom of SARS-CoV-2 infection. Neurol Sci. 2020:1-3.
- DOI: 10.1007/s10072-020-04460
- Zubair AS, McAlpine LS, Gardin T, et al. Neuropathogenesis and neurologic manifestations of the Coronaviruses in the age of Coronavirus disease 2019: A review. JAMA Neurol. 2020.
- DOI: 10.1001/jamaneurol.2020.2065
- Elgamasy S, Kamel MG, Ghozy S, et al. First case of focal epilepsy associated with sars-coronavirus-2. J Med Virol. 2020;.
- DOI: 10.1002/jmv.26113
- Hepburn M, Mullaguri N, George P, et al. Acute symptomatic seizures in critically Ill patients with COVID-19: Is there an association? Neurocrit Care. 2020;1-5.
- DOI: 10.1007/s12028-020-01006-1
- Kuroda N. Epilepsy and COVID-19: Associations and important considerations. Epilepsy Behav. 2020;108:107122.
- DOI: 10.1016/j.yebeh.2020.107122
- Карлов В.А., Бурд С.Г., Лебедева А.В., и др. Эпилепсия и COVID-19. Тактика и лечение. Рекомендации Российской противоэпилептической лиги // Эпилепсия и пароксизмальные состояния. - 2020. - Т.12. - №1. - С. 84-88.
- DOI: 10.17749/2077-8333.2020.12.1.84-88
- Karimi N, Sharifi Razavi A, Rouhani N. Frequent convulsive seizures in an adult patient with COVID-19: A case report. Iran Red Crescent Med J. 2020;22(3):e102828.
- DOI: 10.5812/ircmj.102828
- Холин A.A., Заваденко Н.Н., Холина Е.A. Международные рекомендации по ведению пациентов с эпилепсией в условиях пандемии COVID-19 (по материалам ILAE) // РМЖ. Неврология. - 2020. - №8. - С. 2-4.
- Moriguchi T, Harii N, Goto J, et al. A first case of menin-getis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55-58.
- DOI: 10.1016/j.ijid.2020.03.062
- Ye M, Ren Y, Lv T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav Immun. 2020;S0889-1591(20)30465-7.
- DOI: 10.1016/j.bbi.2020.04.017
- Bernard-Valnet R, Pizzarotti B, Anichini A, et al. Two patients with acute meningoencephalitis concomitant to SARS-CoV-2 infection. Eur J Neurol. 2020;10.1111/ene.
- DOI: 10.1111/ene.14298
- Dogan L, Kaya D, Sarikaya T, et al. Plasmapheresis treatment in COVID-19-related autoimmune meningoencephalitis: case series. Brain Behav Immun. 2020;87:155-158.
- DOI: 10.1016/j.bbi.2020.05.022
- Duong L, Xu P, Liu A. Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in downtown Los Angeles, early april 2020. Brain Behav Immun. 2020;7:33.
- DOI: 10.1016/j.bbi.2020.04.024
- Lovati C, Osio M, Pantoni L. Diagnosing Herpes simplex-1 Encephalitis at the Time of COVID-19 pandemic. Neurol Sci. 2020;41(6):1361-1364.
- DOI: 10.1007/s10072-020-04461-y
- Lu X, Zhang L, Du H, et al. SARS-CoV-2 infection in children. N Engl J Med. 2020:382(17):1663-1665.
- DOI: 10.1056/NEJMc2005073
- McAbee GN, Brosqol Y, Pavlakis S, et al. Encephalitis assоciated with COVID-19 infection in 11 year-old child. Pediatric Neurology. 2020.
- DOI: 10.1016/j.pediatrneurol.2020.04.013
- Perchetti GA, Nalla AK, Huang M-L, et al.Validation of SARS-CoV-2 detection across multiple specimen types. J Clin Virol. 2020;128:104438.
- DOI: 10.1016/j.jcv.2020.104438
- Al-Olama M, Rashid A, Garozzo D. COVID-19-associated Meningoencephalitis complicated with intracranial hemorrhage: a case report. Acta Neurochir (Wien). 2020;162(7):1495-1499.
- DOI: 10.1007/s00701-020-04402-w
- Gu J, Gong E, Zhang B, et al. Multiple organ infection and the pathogenesis of SARS. J Exp Med. 2005;202(3):415-424.
- DOI: 10.1084/jem.20050828
- Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other Coronaviruses. Brain Behav Immun. 2020;87:18-22.
- DOI: 10.1016/j.bbi.2020.03.031
- Hung EC, Chim SS, Chan PK, et al. Detection of SARS coronavirus RNA in the cerebrospinal fluid of a patient with severe acute respiratory syndrome. Clin Chem. 2003;49(12):2108-2109.
- DOI: 10.1373/clinchem.2003.025437
- Zhang QL, Ding YQ, Hou JL, et al. Detection of severe acute respiratory syndrome (SARS)-associated coronavirus RNA in autopsy tissues with in situ hybridization. Di Yi Jun Yi Da Xue Xue Bao. 2003;23(11):1125-1127.
- Pilotto A, Odolini S, Masciocchi SS, et al. Steroid-responsive Encephalitis in Covid-19 disease. Ann Neurol. 2020;.
- DOI: 10.1002/ana.25783
- Arbour N, Day R, Newcombe J, Talbot PJ. Neuroinvasion by human respiratory Coronaviruses. J Virol. 2000;74(19):8913-8921.
- DOI: 10.1128/jvi.74.19.8913-8921.2000
- Lau K-K, Yu W-C, Chu C-M, et al. Possible central nervous system infection by SARS coronavirus. Emerg Infect Dis. 2004;10(2):342-344.
- DOI: 10.3201/eid1002.030638
- Tsai LK, Hsieh ST, Chang YC. Neurological manifestations in severe acute respiratory syndrome. Acta Neurol Taiwan. 2005;14(3):113-119.
- Panariello A, Bassetti R, Radice A, et al. Anti-NMDA receptor encepha-litis in a psychiatric Covid-19 patient: a case report. Brain Behav Immun. 2020;87:179-181.
- DOI: 10.1016/j.bbi.2020.05.054
- Yashavantha Rao HC, Jayabaskaran C. The emergence of a novel Coronavirus (SARS-CoV-2) disease and their neuroinvasive propensity may affect in COVID-19 patients. J Med Virol. 2020;92(7):786-790.
- DOI: 10.1002/jmv.25918
- Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-1034.
- DOI: 10.1016/S0140-6736(20)30628-0
- Hoshino A, Saitoh M, Oka A, et al. Epidemiology of acute ence-phalopathy in japan, with emphasis on the association of viruses and syndromes. Brain Dev. 2012;34(5):337-343.
- DOI: 10.1016/j.braindev.2011.07.012
- Bohmwald K, Galvez N, Ríos M, Kalergis AM. Neurologic alterations due to respiratory virus infections. Front Cell Neurosci. 2018;12:386.
- DOI: 10.3389/fncel.2018.00386
- Чучин М.Ю. Острая некротическая энцефалопатия при вирусной инфекции // Детская больница. - 2012. - №1. - С. 23-28.
- Mizuguchi M, Yamanouchi H, Ichiyama T, Shiomi M. Acute encephalopathy associated with influenza and otherviral infections. Acta Neurol Scand. 2007;115(4Suppl):45-56.
- DOI: 10.1111/1600-0404.2007.00809.x
- Araujo R, Gouveia P, Fineza I. Bilateral thalamic lesions in acute necrotizing encepha-lopathy due to H1N1 infection visual diagnosis. Pediatr Neurol. 2016;65:96-97.
- DOI: 10.1016/j.pediatrneurol.2016.08.008
- Meijer WJ, Linn FH, Wensing AM, et al. Acute influenza virus-associated encephalitis and encephalopathy in adults: a challenging diagnosis. JMM Case Reports. 2016;3(6):e005076.
- DOI: 10.1099/jmmcr.0.005076
- Иванова Г.П. Лейкоэнцефалиты у детей: дифференциально-диагностические, патогенетические и терапевтические аспекты: Автореф. дис. … докт. мед. наук. - СПб., 2012. - 44 с. Доступно по: https://search.rsl.ru/ru/record/01005012368. Ссылка активна на 14.02.2020.
- Desforges M, Le Coupanec A, Dubeau P, et al. Human Coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? viruses. 2019;12(1):14.
- DOI: 10.3390/v12010014
- Das G, Mukherjee N, Ghosh S. Neurological insights of COVID-19 pandemic. ACS Chem Neurosci. 2020:11(9):1206-1209.
- DOI: 10.1021/acschemneuro.0c00201
- Dixon L, Varley J, Gontsarova A, Mallon D, et al. COVID-19-related acute necrotizing encephalopathy with brain stem involvement in a patient with aplastic anemia. Neurol Neuroimmunol Neuroinflamm. 2020;7(5):e789.
- DOI: 10.1212/NXI.0000000000000789
- Cardona GC, Quintana Pájaro LD, Quintero Marzola GC, et al. Neurotropism of SARS-CoV 2: mechanisms and manifestations. J Neurol Sci. 2020;412:116824.
- DOI: 10.1016/j.jns.2020.116824
- Radmanesh A, Derman A, Lui YW, et al. COVID-19-associated diffuse leukoencephalopathy and microhemorrhages. Radiology. 2020;202040. doi: 10.11-48/radiol.2020202040.
- Kandemirli SG, Dogan L, Sarikaya ZT, et al. Brain MRI findings in patients in the intensive care unit with COVID-19 infection. Radiology. 2020;201697.
- DOI: 10.1148/radiol.2020201697
- Novi G, Rossi T, Pedemonte E, et al. Acute disseminated encephalomyelitis after SARS-CoV-2 infection. Neurol Neuroimmunol Neuroinflamm. 2020;7(5):e797.
- DOI: 10.1212/NXI.0000000000000797
- Parsons T, Banks S, Bae C, et al. COVID-19-associated Acute Disseminated Encephalomyelitis (ADEM). J Neurol. 2020;1-4.
- DOI: 10.1007/s00415-020-09951-9
- Reichard RR, Kashani KB, Boire NA, et al. Neuropathology of COVID-19: a spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology. Acta Neuropathol. 2020;140(1):1-6.
- DOI: 10.1007/s00401-020-02166-2
- Franceschi AM, Ahmed O, Giliberto L, Castillo M. Hemorrhagic posterior reversible encephalopathy syndrome as a manifestation of COVID-19 infection. AJNR Am J Neuroradiol. 2020.
- DOI: 10.3174/ajnr.A6595
- Byrnes S, Bisen M, Syed B, et al. COVID-19 Encephalopathy masquerading as substance withdrawal. J Med Virol. 2020;.
- DOI: 10.1002/jmv.26065
- Pastor J, Vega-Zelaya L, Abad EM. Specific EEG encephalopathy pattern in SARS-CoV-2 patients. J Clin Med. 2020;9(5):E1545.
- DOI: 10.3390/jcm9051545
- Poyiadji N, Shahin G, Noujaim D, et al. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020;20118.
- DOI: 10.1148/radiol.2020201187
- Цинзерлинг В.А., Чухловина М.Л. Инфекционные поражения нервной системы: вопросы этиологии, патогенеза и диагностики. Руководство для врачей. - СПб.: ЭЛБИ-СПб, 2011. - 584 с.
- Шмидт Т.Е. Редкие демиелинизирующие заболевания центральной нервной системы // Неврологический журнал. - 2016. - Т.21. - №5. - С. 252-264.
- DOI: 10.18821/1560-9545-2016-21-5-252-264
- Radmanesh F, Rodriguez-Pla A, Pincus MD, Burns JD. Severe cerebral involvement in adult-onset hemophagocytic lymphohistiocytosis. J Clin Neurosci. 2020;76:236-237.
- DOI: 10.1016/j.jocn.2020.04.054
- Finelli PF, Uphoff DF. Magnetic resonance imaging abnormalities with septic encephalopathy. J Neurol Neurosurg Psychiatry. 2004;75(8):1189-1191.
- DOI: 10.1136/jnnp.2003.030833
- Karakike E, Giamarellos-Bourboulis EJ. Macrophage activation-like syndrome: a distinct entity leading to early death in sepsis. Front Immunol. 2019;10:55.
- DOI: 10.3389/fimmu.2019.00055
- Misra DP, Agarwal V, Gasparyan AY, Zimba O. Rheumatologists' perspective on coronavi rus disease 19 (COVID-19) and potential therapeutic targets. Clin Rheumatol. 2020;39(7):2055-2062.
- DOI: 10.1007/s10067-020-05073-9
- Valade S, Azoulay E, Galicier L, et al. Coagulation disorders and bleedings in critically ill patients with hemophagocytic lymphohistiocytosis. Mediсine. 2015;94(40):e1692.
- DOI: 10.1097/MD.0000000000001692
- Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138(5):575-578. 10.1001/JAMA Ophthalmol.2020.1291.
- DOI: 10.1001/jamaophthalmol.2020.1291
- Loon SC, Teoh SC, Oon LL, et al. The severe acute respiratory syndrome Coronavirus in tears. Br J Ophthalmol. 2004;88(7):861-863.
- DOI: 10.1136/bjo.2003.035931
- Salducci M, La Torre G. COVID-19 emergency in the cruise's ship: a case report of conjunctivitis. Clin Ter. 2020;171(3):e189-e191.
- DOI: 10.7417/CT.2020.2212
- Баклаушев В.П., Кулемзин С.В., Горчаков А.А., и др. COVID-19. Этиология, патогенез, диагностика и лечение // Клиническая практика. - 2020. - Т.11. - №1. - С. 7-20.
- DOI: 10.17816/clinpract26339
- Li JО, Lam DS, Chen Y, Ting DS. Novel Coronavirus disease 2019 (COVID-19): the importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104(3):297-298.
- DOI: 10.1136/bjophthalmol-2020-315994
- Chen Lu, Liu M, Zhang Z, et al. Ocular manifestations of a hospitalised patient with confirmed 2019 novel coronavirus disease. Br J Ophthalmol. 2020;104(6):748-755.
- DOI: 10.1136/bjophthalmol-2020-316304
- Vassilara F, Spyridaki A, Pothitos G, et al. A rare case of human coronavirus 229E associated with acute respiratory distress syndrome in a healthy adult. Case Rep Infect Dis. 2018;2018:6796839.
- DOI: 10.1155/2018/6796839
- Zhou Y, Zeng Y, Tong Y, et al. Ophthalmologic evidence against the interpersonal trans-mission of 2019 novel coronavirus through conjunctiva. New York: medRxiv. 2020.
- DOI: 10.1101/2020.02.11.20021956
- Scalinci SZ, Trovato Battagliola E. Conjunctivitis can be the only presenting sign and symptom of COVID-19. IDCases. 2020;20:e00774.
- DOI: 10.1016/j.idcr.2020.e00774
- Cheema M, Aghazadeh H, Nazarali S, et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID-19). Can J Ophthalmol. 2020;S0008-4182(20)30305-7.
- DOI: 10.1016/j.jcjo.2020.03.003
- Sadhu S, Agrawal R, Pyare R, et al. COVID-19: Limiting the risks for eye care professionals. Ocul Immunol Inflamm. 2020;1-7.
- DOI: 10.1080/0927394-8.2020.1755-442
- De Grootmijnes JD, van Dun JM, van der Most RG, de Groot RJ. Natural history of a recurrent feline coronavirus infection and the role of cellular immunity in survival and disease. J Virol. 2005;79(2):1036-1044.
- DOI: 10.1128/JVI.79.2.1036-1044.2005
- Neri P, Pichi F. COVID-19 and the eye immunity: lesson learned from the past and possible new therapeutic insights. Int Ophthalmol. 2020;40(5):1057-1060.
- DOI: 10.1007/s10792-020-01389-2
- Nakagaki K, Nakagaki K, Taguchi F. Receptor-independent spread of a highly neurotropic murine coronavirus JHMV strain from initially infected microglial cells in mixed neural cultures. J Virol. 2005;79(10):6102-6110.
- DOI: 10.1128/JVI.79.10.6102-6110.2005
- Shindler KS, Kenyon LC, Dutt M, et al. Experimental optic neuritis induced by a demyelinating strain of mouse hepatitis virus. J Virol. 2008;82(17):8882-8886.
- DOI: 10.1128/JVI.00920-08
- Bailey OT, Pappenheimer AM, Cheever FS, Daniels JB. A murine virus (JHM) causing disseminated encephalomyelitis with extensive destruction of myelin: II. Pathology. J Exp Med. 1949;90(3):195-212.
- DOI: 10.1084/jem.90.3.195
- Seah I, Agrawal R. Can the Coronavirus Disease 2019 (COVID-19) affect the eyes? A review of Coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020;28(3):391-395.
- DOI: 10.1080/09273948.2020.1738501
- Butowt R, Bilinska K. SARS-CoV-2: olfaction, brain infection, and the urgent need for clinical samples allowing earlier virus detection. ACS Chem Neurosci. 2020;11(9):1200-1203.
- DOI: 10.1021/acschemneuro.0c00172
- Qing H, Li Z, Yang Z, et al. The possibility of COVID-19 transmission from eye to nose. Acta Ophthalmol. 2020;98(3):e388.
- DOI: 10.1111/aos.14412
- Giacomelli A, Pezzati L, Conti F, et al. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: A cross-sectional study. Clin Infect Dis. 2020;ciaa330.
- DOI: 10.1093/cid/ciaa330
- Ralli M, Di Stadio A, Greco A, et al. Defining the burden of olfactory dysfunction in COVID-19 patients. Eur Rev Med Pharmacol Sci. 2020;24(7):3440-3441.
- DOI: 10.26355/eurrev_202004_20797
- Lechien JR, Chiesa-Estomba CM, Place S, et al.; COVID-19 Task Force of YO-IFOS. Clinical and epidemiological characteristics of 1,420 European patients with mild-to-moderate Coronavirus Disease 2019. J Intern Med. 2020;.
- DOI: 10.1111/joim.13089
- Xydakis MS, Dehgani-Mobaraki P, Holbrook EH, et al. Smell and taste dysfunction in patients with COVID-19. Lancet Infect Dis. 2020;S1473-3099(20)30293-0.
- DOI: 10.1016/S1473-3099(20)30293-0
- Gane SB, Kelly C, Hopkins C. Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome? Rhinology. 2020;58(3):299-301.
- DOI: 10.4193/Rhin20.114
- Hopkins C, Surda P, Kumar N. Presentation of new onset anosmia during the COVID-19 pandemic. Rhinology. 2020;58(3):295-298.
- DOI: 10.4193/Rhin20.116
- Moein ST, Hashemian SM, Mansourafshar B, et al. Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol. 2020;.
- DOI: 10.1002/alr.22587
- Yan CH, Faraji F, Prajapati DP, et al. Association of chemosen-sory dysfunction and Covid-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol. 2020;.
- DOI: 10.1002/alr.22579
- Gautier J-F, Ravussin Y. A new symptom of COVID-19: loss of taste and smell. Obesity (Silver Spring). 2020;28(5):848.
- DOI: 10.1002/oby.22809
- Izquierdo-Dominguez A, Rojas-Lechuga MJ, Mullol J, Alobid I. Olfactory dysfunction in the COVID-19 outbreak. J Investig Allergol Clin Immunol. 2020.
- DOI: 10.18176/jiaci.0567
- Temmel AF, Quint C, Schickinger-Fischer B, et al. Characteristics of olfactory dis-orders in relation to major causes of olfactory loss. Arch Otolaryngol Head Neck Surg. 2002;128(6):635-641.
- DOI: 10.1001/archotol.128.6.635
- Soler ZM, Patel ZM, Turner JH, Holbrook EH. A primer on viral-associated olfactory loss in the era of COVID-19. Int Forum Allergy Rhinol. 2020;.
- DOI: 10.1002/alr.22578
- Lovato A, de Filippis C. Clinical presentation of COVID-19: a systematic review focusing on upper airway symptoms. Ear Nose Throat J. 2020;145561320920762.
- DOI: 10.1177/0145561320920762
- Heidari F, Karimi E, Firouzifar M, et al. Anosmia as a prominent symptom of COVID-19 infection. Rhinology. 2020;58(3):302-303.
- DOI: 10.4193/Rhin20.140
- Obiefuna S, Donohoe C. Neuroanatomy, Nucleus Gustatory. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020.
- Goh Y, Beh DL, Makmur A, et al. Pearls and oysters: facial nerve palsy as a neurological manifestation of Covid-19 infection. Neurology. 2020;.
- DOI: 10.1212/WNL.0000000000009863
- Andorinho de Freitas Ferreira AC, Romão ТТ, Macedo YS, et al. COVID-19 and herpes zoster coinfection presenting with trigeminal neuropathy. Eur J Neurol. 2020:.
- DOI: 10.1111/ene.14361
- Vaira LA, Salzano G, Deiana G, De Riu G. Anosmia and ageusia: common findings in COVID-19 patients. Laryngoscope. 2020;130(7):1787.
- DOI: 10.1002/lary.28692
- Vaira LA, Deiana G, Fois AG, et al. Objective evaluation of anosmia and ageusia in COVID-19 patients: Single-center experience on 72 cases. Head Neck. 2020;42(6):1252-1258.
- DOI: 10.1002/hed.26204
- Finsterer J, Stollberger C. Causes of Hypogeusia/Hyposmia in SARS-CoV2 infected patients. J Med Virol. 2020;.
- DOI: 10.1002/jmv.25903
- Wee LE, Chan YF, Teo NW, et al. The role of self-reported olfactory and gustatory dysfunction as a screening criterion for suspected COVID-19. Eur Arch Otorhinolaryngol. 2020;1-2.
- DOI: 10.1007/s00405-020-05999-5
- Ng SC, Tilg H. COVID-19 and the gastrointestinal tract: more than meets the eye. Gut. 2020;69(6):973-974.
- DOI: 10.1136/gutjnl-2020-321195
- Agarwal A, Chen A, Ravindran N, et al. Gastrointestinal and liver manifestations of COVID-19. J Clin Exp Hepatol. 2020;10(3):263-265. 10.1016/j.jceh. 2020.03.001.
- DOI: 10.1016/j.jceh.2020.03.001
- Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970-971.
- DOI: 10.1056/NEJMc2001468
- Collins AM, Neurogenic Cough. Neurologic and Neurodegenerative Diseases of the Larynx. 2020. Р. 253-261.
- Татарников В.С. Роль ростральных вентролатеральных отделов продолговатого мозга в регуляции активности дыхательного центра: Автореф. дис. … канд. мед. наук. - Самара, 1996. - 22 с. Доступно по: https://search.rsl.ru/ru/record/01000098524. Ссылка активна на 14.02.2020.
- Lee I-C, Huo T-I, Huang Yi-H. Gastrointestinal and liver manifestations in patients with COVID-19. J Chin Med Assoc. 2020;.
- DOI: 10.1097/jcma.0000000000000319
- Shastin D, Nidamanuri P, Nannapaneni R. Recurrent hiccups may signal brainstem pathology and should be investigated. BMJ Case Rep. 2018;2018. pii: bcr-2017-222926.
- DOI: 10.1136/bcr-2017-222926
- Xu J, Zhong S, Liu J, et al. Detection of severe acute respiratory syndrome coronavirus in the brain: potential role of the chemokine mig in pathogenesis. Clin Infect Dis. 2005;41(8):1089-1096.
- DOI: 10.1086/444461
- Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neursci. 2020;11(7):995-998.
- DOI: 10.1021/acschemneuro.0c00122
- Li Y-C, Bai W-Z, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020;92(6):552-555.
- DOI: 10.1002/jmv.25728
- Tassorelli C, Mojoli F, Baldanti F, et al. COVID-19: What if the brain had a role in causing the deaths? Eur J Neurol. 2020;.
- DOI: 10.1111/ene.14275
- McCray PB, L, C, et al. Lethal infection of K18-hACE2 Mice infected with severe acute respiratory syndrome Coronavirus.. 2007;81(2):813-821. doi:.
- Natoli S, Oliveira V, Calabresi P, et al. Does SARS-Cov-2 invade the brain? Translational lessons from animal models. Eur J Neurol. 2020;.
- DOI: 10.1111/ene.14277
- Camdessanche JP, Morel J, Pozzetto B, et al. COVID-19 may induce Guillain-Barré syndrome. Rev Neurol (Paris). 2020;176(6):516-518.
- DOI: 10.1016/j.neurol.2020.04.003
- Riva N, Russo T, Falzone YM, et al. Post-infectious Guillain-Barré syndrome related to SARS-CoV-2 infection: a case report. J Neurol. 2020;1-3.
- DOI: 10.1007/s00415-020-09907-z
- Alberti P, Beretta S, Piatti M, et al. Guillain-Barré Syndrome Related to COVID-19 Infection. Neurol Neuroimmunol Neuroinflamm. 2020;7(4):e741.
- DOI: 10.1212/XI.0000000000000741
- Toscano G, Palmerini F, Ravaglia S, et al. Guillain-Barré syndrome associated with SARS-CoV-2. N Engl J Med. 2020;382(26):2574-2576.
- DOI: 10.1056/NEJMc2009191
- Padroni M, Mastrangelo V, Asioli GM, et al. Guillain-Barré syndrome following COVID-19: new infection, old complication? J Neurol. 2020;1-3.
- DOI: 10.1007/s00415-020-09849-6
- Finsterer J, Scorza FA, Ghosh R. COVID-19 Polyradiculitis in 24 Patients Without SARS-CoV-2 in the Cerebro-Spinal Fluid. J Med Virol. 2020;.
- DOI: 10.1002/jmv.26121
- Coen M, Jeanson G, Almeida LA, et al. Guillain-Barré Syndrome as a complication of SARS-CoV-2 infection. Brain Behav Immun. 2020;87:111-112.
- DOI: 10.1016/j.bbi.2020.04.074
- Lascano AM, Epiney J-B, Coen M, et al. SARS-CoV-2 and Guillain-Barré Syndrome: AIDP variant with favorable outcome. Eur J Neurol. 2020;.
- DOI: 10.1111/ene.14368
- Bigaut K, Mallaret M, Baloglu S, et al. Guillain-Barré syndrome related to SARS-CoV-2 infection. Neurol Neuroimmunol Neuroinflamm. 2020;7(5):e785.
- DOI: 10.1212/NXI.0000000000000785
- Assini A, Benedetti L, Di Maio S, et al. New clinical manifestation of COVID-19 related Guillain-Barrè Syndrome highly responsive to intravenous immunoglobulins: two Italian cases. Neurol Sci. 2020.
- DOI: 10.1007/s10072-020-04484-5
- Oguz-Akarsu E, Ozpar R, Mirzayev H, et al. Guillain-Barré syndrome in a patient with minimal symptoms of COVID-19 infection. Muscle Nerve. 2020;.
- DOI: 10.1002/mus.26992
- Sedaghat Z, Karimi N. Guillain-Barre syndrome associated with COVID-19 infection: a case report. J Clin Neurosci. 2020;76:233-235.
- DOI: 10.1016/j.jocn.2020.04.062
- El Otmani H, El Moutawakil B, Rafai MA, et al. Covid-19 and Guillain-Barré syndrome: more than a coincidence! Rev Neurol (Paris). 2020;176(6):518-519.
- DOI: 10.1016/j.neurol.2020.04.007
- Su XW, Palka SV, Rao RR, et al. SARS-CoV-2-associated Guillain-Barré syndrome with dysautonomia. Muscle Nerve. 2020;.
- DOI: 10.1002/mus.26988
- Turgay C, Emine T, Ozlem K, et al. A rare cause of acute flaccid paralysis: human coronaviruses. J Pediatr Neurosci. 2015;10(3):280-281.
- DOI: 10.4103/1817-1745.165716
- Kim JE, Heo JH, Kim HO, et al. Neurological complications during treatment of Middle East respiratory syndrome. J Clin Neurol. 2017;13(3):227-233.
- DOI: 10.3988/jcn.2017.13.3.227
- Gigli GL, Bax F, Marini A, et al. Guillain-Barré syndrome in the COVID-19 era: just an occasional cluster? J Neurol. 2020;1-3.
- DOI: 10.1007/s00415-020-09911-3
- Gupta A, Paliwal VK, Garg RK. Is COVID-19-related Guillain-Barré syndrome different? Brain Behav Immun. 2020;87:177-178.
- DOI: 10.1016/j.bbi.2020.05.051
- Sancho-Saldaña A, Lambea-Gil Á, Capablo Liesa JL, et al. Guillain-Barré syndrome associated with leptomeningeal enhancement following SARS-CoV-2 infection. Clin Med (Lond). 2020;clinmed.2020-0213.
- DOI: 10.7861/clinmed.2020-0213
- Chan JL, Ebadi H, Sarna JR. Guillain-Barré syndrome with facial diplegia related to SARS-CoV-2 infection. Can J Neurol Sci. 2020;1-10.
- DOI: 10.1017/cjn.2020.106
- Caamaño DS, Beato AR. Facial diplegia, a possible atypical variant of Guillain-Barré Syndrome as a rare neurological complication of SARS-CoV-2. J Clin Neurosci. 2020;77:230-232.
- DOI: 10.1016/j.jocn.2020.05.016
- Helbok R, Beer R, Löscher W, et al. Guillain-Barré syndrome in a patient with antibodies against SARS-COV-2. Eur J Neurol. 2020.
- DOI: 10.1111/ene.14388
- Scoppetta C, Di Gennaro G, Polverino F. Editorial - High dose intravenous immunoglobulins as a therapeutic option for COVID-19 patients. Eur Rev Med Pharmacol Sci. 2020;24(9):5178-5179.
- DOI: 10.26355/eurrev_202005_21214
- Gutiérrez-Ortiz C, Méndez A, Rodrigo-Rey S, et al. Miller fisher syndrome and polyneuritis Cranialis in COVID-19. Neurology. 2020;.
- DOI: 10.1212/WNL.0000000000009619
- Lantos JE, Strauss SB, Lin E. COVID-19-associated miller fisher syndrome: MRI findings. AJNR Am J Neuroradiol. 2020. 10.3174 /ajnr.A6609.
- DOI: 10.3174/ajnr.A6609
- Dinkin M, Gao V, Kahan J, et al. COVID-19 presenting with ophthalmoparesis from cranial nerve palsy. Neurology. 2020;.
- DOI: 10.1212/WNL.0000000000009700
- Wei H, Yin H, Huang M, Guo Z. The 2019 novel cornoavirus pneumonia with onset of oculomotor nerve palsy: a case study. J Neurol. 2020;267(5):1550-1553.
- DOI: 10.1007/s00415-020-09773-9
- Pérez Álvarez ÁI, Suárez Cuervo C, Fernández Menéndez S. [Infección por SARS-CoV-2 asociada a diplopía y anticuerpos antirreceptor de acetilcolina. (In English, Spanish)]. Neurología. 2020,35(4):264-265.
- DOI: 10.1016/j.nrl.2020.04.003
- Anand P, Slama MC, Kaku M, et al. COVID-19 in patients with myasthenia gravis. Muscle Nerve. 2020;.
- DOI: 10.1002/mus.26918
- Guidon AC, Amato AA. COVID-19 and neuromuscular disorders. Neurology. 2020;94(22):959-969.
- DOI: 10.1212/WNL.0000000000009566
- Jacob S, Muppidi S, Guidon A, et al; International MG/COVID-19 Working Group. Guidance for the management of myasthenia gravis (MG) and Lambert-Eaton myasthenic syndrome (LEMS) during the COVID-19 pandemic. J Neurol Sci. 2020;412:116803.
- DOI: 10.1016/j.jns.2020.116803
- Delly F, Syed MJ, Lisak RP, Zutshi D. Myasthenic crisis in COVID-19. J Neurol Sci. 2020;414:116888.
- DOI: 10.1016/j.jns.2020.116888
- Ramaswamy SB, Govindarajan R. COVID-19 in Refractory Myasthenia Gravis - A Case Report of Successful Outcome. J Neuromuscul Dis. 2020;7(3):361-364. 10.3233/JND - 200520.
- DOI: 10.3233/JND-200520
- Wong PF, Craik S, Newman P, et al. Lessons of the month 1: a case of rhombencephalitis as a rare complication of acute COVID-19 infection. Clin Med (Lond). 2020. pii: clinmed.2020-0182.
- DOI: 10.7861/clinmed.2020-0182
- Cuneo GL, Grazzini I, Guadagni M, et al. An atypical Bickerstaff's brainstem encephalitis with involvement of spinal cord. Neuroradiol J. 2016;29(5):396-399. 10.1177/197140091666 5383.
- DOI: 10.1177/1971400916665383
- Муртазина А.Ф., Наумова Е.С., Никитин С.С., и др. Стволовой энцефалит Бикерстаффа, острый поперечный миелит и острая моторная аксональная нейропатия: сложности диагностики и лечения пациентов с перекрестными синдромами. Клиническое наблюдение // Нервно-мышечные болезни. - 2017. - Т.7. - №3. - С. 56-62. [Murtazina AF, Naumova ES, Nikitin SS, et al. Bickerstaff brainstem encephalitis, acute transverse myelitis, and acute motor axonal neuropathy: diagnostic and treatment challenges in patients with concomitant syndromes. Clinical observation. Neuromuscular Diseases. 2017;7(3):56-62. (In Russ).]
- DOI: 10.17650/2222-8721-2017-7-3-56-62
- Sotoca J, Rodríguez-Álvarez Y. COVID-19-associated acute necrotizing myelitis. Neurol Neuroimmunol Neuroinflamm. 2020;7(5):e803.
- DOI: 10.1212/NXI.0000000000000803
- Гусев Е.И., Мартынов М.Ю., Бойко А.Н., и др. Новая коронавирусная инфекция (COVID-19) и поражение нервной системы: механизмы неврологических расстройств, клинические проявления, организация неврологической помощи // Журнал неврологии и психиатрии им. С.С. Корсакова. - 2020. - Т.120. - №6. - С. 7-16. [Gusev EI, Martynov MYu, Boyko AN, et al. Novaya koronavirusnaya infektsiya (COVID-19) i porazheniye nervnoy sistemy: mekhanizmy nevrologicheskikh rasstroystv, klinicheskiye proyavleniya, organizatsiya nevrologicheskoy pomoshchi. S.S. Korsakov Journal of Neurology and Psychiatry. 2020;120(6):7-16. (In Russ).] 10.17116/ jnevro20201200617. 10.17116/jnevro20201200617
- DOI: 10.17116/jnevro20201200617.https
- Анестезиолого-реанимационное обеспечение пациентов с новой коронавирусной инфекцией COVID-19. Федерация анестезиологов и реаниматологов. Методические рекомендации. - М., 2020. - 183 с.
- Lai C-C, Liu YH, Wang C-Yi, et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): facts and myths. J Microbiol Immunol Infect. 2020;53(3):404-412.
- DOI: 10.1016/j.jmii.2020.02.012
- Varga Z, Flammer AJ, Steiger P, et al. Endotehelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-1418. 10.1016/S0140-6736 (20)30937-5.
- DOI: 10.1016/S0140-6736(20)30937-5
- Morassi M, Bagatto D, Cobelli M, et al. Stroke in patients with SARS-CoV-2 infection: case series. J Neurol. 2020;1-8.
- DOI: 10.1007/s00415-020-09885-2
- Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020.
- DOI: 10.1001/jama-cardio.2020.1096
- Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020:e201017.
- DOI: 10.1001/jamacardio.2020.1017
- Qureshi AI, Abd-Allah F, Alsenani F, et al. Management of acute ischemic stroke in patients with COVID-19 infection: Report of an international panel. Int J Stroke. 2020;1747493020923234.
- DOI: 10.1177/1747493020923234
- Pranata R, Huang I, Lukito AA, Raharjo SB. Elevated N-terminal Pro-Brain natriuretic peptide is associated with increased mortality in patients with COVID-19: systematic review and meta-analysis. Postgrad Med J. 2020;96(1137):387-391.
- DOI: 10.1136/postgradmedj-2020-137884
- Tu WJ, Cao J, Yu L, et al. Clinicolaboratory study of 25 fatal cases of COVID-19 in Wuhan. Intensive Care Med. 2020;46(6):1117-1120.
- DOI: 10.1007/s00134-020-06023-4
- Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020.
- DOI: 10.1001/jamacardio.2020.1286
- Akhmerov A, Marban E. COVID-19 and the heart. Circ Res. 2020;126(10):1443-1455. 10.1161/CIRCRES AHA.120.317055.
- DOI: 10.1161/CIRCRESAHA.120.317055
- Aggarwal G, Lippi G, Henry BM. Cerebrovascular disease is associated with an increased disease severity in patients with Coronavirus Disease 2019 (COVID-19): a pooled analysis of published literature. Int J Stroke. 2020;15(4):385-389.
- DOI: 10.1177/1747493020921664
- Hess DC, Eldahshan W, Rutkowski E. COVID-19-related stroke. Transl Stroke Res. 2020;11(3):322-325.
- DOI: 10.1007/s12975-020-00818-9
- Young K. COVID-19: Stroke in Young Adults/New Presentation in Kids/ACS Advissions. N Engl J Med. 2020.
- DOI: 10.1056/NEYMc2009787
- Jin H., Hong C., Chen S., Zhou Y, Wang Y. et al. Consensus for Prevention and Management of Coronavirus Disease 2019 (COVID-19) for Neurologists. Stroke Vasc. Neurol., 2020; svn-2020-0003-82.
- DOI: 10.1136/svn-2020-000382
- Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14.
- DOI: 10.1016/j.thromres.2020.04.024
- Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382(17):e38.
- DOI: 10.1056/NEJMc2007575
- Bernstein L, Stead Sellers F. Patients with heart attacks, strokes and even appendicitis vanish from hospitals. 2020. Available from: https://www.washingtonpost.com/health/patients-with-heart-attacks-strokes-and-even-appendicitis-vanish-from-hospitals/2020/04/19/9ca3ef24-7eb4-11ea-9040-68981f488eed_story.html.
- Cavalcanti DD, Raz E, Shapiro M, et al. Cerebral venous thrombosis associated with COVID-19. AJNR Am J Neuroradiol. 2020.
- DOI: 10.3174/ajnr.A6644
- Hughes C, Nichols T, Pike А, et al. Cerebral venous sinus thrombosis as a presentation of COVID-19. Eur J Case Rep Intern Med. 2020;7(5):001691.
- DOI: 10.12890/2020_001691
- Poillon G, Obadia M, Perrin M, et al. Cerebral venous thrombosis associated with COVID-19 infection: causality or coincidence? J Neuroradiol. 2020;S0150-9861(20)30167-X.
- DOI: 10.1016/j.neu-rad.2020.05.003
- Avula A, Nalleballe K, Narula N, et al. COVID-19 presenting as stroke. Brain Behav Immun. 2020;87:115-119.
- DOI: 10.1016/j.bbi.2020.04.077
- Violi F, Pastori D, Cangemi R, et al. Hypercoagulation and antithrom-botic treatment in Coronavirus 2019: a new challenge. Thromb Haemost. 2020;120(6):949-956.
- DOI: 10.1055/s-0040-1710317
- Zhao J, Rudd A, Liu R. Challenges and potential solutions of stroke care during the Coronavirus disease 2019 (COVID-19) outbreak. Stroke. 2020;51(5):1356-1357.
- DOI: 10.1161/STROKEAHA.120.029701
- Oxley TJ, Mocco J, Majidi S, et al. Large-Vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382(20):e60.
- DOI: 10.1056/NEJMc2009787
- Siniscalchi A, Gallelli L. Could COVID-19 represent a negative prognostic factor in patients with stroke? Infect Control Hosp Epidemiol. 2020;1.
- DOI: 10.1017/ice.2020.146
- Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382(23):2268-2270.
- DOI: 10.1056/NEJMc2008597
- Dafer RM, Osteraas ND, Biller J. Acute stroke care in the Coronavirus disease 2019 pandemic. J Stroke Cerebrovasc Dis. 2020;29(7):10488. doi: 16/j.jstrokecerebrovasdis.2020.104881.
- Leira EC, Russman AN, Biller J, et al. Preserving stroke care during the COVID-19 pandemic: potential issues and solutions. Neurology. 2020;10.1212/WNL.00000-00000009713.
- DOI: 10.1212/WNL.0000000000009713
- Tsivgoulis G, Palaiodimou L, Katsanos AH, et al. Neurological manifestations and implications of COVID-19 pandemic. Ther Adv Neurol Disord. 2020;13:1756286420932036.
- DOI: 10.1177/1756286420932036
- Smith MS, Bonomo J, Knight 4th WA, et al. Endovascular therapy for patients with acute ischemic stroke during the COVID-19 Pandemic: a proposed algorithm. Stroke. 2020;51(6):1902-1909.
- DOI: 10.1161/STROKEAHA.120.029863
- Fraser JF, Arthur AS, Chen M, et al. Society of neurointerventional surgery recommendations for the care of emergent neurointerventional patients in the setting of Covid-19. J Neurointerv Surg. 2020;12(6):539-541.
- DOI: 10.1136/neu-rintsurg-2020-016098
- Sharifi-Razavi A, Karimi N, Rouhani N. COVID-19 and intracerebral haemorrhage: causative or coincidental? New Microbes New Infect. 2020;35:100669.
- DOI: 10.1016/j.nmni.2020.100669
- Saiegh FA, Ghosh R, Leibold A, et al. Status of SARS-CoV-2 in cerebrospinal fluid of patients with COVID-19 and stroke. J Neurol Neurosurg Psychiatry. 2020;jnnp-2020-323522.
- DOI: 10.1136/jnnp-2020-323522
- Chougar L., Mathon B., Weiss N., Degos V., Shor N. Atypical Deep Cerebral Vein Thrombosis with Hemorrhagic Venous Infarction in a Patient Positive for COVID-19. AJNR Am J Neuroradiol. 2020.
- DOI: 10.3174/ajnr.A6642
- Herman C., Mayer K., Sarwal A. Scoping review of prevalence of neurologic comorbidities in patients hospitalized for COVID-19. Neurology., 2020; 95:1-8. 10.1212/WNL.0000000000 009673.
- DOI: 10.1212/WNL.0000000000009673
- Tay HS, Harwood R. Atypical presentation of COVID-19 in a frail older person. Age Ageing. 2020;afaa068.
- DOI: 10.1093/ageing/afaa068
- Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;e200950.
- DOI: 10.1001/jamacardio.2020.0950
- Potere N, Valeriani E, Candeloro M, Tana M, Porreca E. et al. Acute complications and mortality in hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Crit Care. 2020;24(1):389.
- DOI: 10.1186/s13054-020-03022-1
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-448.
- DOI: 10.1016/S2213-2600(20)30079-5
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062.
- DOI: 10.1016/S0140-6736(20)30566-3
- La Hue SC, James TC, Newman JC, et al. W. Collaborative Delirium Prevention in the Age of COVID-19. J Am Geriatr Soc. 2020;68(5):947-949.
- DOI: 10.1111/jgs.16480
- Sanders BJ, Bakar M, Mehta S, et al. Hyperactive delirium requires more aggressive management in patients with COVID-19: temporarily rethinking "Low and Slow". J Pain Symptom Manage. 2020: S0885-3924(20)30389-4.
- DOI: 10.1016/j.jpainsymman.2020.05.013
- Salluh JI, Wang H, Schneider EB. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350:h2538.
- DOI: 10.1136/bmj.h2538
- O'Hanlon S, Inouye SK. Delirium: a missing piece in the COVID-19 pandemic puzzle. Age Ageing. 2020:afaa094.
- DOI: 10.1093/ageing/afaa094
- Alkeridy WA, Almaghlouth I, Alrashed R, et al. A unique presentation of delirium in a patient with otherwise asymptomatic COVID-19. J Am Geriatr Soc. 2020;.
- DOI: 10.1111/jgs.16536
- Kotfis K, Roberson SW, Wilson JE, et al. COVID-19: ICU delirium management during SARS-CoV-2.pandemic.Crit Care. 2020;24(1):176.
- DOI: 10.1186/s13054-020-02882-x
- Седация пациентов в отделениях анестезиологии, реанимации и интенсивной терапии. Федерация анестезиологов и реаниматологов. Методические рекомендации. - М., 2020. - 39 с.
- Kotfis K, Williams RS, Wilson J, et al. COVID-19: What do we need to know about ICU delirium during the SARS-CoV-2 pandemic? Anaesthesiol Intensive Ther. 2020;40590.
- DOI: 10.5114/ait.2020.95164
- Shneider A, Kudriavtsev A, Vakhrusheva A. Can Melatonin reduce the severity of COVID-19 pandemic? Int Rev Immunol. 2020;1-10.
- DOI: 10.1080/08830185.2020.1756284
- Zambrelli E, Canevini M, Gambini O, D'Agostino A. Delirium and sleep disturbances in COVID-19: a possible role for melatonin in hospitalized patients? Sleep Med. 2020;70:111.
- DOI: 10.1016/j.sleep.2020.04.006
- Rábano-Suárez P, Bermejo-Guerrero L, Méndez-Guerrero A, et al. Genera-lized myoclonus in COVID-19. Neurology. 2020;. 10.1212/WNL.00000 00000009829.
- DOI: 10.1212/WNL.0000000000009829
- Balloy G., Mahé P.J., Leclair-Visonneau L., Péréon Y. et al. Non-lesional status epilepticus in a patient with coronavirus disease 2019. Neurophysiol., 2020. 10.1016/j.clinph.2020. 05.005.
- DOI: 10.1016/j.clinph.2020.05.005
- Garg RK, Paliwal VK, Gupta A. Encephalopathy in patients with COVID-19: a review. J Med Virol. 2020.
- DOI: 10.1002/jmv.26207
- Asadi-Pooya A.A. Seizures Associated With Coronavirus Infections. Seizure., 2020;79:49-52.
- DOI: 10.1016/j.seizure.2020.05.005
- French JA, Brodie MJ, Caraballo R. Keeping people with epilepsy safe during the Covid-19 pandemic. Neurology. 2020;94(23):1032-1037.
- DOI: 10.1212/WNL0000000000009632
- Zayet S, Abdallah YB, Royer P-Y, et al. Encephalopathy in patients with COVID-19: ‘Causality or Coincidence?' J Med Virol. 2020;.
- DOI: 10.1002/jmv.26027
- Filatov A, Sharma P, Hindi F, Espinosa PS. Neurological complications of Coronavirus disease (COVID-19) Encephalopathy. Cureus. 2020;12(3):e7352.
- DOI: 10.7759/cureus.7352
- Haddad S, Tayyar R, Risch L, et al. Encephalopathy and Seizure Activity in a COVID-19 well controlled HIV patient. IDCases. 2020;21:e00814.
- DOI: 10.1016/j.idcr.2020.e00814
- Pinto AA, Carroll LS, Nar V, et al. CNS inflammatory vasculopathy with Antimyelin Oligodendrocyte Glycoprotein Antibodies in COVID-19. Neurol Neuroimmunol Neuroinflamm. 2020;7(5):e813.
- DOI: 10.1212/NXI.0000000000000813
- Brun G, Hak J-F, Coze S, et al. COVID-19-White matter and globus pallidum lesions: demyelination or small-vessel vasculitis? Neurol Neuroimmunol Neuroinflamm. 2020;7(4):e777.
- DOI: 10.1212/NXI.0000000000000777


