Постковидная астения, саркопения и генерализованная мышечная слабость у гериатрических больных
Автор: Белопасов В.В., Веселова Д.К.
Журнал: Клиническая практика @clinpractice
Рубрика: Обзоры
Статья в выпуске: 2 т.15, 2024 года.
Бесплатный доступ
Астения, саркопения, ограничение двигательной активности значительно распространены среди гериатрических пациентов в постковидном периоде. Внедрение SARS-CoV-2 в организм человека запускает системные воспалительные реакции, оказывая прямое и опосредованное патологическое воздействие на скелетные мышцы. Проявлениями постковидного синдрома могут быть дисфункциональные нарушения органов и систем, включающие астению, мышечную слабость, одышку, боль в груди, когнитивные нарушения, депрессию, тревогу и нарушения сна. Сопутствующие гипоксемия, коморбидность и длительная гиподинамия способствуют изменениям структуры и функциональности мышечных волокон. Одним из новейших диагностических трендов является акцент на оценку индекса ALMI, свидетельствующего о том, что снижение мышечной массы верхних и нижних конечностей является возможной причиной развития функциональных ограничений у пациентов, перенёсших COVID-19. Реабилитация пациентов, перенёсших COVID-19, предполагает ежедневное выполнение физических упражнений с отягощением с учётом переносимости нагрузок, а также обязательную медикаментозную, нутритивную и психологическую поддержку.
Астения, саркопения, постковидный период, индекс almi
Короткий адрес: https://sciup.org/143183232
IDR: 143183232 | DOI: 10.17816/clinpract629475
Текст обзорной статьи Постковидная астения, саркопения и генерализованная мышечная слабость у гериатрических больных
Белопасов В.В., Веселова Д.К. Постковидная астения, саркопения и генерализованная мышечная слабость у гериатрических больных. Клиническая прак тика. 2024;15(2):51–58. doi:
Неожиданно и громко пронеслась по миру пандемия COVID-19 и привела к далеко идущим последствиям во всех сферах жизни общества. Проявления и осложнения заболевания, по многочисленным наблюдениям, носят гетерогенный характер, однако наиболее тяжёлое течение болезни отмечается у пожилых людей ввиду комбинированного воздействия множества факторов, в частности истощения их физиологических, когнитивных, функциональных резервов, известных как старческая астения, или «старческая хрупкость» [1]. Зачастую сопутствующая «старческой хрупкости» саркопения — возрастассоциированное поражение скелетной мускулатуры с прогрессирующей потерей мышечной массы и силы — увеличивает восприимчивость пожилого человека к инфекционным агентам и повышает риск развития негатив- ных последствий. Действительно, более высокая летальность вследствие перенесённой COVID-19 наблюдается у пожилых пациентов с диагностированной саркопенией [2].
Актуальность публикации объясняется медико-социальной значимостью астении и мышечной слабости у лиц пожилого возраста. Кроме того, тематика постковидной астении и саркопении у гериатрических больных, невзирая на злободневность и значимость, остаётся недостаточно освещённой как в отечественной, так и зарубежной литературе. Целью научного обзора является расширение знаний о подходах к диагностике и лечению генерализованной мышечной слабости в целом и в составе постковидного синдрома, что способствует укреплению и развитию мультиди-циплинарного подхода к возможности управления процессами старения.
Лицензия CC BY-NC-ND 4 /
The article can be used under the CC BY-NC-ND 4 license
POST-COVID ASTHENIA, SARCOPENIA AND MUSCLEWEAKNESS AMONG GERIATRIC PATIENTS
-
V .V. Belopasov1, D.K. Veselova2
-
1 Astrakhan State Medical University, Astrakhan, Russian Federation
-
2 Clinic City, Astrakhan, Russian Federation
Sarcopenia, asthenia, and motor activity restriction are common among geriatric patients in the post-COVID period. The SARS-CoV-2 virus triggers a cytokine storm in the human body and induces a direct viral effect on skeletal muscles. Manifestations of post-acute sequelae of COVID-19 (PASC) can include organ and system dysfunction, asthenia, muscle weakness, dyspnea, chest pain, cognitive impairment, depression, anxiety, and sleep disorders. Hypoxemia, comorbidity, and prolonged inactivity contribute to changes in the structure and functionality of the muscular fibers. One of the recent studies is ALMI-index, which indicates that a decrease in muscle mass of the upper and lower extremities may cause functional limitations in patients with long-COVID conditions. Rehabilitation of patients with post-COVID syndrome involves daily exercise with weights, considering load tolerance; mandatory medication; and nutritional and psychological support. Keywords: sarcopenia; long-COVID; ALMI-index; asthenia.
Belopasov VV, Veselova DK. Post-covid asthenia, sarcopenia and muscle weakness among geriatric patients. Journal of Clinical Practice. 2024;15(2):51–58. doi:
Submitted 27.03.2024 Revised 19.05.2024 Published online 25.06.2024
ТЕЧЕНИЕ САРКОПЕНИИ В КОНТЕКСТЕ ПОСТКОВИДНОГО СИНДРОМА
У пациентов с саркопенией в большинстве случаев отмечаются высокие показатели по шкале NEWS-2 (National Early Warning Score) наряду с повышением C-реактивного белка в крови как свидетельство тяжёлого течения COVID-19. Группа исследователей во главе с J.W. Kim [3] выделяет перекрёстное взаимодействие между скелетной мускулатурой и иммунной системой как основополагающий связующий фактор между саркопе-нией и клиническим течением COVID-19. Скелетные мышцы способны высвобождать множество мио-кинов, участвующих в аутокринной и паракринной регуляции [4]. К таким миокинам относят, например, интерлейкины (interleukin, IL) 6 и 15, которые стимулируют не только пролиферацию и активацию нейтрофилов, NK-клеток и CD8+Т-лимфоцитов, но и воздействуют на метаболизм мышечной ткани [4, 5]. При инфицировании снижение продукции IL-15 может способствовать плохому иммунному ответу против SARS-CoV-2. Кроме того, дизрегуля-ция выработки миокинов провоцирует провоспали-тельные процессы в клетках и тканях [6, 7].
Не меньший научный интерес вызывает течение саркопении при постковидном синдроме (postacute sequelae of COVID-19, PASC), чья природа, безусловно, является полиэтиологичной [8, 9]. Проявлениями PASC могут быть дисфункциональные нарушения органов и систем, сохраняющиеся после перенесённой инфекции более 3 месяцев либо возникшие de novo после выздоровления [10, 11], включающие астению, мышечную слабость, одышку, боль в груди, когнитивные нарушения, депрессию, тревогу и нарушения сна [12]. При обследовании во время госпитализации удельный вес миалгий и утомляемости в зависимости от возраста и выраженности респираторного синдрома составляет от 14,4 до 100% [13].
У пациентов с проявлениями «старческой хрупкости» и саркопенией отмечалось более выраженное проявление симптомов постковидного синдрома. У многих наблюдалась трансформация субклинических форм мышечной слабости (дина-пении, миопении, пресаркопении) в клинически выраженную саркопению из-за интенсивных катаболических процессов, длительного постельного режима, потери веса, недостаточного поступления белка и применения стероидных гормонов в процессе лечения. Некоторые клинические наблюдения показали, что пациенты с перенесённым COVID-19 подвергаются высокому риску развития миозита и рабдомиолиза [10, 14].

По результатам исследований, проведённых в период с 2020 по 2023 год с целью сравнительной характеристики симптомов long-COVID (постковид-ный синдром) у пациентов с пре- и саркопенией со здоровой когортой, установления прогрессирования старческой астении на фоне постковидного синдрома, а также контроля клинических проявлений саркопении и «старческой хрупкости» в динамике [10, 14, 15], обнаружено следующее.
Пожилые пациенты с высокими (от 6 баллов и выше) показателями шкалы CFS (Clinical Frailty Scale), оценивающей степень тяжести старческой астении, чаще демонстрировали тяжёлое атипичное течение коронавирусной инфекции в сочетании с делирием, что закономерно сопровождалось большей продолжительностью госпитализации. Результаты измерения окружности плеча и голени, оценки опросника SARC-F (A Simple Questionnaire to Rapidly Diagnose Sarcopenia), используемого для скрининга саркопении у данной группы пациентов, подтверждали наличие пресаркопении и зачастую саркопении, обусловливающих ограничение функциональной активности, через месяц после выписки из стационара. Эти нарушения, как правило, сохранялись длительно и повышали риск повторной госпитализации [15–18]. Через 3 месяца у исследуемой когорты с постковид-ным синдромом оставались жалобы на одышку при минимальной физической нагрузке, миалгии, утомляемость и снижение работоспособности, а также клинические признаки атрофии скелетных мышц. Те же нарушения выявлялись и по истечении 6 месяцев. Таким образом, связь между постковидным синдромом и прогрессированием патологического процесса скелетной мышечной ткани подтверждалась. Наибольший прирост индекса хрупкости (Frailty Index, FI) отмечался в течение первого месяца после разрешения COVID-19 [10].
«Хрупкие» пациенты ожидаемо были старше, чем здоровые индивидуумы. Эти данные согласуются с тем фактом, что накопление дефицитов и снижение физиологических резервов усиливаются с возрастом и, как и ожидалось, с распространённостью слабости. По многочисленным статистическим данным установлено, что лица с диагностированной саркопенией чаще страдали гипертонией и сердечно-сосудистыми заболеваниями, чем пациенты, у которых саркопения отсутствовала [19].
В одном из недавно проведённых исследований [20] выявлена отчётливая связь между сарко-пенией и длительными проявлениями COVID-19. Следует отметить, что вывод сделан авторами на основании данных, полученных при обследовании гетерогенной группы больных, включавшей не только пациентов, которые лишь подозревали наличие у них заболевания (без клинического или тестового диагноза), но и тех, у кого инфекция SARS-CoV-2 была верифицирована. Более того, мышечная слабость констатировалась не с помощью валидизиро-ванных тестов, а путём стандартного анкетирования об уровне физической подготовки.
Результаты наблюдений T. Shinohara и соавт. [21] за пожилыми людьми с астенией, проживающими в японских общинах, показали объективное снижение у них силы сгибателей мышц нижних конечностей.
Известно, что саркопения, остро развивающаяся на фоне COVID-19, вследствие гиподинамии, снижения мотивации к регулярным нагрузкам и дефицита белкового питания нередко модифицируется в хроническую форму [22, 23]. По некоторым аналитическим данным [24], генерализованная атрофия скелетных мышц может быть обусловлена повышением уровня ангиотензина II по альтернативному пути и снижением уровня ангиотензинпревращающего фермента 2 (angiotensin-converting enzyme 2, ACE2).
У пациентов с саркопенией отмечается ослабление мышц, участвующих в акте дыхания, что осложняет лечение ковидассоциированной пневмонии и острого респираторного дистресс-синдрома, ухудшает прогноз постковидного синдрома [25]. Часто у пожилых лиц с астенией отмечается появление одышки de novo через 1–3 месяца после выписки из стационара, что может свидетельствовать о развитии саркопени-ческой респираторной недостаточности [26].
Таким образом, последствия вирусной инвазии SARS-CoV-2 оказываются крайне неблагоприятными для пациентов пожилого и старческого возраста ввиду ускоренного катаболизма мышечной ткани и прогрессирования уже имеющейся симптоматики старческой астении и коморбидных заболеваний [27].
БИОХИМИЧЕСКИЕ, ГЕНЕТИЧЕСКИЕИ ЭПИГЕНЕТИЧЕСКИЕ ПРЕДИКТОРЫ РАЗВИТИЯ МЫШЕЧНОЙ СЛАБОСТИВ ПОСТКОВИДНОМ ПЕРИОДЕ
Симптомы поражения скелетной мускулатуры (мышечная боль/миалгия), мышечная слабость (от умеренной до выраженной), усталость и непереносимость физических нагрузок наблюдаются не только в остром, но и отдалённом постковид-ном периоде (так называемый long-COVID) [28, 29]. Миалгия и артралгия чаще возникают в отделении интенсивной терапии у пациентов с вынужденной длительной иммобилизацией [30]. Высокая распространённость этих симптомов указывает на стойкие структурные и функциональные изменения в скелетных мышцах у пациентов с COVID-19. Исследования, проведённые в группах, различных по полу и возрасту, продемонстрировали примерно у 53–63% пациентов наличие одышки, усталости и мышечной слабости [31, 32]. Указанная симпто- матика чаще встречалась у женщин и пациентов с тяжёлым течением COVID-19 [33, 34].
У отдельных заболевших тяжёлой формой COVID-19 с вынужденной иммобилизацией в отделении реанимации и интенсивной терапии площадь поперечного сечения прямой мышцы бедра уменьшилась на 30%, толщина переднего отдела четырёхглавой мышцы бедра — почти на 20% спустя 10 дней после их поступления в стационар. В постковидном периоде слабость разгибателей нижних и сгибателей верхних конечностей выявлялась у 75–85% пациентов в возрастном диапазоне от 40 до 88 лет [35]. Лица с ранее диагностированной саркопенией в 2 раза больше времени провели в стационаре, и уровень смертности среди них был в 8 раз выше, чем среди пациентов без саркопении [36].
Значительное количество публикаций посвящено роли SARS-CoV-2 в развитии мышечной сла- бости [37] и качественном изменении мышечных волокон в виде жировой инфильтрации, фиброза, повреждения структурных элементов саркомера (миозинолизиса) у пациентов из группы риска. К предрасполагающим факторам можно отнести гиподинамию, гиповитаминоз, хронические заболевания, женский пол, пожилой и старческий возраст, системное воспаление (рис. 1) [38–42]. В некоторых исследованиях при оценке возможных причин мышечной атрофии обращается внимание на активацию убиквитин-протеасомного пути и белков-каль-паинов [43]. Отмечен также факт повышения в крови креатинкиназы до уровней, сопоставимых с таковыми при рабдомиолизе [44], что указывает на быстрое разрушение скелетных мышц.
В скелетных мышцах пациентов, погибших от COVID-19, выявлены значительная инфильтрация их лейкоцитами и Т-клетками-киллерами, а также признаки дегенерации мышечных волокон [44]. У пациентов с тяжёлой формой COVID-19 и лёгочным фиброзом эти изменения тесно связаны с нарушением сигнального пути трансформирующего фактора роста β (transforming growth factor β , TGF- β ) [45] и повышенной экспрессией ACE2 [24]. Z. Shi и соавт. [46] обратили также внимание на высокую степень фиброза мышечной части диафрагмы. По мнению
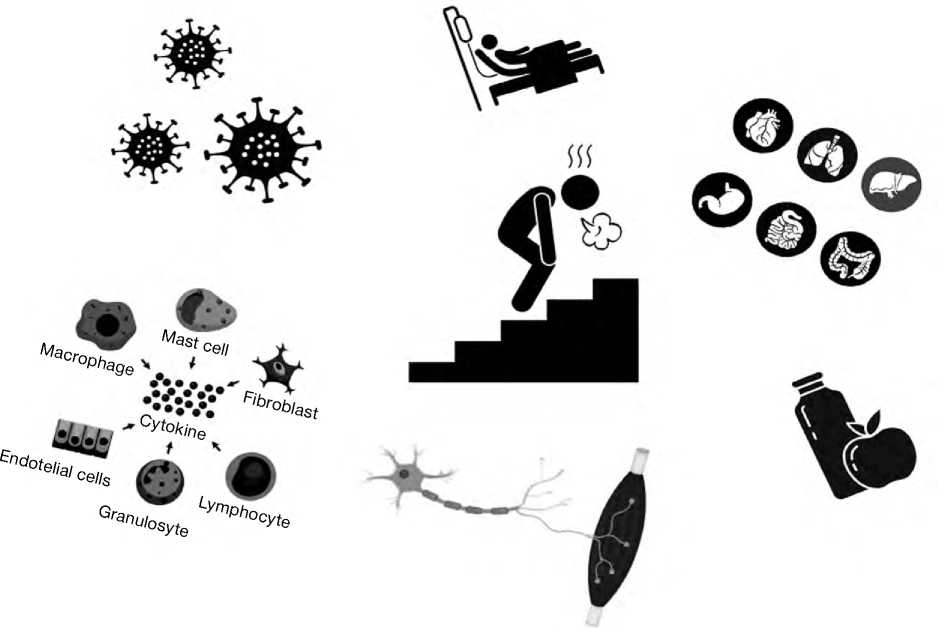
Рис. 1. Мультифакториальность развития генерализованной мышечной слабости у пациентов с постковидным синдромом.
Fig. 1. Multifactorial development of generalized muscle weakness in patients with post-COVID syndrome.
C.J. Walsh и соавт. [47], у пациентов с миопатией критических состояний нарушена экспрессия генов, участвующих в регенерации скелетных мышц и образовании в них межклеточного матрикса, что, возможно, может способствовать развитию фиброза. T. Yang и соавт. [48] считают, что изменения метаболизма в мышечной ткани при саркопении пожилых связаны с белком-миокином GDF-15. Эти заключения могут стать важным ключом к пониманию механизмов возникновения стойкой мышечной слабости у пациентов с постковидным синдромом.
Известно, что вирус SARS-CoV-1 поражает скелетные мышцы посредством прямой вирусной инвазии, поскольку рецептор ACE2 широко экспрессируется в тканях опорно-двигательной системы [49]. Предполагается, что SARS-CoV-2, взаимодействуя с ACE2, проникает непосредственно в мышечные волокна. Основной мишенью вируса являются миобласты, что объясняет потерю регенеративных способностей скелетных мышц в постковидном периоде, поскольку миобласты не способны к активной дифференцировке, восстановлению структурных изменений, возникших при инфицировании [50].
Другими потенциальными механизмами поражения скелетной мускулатуры в остром и постко-видном периоде являются активация миотоксиче-ских цитокинов, отложение иммунных комплексов в мышцах, поражение мышечных мембран миоцитов вирусными антигенами [51–53].
Гиподинамия является, пожалуй, главным предиктором развития мышечной слабости, будь это вынужденная длительная иммобилизация пациентов с тяжёлой формой COVID-19 в отделении реанимации и интенсивной терапии или изначально низкая физическая активность. Каждая из причин изменяет метаболические и сократительные свойства скелетных мышц, что приводит к дальнейшему снижению их функциональности, формируя порочный круг [54].
Ряд зарубежных публикаций описывает случаи, доказывающие, что кратковременное (до 10 дней) отсутствие двигательной активности может способствовать потере общей мышечной массы на 5%, а длительное (до 6 недель) — на ~20% [52]. Снижение мышечной силы в значительной степени объясняется ослаблением сократительной функции из-за уменьшения площади поперечного сечения мышечных волокон. Быстрее всего подвергаются атрофии мышечные волокна II типа, способные к интенсивной, но кратковременной работе. Поскольку волокна II типа вырабатывают в 5 раз больше энергии, чем волокна I типа, их атрофия приводит к снижению выносливости, что оказывает большее негативное влияние на повседневную активность больных, чем непосредственно снижение мышечной силы [55].
Объективным критерием степени поражения мышц, по мнению R. Ram i rez-V e lez и соавт. [50], может служить индекс ALMI (Appendicular Lean Mass Index) — соотношение суммы мышечной массы верхних и нижних конечностей (ALM) к квадрату роста (height): ALMI=(ALM/height2). Согласно рекомендациям Европейской рабочей группы по саркопении у пожилых людей (European Working Group on Sarcopenia in Older People, EWGSOP), показатели ALMI <6,0 кг/м2 у женщин и <7,0 кг/м2 у мужчин являются нижними пороговыми значениями общей мышечной массы [18]. У пациентов с постковидным синдромом критическое снижение мышечной массы, оценённое на основании индекса ALMI, показателей физической активности с использованием международного опросника IPAQ (International Questionnaire on Physical Activity), силы хвата, измеренной с помощью динамометра, выявляется значительно чаще по сравнению с неинфицированными пациентами.
Длительная иммобилизация не только приводит к потере мышечной массы и силы, но и провоцирует метаболические нарушения, которые в свою очередь приводят к повышенной утомляемости, непереносимости физических нагрузок и снижению максимального потребления кислорода вследствие снижения плотности митохондрий и способности к окислительному фосфорилированию [56, 57].
Стоит отдельно упомянуть о влиянии кортикостероидов, применяемых для лечения COVID-19, на развитие мышечной слабости. У пациентов с тяжёлым течением COVID-19 при назначении глюкокортикоидов достоверно снижались сила хвата и пройденное за определённый промежуток времени расстояние, что свидетельствовало о негативном воздействии высоких дозировок данного лекарственного препарата на функцию скелетных мышц, но отсутствие корреляции между дозой гидрокортизона и уменьшением площади поперечного сечения четырёхглавой мышцы бедра свидетельствует, что роль лекарственных препаратов в формировании стойкой мышечной слабости не столь значительна [30].
КРАТКИЙ ОБЗОР ТЕРАПЕВТИЧЕСКОГО ПОДХОДА К ГЕНЕРАЛИЗОВАННОЙ МЫШЕЧНОЙ СЛАБОСТИ
Определяющим при выборе средств и методов лечения мышечной слабости у пациентов в постко- видном периоде, безусловно, является интегративный подход. Реабилитация пациентов, перенёсших COVID-19 в тяжёлой и лёгкой форме, предполагает ежедневное выполнение физических упражнений с отягощением с учётом переносимости нагрузок; обязательную медикаментозную, нутритивную и психологическую поддержку. Силовые тренировки имеют доказанную эффективность в лечении всех форм мышечной слабости. Физические упражнения уменьшают местное и системное воспаление, способствуют коррекции метаболических нарушений [58, 59]. Отдельного внимания заслуживает изучение применения высокоинтенсивного интервального тренинга (High Intensive Interval Trening, HIIT) в качестве ведущего метода физической реабилитации ослабленных пациентов [60]. Нагрузка должна тщательно оцениваться врачами лечебной физкультуры, реабилитологами; план тренировок и веса отягощений должен соответствовать самочувствию и возможностям пациента, так как у ряда больных с PASC недомогание после физической нагрузки, мышечные боли являются фактором, осложняющим продолжение восстановительного лечения.
Единый терапевтический алгоритм лечения сар-копении в настоящее время не определён. Расширение областей исследования в данном направлении следует рассматривать с позиции первостепенной важности относительно восстановления пациентов с COVID-ассоциированной мышечной слабостью.
Генерализованная мышечная слабость, миалгия, ограничение двигательной активности являются ключевыми симптомами пациентов в постковид-ном периоде. Аналитические данные свидетельствуют о том, что в основе этих симптомов могут лежать потеря мышечной массы и силы вследствие дизрегуляции миокинов, снижение уровня ACE2 в мышечной ткани, атрофия, фиброз мышечных волокон. Усугубляющими факторами являются непосредственная инвазия SARS-CoV-2 в скелетные мышцы, инициированное цитокиновым штормом системное воспаление, гипоксемия, вынужденная длительная гиподинамия, недостаточное белковое питание, коморбидные заболевания, побочный эффект приёма глюкокортикоидов.
Саркопения чаще констатируется у пациентов с длительным пребыванием в стационаре. При её развитии отмечается снижение силы мышц, в том числе участвующих в акте дыхания, что осложняет лечение ковидассоциированной пневмонии и острого респираторного дистресс-синдрома, ухудшает прогноз и, кроме того, обусловливает значительно более высокий уровень смертности от коронавирусной инфекции COVID-19 [2, 26, 36]. Потеря мышечной массы является предполагаемой достоверной причиной развития и прогрессирования функциональных ограничений у пациентов старшего возраста не только в постковидном и лонгковидном периоде, при этом отягчающим фактором служит наличие ко-морбидных заболеваний [61].
ЗАКЛЮЧЕНИЕ
Бесспорно, необходимо дальнейшее, более углублённое исследование форм мышечной патологии в постковидном периоде. Не менее важно создание клинических рекомендаций для врачей поликлиник и стационаров, предоставляющих возможность правильно диагностировать и лечить проявления мышечной слабости и астении у гериатрических больных.
ДОПОЛНИТЕЛЬНАЯ ИНФОРМАЦИЯ
Источник финансирования. Авторы заявляют об отсутствии внешнего финансирования при проведении поисково-аналитической работы.
Список литературы Постковидная астения, саркопения и генерализованная мышечная слабость у гериатрических больных
- Веселова Д.К., Белопасов В.В. Старческая астения и старческая апатия в повседневной клинической практике в условиях пандемии новой коронавирусной инфекции COVID-19 // Клиническая практика. 2022. Т. 13, № 1. C. 66–78. [Veselova DK, Belopasov VV. Frailty and senile apathy in the everyday clinical practice in the conditions of COVID-19. J Clin Pract. 2022;13(1): 66–78]. EDN: ZRCWPY doi: 10.17816/clinpract104831
- Dennis A, Wamil M, Alberts J, et al. Multiorgan impairment in lowrisk individuals with post-COVID-19 syndrome: A prospective, community-based study. BMJ Open. 2021;11(3):e048391. EDN: GWXGCT doi: 10.1136/bmjopen-2020-048391
- Kim JW, Yoon JS, Kim EJ, et al. Prognostic implication of baseline sarcopenia for length of hospital stay and survival in patients with coronavirus disease 2019. J Gerontol A Biol Sci Med Sci. 2021;76(8):e110–e116. doi: 10.1093/gerona/glab085
- Rovere Querini P, De Lorenzo R, Conte C. Post-COVID-19 follow-up clinic: Depicting chronicity of a new disease. Acta Biomed. 2020;20(9-S):22–28. doi: 10.23750/abm.v91i9-S.10146
- Rovere-Querini P, Tresoldi C, Conte C, et al. Biobanking for COVID-19 research. Panminerva Med. 2022;64(2):244–252. EDN: OPROIG doi: 10.23736/S0031-0808.20.04168-3
- Malmstrom TK, Morley JE. SARC-F: A simple questionnaire to rapidly diagnose sarcopenia. JAMDA. 2013;14(8):531–532. doi: 10.1016/j.jamda.2013.05.018
- Rubenstein LZ, Harker JO, Salva A, et al. Screening for undernutrition in geriatric practice: Developing the shortform mini-nutritional assessment (MNA-SF). J Gerontol. 2001;56(6):M366–372. doi: 10.1093/gerona/56.6.m366
- Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothlialitis, thombosis, and angiogenesis in COVID-19. NEJM. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432
- Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265–1273. EDN: RIODCA doi: 10.1001/jamacardio.2020.3557
- Damanti S, Cilla M, Cilona M, et al. Prevalence of long COVID-19 symptoms after hospital dischargein frail and robust patients. Front Med. 2022;(9):834887. EDN: OMKZAO doi: 10.3389/fmed.2022.834887
- Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID- 19 in a multistate health care systems network-- United States. Morbid Mortal Wkly Rep. 2020;69(30):993–998. doi: 10.15585/mmwr.mm6930e1
- Raveendran AV. Long COVID-19: Challenges in the diagnosis and proposed diagnostic criteria. Diabetes Metab Syndr. 2021;15(1):145–146. doi: 10.1016/j.dsx.2020.12.025
- Белопасов В.В., Яшу Я., Самойлова Е.М., Баклаушев В.П. Поражение нервной системы при СOVID-19 // Клиническая практика. 2020. Т. 11, № 2. C. 60–80. [Belopasov VV, Yashu Y, Samoilova EM, Baklaushev VP. Nervous system damage in SOVID-19. J Clin Pract. 2020;11(2):60–80]. EDN: JLSSLO doi: 10.17816/clinpract34851
- Piotrowicz K, Gąsowski J, Michel JP, Veronese N. Post-COVID-19 acute sarcopenia: Physiopathology and management. Aging Clin Exp Res. 2021;33(10):2887–2898. EDN: RHRMZN doi: 10.1007/s40520-021-01942-8
- De Giorgio MR, Di Noia S, Morciano C, Conte D. The impact of SARS-CoV-2 on skeletal muscles. Acta Myol. 2020;39(4): 307–312. doi: 10.36185/2532-1900-034
- Van Seben R, Reichardt LA, Aarden JJ, et al. The course of geriatric syndromes in acutely hospitalized older adults: The hospital-ADL study. J Am Med Dir Assoc. 2019;20(2):152–158.e2. doi: 10.1016/j.jamda.2018.08.003
- Reichardt LA, van Seben R, Aarden JJ, et al. Trajectories of cognitive-affective depressive symptoms in acutely hospitalized older adults: The hospital-ADL study. J Psychosom Res. 2019;(120):66–73. doi: 10.1016/j.jpsychores.2019.03.011
- Hoyer EH, Needham DM, Atanelov L, et al. Association of impaired functional status at hospital discharge and subsequent rehospitalization. J Hosp Med. 2014;9(5):277–282. doi: 10.1002/jhm.2152
- Bellelli G, Rebora P, Valsecchi MG, et al.; COVID-19 Monza Team Members. Frailty index predicts poor outcome in COVID-19 patients. Intensive Care Med. 2020;46(8):1634–1636. EDN: SEPGUS doi: 10.1007/s00134-020-06087-2
- Jones R, Davis A, Stanley B, et al. Risk predictorsand symptom features of long COVID within a broad primary care patientpopulation including both tested and untested patients. Pragmat Obs Res. 2021;(12):93–104. doi: 10.2147/POR.S31618638
- Shinohara T, Saida K, Tanaka S, Murayama A. Association between frailty and changes in lifestyle and physical or psychological conditions among older adults affected by the coronavirus disease 2019 countermeasures in Japan. Geriatr Gerontol Int. 2021;21(1):39–42. doi: 10.1111/ggi.14092
- Damanti S, Azzolino D, Roncaglione C, et al. Efficacy of nutritional interventions as stand-alone or synergistic treatments with exercise for the management of sarcopenia. Nutrients. 2019;11(9):1991. doi: 10.3390/nu11091991
- Yamada M, Kimura Y, Ishiyama D, et al. Effect of the COVID-19 epidemic on physical activity in communitydwelling older adults in Japan: A cross-sectional online survey. J Nutr Health Aging. 2020;24(9):948–950. EDN: HPTQJB doi: 10.1007/s12603-020-1424-2
- Bahat G. COVID-19 and the renin angiotensin system: Implications for the older adults. J Nutr Health Aging. 2020; 24(7):699–704. EDN: SIOIYR doi: 10.1007/s12603-020-1403-7
- Ohara DG, Pegorari MS, Dos Santos NL, et al. Respiratory muscle strength as a discriminator of sarcopenia in community-dwelling elderly: A cross-sectional study. J Nutr Health Aging. 2018; 22(8):952–958. EDN: HWRFVK doi: 10.1007/s12603-018-1079-4
- Белопасов В.В., Белопасова А.В., Веселова Д.К. Инволюционные формы патологии скелетной мускулатуры // Медицинский алфавит. 2022. № 32. С. 17–24. [Belopasov VV, Belopasova AV, Veselova DK. Involutionary forms of skeletal muscle pathology. Meditsinskii alfavit. 2022;(32):17–24]. EDN: WUXSUA doi: 10.33667/2078-5631-2022-32-17-24
- Barnes M, Heywood AE, Mahimbo A, et al. Acute myocardial infarction and influenza: A meta-analysis of case-control studies. Heart. 2015;101(21):1738–1747. doi: 10.1136/heartjnl-2015-307691
- Soares MN, Eggelbusch M, Naddaf E, et al. Skeletal muscle alterations in patients with acute COVID-19 and post-acute sequelae of COVID-19. J Cachexia Sarcopenia Muscle. 2022;13(1):11–22. EDN: TAXEUE doi: 10.1002/jcsm.12896
- Carfi A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–605. doi: 10.1001/jama.2020.12603
- Pleguezuelos E, del Carmen A, Llorensi G, et al. Severe loss of mechanical efficiency in COVID-19 patients. J Cachexia Sarcopenia Muscle. 2021;12(4):1056–1063. doi: 10.1002/jcsm.12739
- Gautam N, Madathil S, Tahani N, et al. Medium-term outcome of severe to critically ill patients with SARS-CoV-2 infection. Clin Infect Dis. 2022;74(2):301–308. doi: 10.1093/cid/ciab341
- Huang C, Huang L, Wang Y, et al. 6-Month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet. 2021;397(10270):220–232. doi: 10.1016/S0140-6736(20)32656-8
- Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–631. EDN: KSEJGQ doi: 10.1038/s41591-021-01292-y
- Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–615. doi: 10.1038/s41591-021-01283-z
- De Andrade-Junior MC, de Salles IC, de Brito CM, et al. Skeletal muscle wasting and function impairment in intensive care patients with severe COVID-19. Front Physiol. 2021;(12):640973. doi: 10.3389/fphys.2021.640973
- Paneroni M, Simonelli C, Saleri M, et al. Muscle strength and physical performance in patients without previous disabilities recovering from COVID-19 pneumonia. Am J Phys Med Rehabil. 2021;100(2):105–109. EDN: RMAPLN doi: 10.1097/PHM.0000000000001641
- Kim JW, Yoon JS, Kim EJ, et al. Prognostic implication of baseline sarcopenia for length of hospital stay and survival in patients with coronavirus disease 2019. J Gerontol A Biol Sci Med Sci. 2021;76(8):e110–e116. doi: 10.1093/gerona/glab085
- Yang T, Li Z, Jiang L, et al. Risk factors for intensive care unitacquired weakness: A systematic review and meta-analysis. Acta Neurol Scand. 2018;138(2):104–114. doi: 10.1111/ane.12964
- Mohammadi B, Schedel I, Graf K, et al. Role of endotoxin in the pathogenesis of critical illness polyneuropathy. J Neurol. 2008;255(2):265–272. doi: 10.1007/s00415-008-0722-0
- Lacomis D, Giuliani MJ, van Cott A, Kramer DJ. Acute myopathy of intensive care: Clinical, electromyographic, and pathological aspects. Ann Neurol. 1996;40(4):645–654. doi: 10.1002/ana.410400415
- Al-Lozi MT, Pestronk A, Yee WC, et al. Rapidly evolving myopathy with myosin-deficient muscle fibers. Ann Neurol. 1994;35(3):273–279. doi: 10.1002/ana.410350306
- Bierbrauer J, Koch S, Olbricht C, et al. Early type II fiber atrophy in intensive care unit patients with nonexcitable muscle membrane. Crit Care Med. 2012;40(2):647–650. doi: 10.1097/CCM.0b013e31823295e6
- Wollersheim T, Woehlecke J, Krebs M, et al. Dynamics of myosin degradation in intensive care unit-acquired weakness during severe critical illness. Intensive Care Med. 2014;40(4):528–538. doi: 10.1007/s00134-014-3224-9
- Aschman T, Schneider J, Greuel S, et al. Association between SARS-CoV-2 infection and immune-mediated myopathy in patients who have died. JAMA Neurol. 2021;78(8):948–960. doi: 10.1001/jamaneurol.2021.2004
- Stukalov A, Girault V, Grass V, et al. Multilevel proteomics reveals host perturbations by SARS-CoV-2 and SARS-CoV. Nature. 2021;594(7862):246–252. EDN: AJPQPV doi: 10.1038/s41586-021-03493-4
- Shi Z, de Vries HJ, Vlaar AP, et al. Diaphragm pathology in critically ill patients with COVID-19 and postmortem findings from 3 medical centers. JAMA Intern Med. 2021;181(1):122–124. doi: 10.1001/jamainternmed.2020.6278
- Walsh CJ, Batt J, Herridge MS, et al. Transcriptomic analysis reveals abnormal muscle repair and remodeling in survivors of critical illness with sustained weakness. Sci Rep. 2016;(6):29334. doi: 10.1038/srep29334
- Yang T, Li Z, Jiang L, et al. Risk factors for intensive care unitacquired weakness: A systematic review and meta-analysis. Acta Neurol Scand. 2018;138(2):104–114. doi: 10.1111/ane.12964
- Leung TW, Wong KS, Hui AC, et al. Myopathic changes associated with severe acute respiratory syndrome: A postmortem case series. Arch Neurol. 2005;62(7):1113–1117. doi: 10.1001/archneur.62.7.1113
- Ramírez-Vélez R, Legarra-Gorgoñon G, Oscoz-Ochandorena S, et al. Reduced muscle strength in patients with long-COVID-19 syndrome is mediated by limb muscle mass. J Appl Physiol (1985). 2023;134(1):50–58. EDN: HYPAJI doi: 10.1152/japplphysiol.00599.2022
- Rudroff T, Workman CD, Ponto LL. 18 F-FDG-PET imaging for post-COVID-19 brain and skeletal muscle alterations. Viruses. 2021;13(11):2283. doi: 10.3390/v13112283
- Han Q, Zheng B, Daines L, Sheikh A. Long-term sequelae of COVID-19: A systematic review and meta-analysis of oneyear follow-up studies on post-COVID symptoms. Pathogens. 2022;11(2):269. EDN: BPFUTB doi: 10.3390/pathogens11020269
- Medrinal C, Prieur G, Bonnevie T, et al. Muscle weakness, functional capacities and recovery for COVID-19 ICU survivors. BMC Anesthesiol. 2021;21(1):64. EDN: GCASJI doi: 10.1186/s12871-021-01274-0
- Marusic U, Narici M, Simunic B, et al. Nonuniform loss of muscle strength and atrophy during bed rest: A systematic review. J Appl Physiol (1985). 2021;131(1):194–206. doi: 10.1152/japplphysiol.00363.2020
- Tanriverdi A, Savci S, Kahraman BO, Ozpelit E. Extrapulmonary features of post-COVID-19 patients: Muscle function, physical activity, mood, and sleep quality. Ir J Med Sci. 2022;191(3): 969–975. EDN: IBYBRG doi: 10.1007/s11845-021-02667-3
- Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143–1211. EDN: NTJJCW doi: 10.1002/cphy.c110025
- Hyatt H, Deminice R, Yoshihara T, Powers SK. Mitochondrial dysfunction induces muscle atrophy during prolonged inactivity: A review of the causes and effects. Arch Biochem Biophys. 2019;(662):49–60. EDN: YJWJYF doi: 10.1016/j.abb.2018.11.005
- Bij de Vaate E, Gerrits KH, Goossens PH. Personalized recovery of severe COVID19: Rehabilitation from the perspective of patient needs. Eur J Clin Invest. 2020;50(7):e13325. doi: 10.1111/eci.13325
- Valente AF, Jaspers RT, Wüst RC. Regular physical exercise mediates the immune response in atherosclerosis. Exerc Immunol Rev. 2021;27:42–53.
- Atakan MM, Li Y, Kosar SN, et al. Evidence-based effects of high-intensity interval training on exercise capacity and health: A review with historical perspective. Int J Environ Res Public Health. 2021;18(13):7201. doi: 10.3390/ ijerph18137201
- Белопасов В.В., Журавлева Е.Н., Нугманова Н.П., Абдрашитова А.Т. Постковидные неврологические синдромы // Клиническая практика. 2021. Т. 12, № 2. C. 69–82. [Belopasov VV, Zhuravleva EN, Nugmanova NP, Abdrashitova AT. Post-Covid-19 neurological syndromes. J Clin Pract. 2021;12(2): 69–82]. EDN: MZQWAN doi: 10.17816/clinpract71137