Постковидные неврологические синдромы
Автор: Белопасов Владимир Викторович, Журавлева Екатерина Николаевна, Нугманова Наталья Павловна, Абдрашитова Аделя Тафкильевна
Журнал: Клиническая практика @clinpractice
Рубрика: Обзоры
Статья в выпуске: 2 т.12, 2021 года.
Бесплатный доступ
В статье освещены патогенез, клинические проявления поражения центральной и периферической нервной системы, возникшие или сохраняющиеся у больных в постковидном периоде (Long-COVID-19). Их правильная оценка, использование эффективных методов комплексного лечения, направленной нейрореабилитации способствуют обратимости функциональных нарушений, предотвращению, снижению инвалидности, повышению показателей качества жизни, предупреждению прогрессирования когнитивных, эмоциональных, поведенческих расстройств, инициированных SARS-CoV-2.
Подострый, хронический covid-19, заболевания центральной и периферической нервной системы
Короткий адрес: https://sciup.org/143175853
IDR: 143175853 | DOI: 10.17816/clinpract71137
Текст обзорной статьи Постковидные неврологические синдромы
Submitted 25.05.2021
Revised 02.06.2021
Published 30.06.2021
Список сокращений
|
КТ — компьютерная томография |
СOVID-19 (Coronavirus Disease 2019) — коронави- |
|
КФК — креатинфосфокиназа |
русная инфекция 2019 года |
|
МРТ — магнитно-резонансная томография |
SARS-CoV-2 (severe acute respiratory syndrome-related coronavirus 2) — новый коронавирус тяжело- |
|
ПЭТ — позитронно-эмиссионная томография |
го острого респираторного синдрома 2 |
АКТУАЛЬНОСТЬ
Знание клинических форм, их комбинаций, диагностических алгоритмов и методов объективной оценки, характерных для постковидного пери- ода функциональных и структурных изменений в головном мозгу, вегетативной и периферической нервной системе, важно не только для постановки диагноза, выбора фармакотерапии и методов
КТ ГА
нейрореабилитации, но и для прогнозирования полученных результатов, обоснования профилактических мер для предотвращения негативного влияния перенесенного заболевания на физическое, социальное, психическое благополучие больного, предупреждения негативных исходов в виде потери трудоспособности, инвалидности и отсроченных долгосрочных последствий коронавирусной инфекции (хронической ангиоэнцефалопатии, структурной эпилепсии, паркинсонизма, лейкоэнцефалопатии, других прогрессирующих форм ней-родегенеративной и аутоиммунной патологии).
В период продолжающейся пандемии COVID-19 оценка больного, перенесшего COVID-19, лечащим врачом (неврологом, физиотерапевтом, реабилито-логом, психотерапевтом) определяется состоянием его здоровья на момент обращения, наличием выявленных у него в острой фазе клинических проявлений и осложнений, успешностью проводимой терапии, а также сохраняющимися последствиями заболевания, негативно влияющими на качество жизни. Глава Европейского регионального бюро Всемирной организации здравоохранения Ханс Клюге заметил: «Худший сценарий позади. Мы знаем о коронавирусе больше по сравнению с 2020 годом, когда он только начал распространяться». Механизмы инвазии и клинические проявления SARS-CoV-2 до попадания и в период пребывания больного в стационаре в основном охарактеризованы [1–5], а возникающие и сохраняющиеся при лечении на дому, а также после выписки из инфекционного отделения на долечивание и реабилитацию — требуют осмысления.
В представленном нами обзоре речь пойдет о неврологических осложнениях и психосоматических расстройствах в постковидном периоде, с которыми встречаются врачи на поликлиническом приеме и в стационарах.
Уже в первые месяцы после объявления Всемирной организацией здравоохранения о начале пандемии и необходимости управления ее последствиями [6] при функциональной оценке состояния больных на всех этапах заболевания были очерчены временные сроки появления и сохранения клинических симптомов, отражающих его тяжесть и локализацию в зависимости от повреждения органа/органов и систем-мишеней; разработаны, а впоследствии уточнены типы и подтипы синдрома long COVID [7, 8]:
-
• для 1-го типа (острый COVID-19) характерно развитие плохо или недостаточно курабельных
дефицитарных структурных нарушений в периоде инфицирования заболевшего;
-
• для 2-го типа — сохраняющиеся симптомы в течение 4–12 нед. после заражения COVID-19;
-
• для 3-го типа (long COVID, long haulers — постко-видный, затяжной/longhaul COVID-19 синдром, более 12 нед.) — течение непрерывное, рецидивирующее, ремиттирующее (≥3 мес — подтип 3A , ≥6 мес — подтип 3B ) после почти полного выздоровления или редукции первоначальных симптомов;
-
• для 4-го типа — при бессимптомном течении острого периода внезапное развитие органной патологии спустя 1–3 мес ( подтип 4А ) или более ( подтип 4B );
-
• для 5-го типа — летальный исход, причинносвязанный со скрытно протекающим заболеванием легких, миокарда, питающих их и мозг сосудов [9, 10].
Такой подход позволяет осуществлять диагностику, лечение и реабилитацию больных независимо от их возраста вне ковидных госпиталей. Сохраняющиеся или вновь возникающие симптомы, функциональные нарушения, связанные с COVID-19, в ≥50% случаев, по данным анкетирования и анализу исходов заболевания в стационарах и поликлиниках, негативно отражаются на качестве жизни, мобильности и независимости обратившихся за медицинской помощью больных [11–14].
К симптомам, требующим внимания невролога, относятся вновь возникшая или сохраняющаяся локальная боль; тахикардия; непродуктивный, не-купируемый бронхо- и муколитиками надсадный кашель; периодическое падение уровня сатурации при пульсоксиметрии; одышка; парестезии; диплопия; икота; снижение/потеря обоняния, вкуса, зрения, слуха; утомляемость; несистемное головокружение; плохая переносимость физических нагрузок; потеря аппетита, мышечной массы; внезапное «выключение» сознания; фокальные и генерализованные судороги; изменение настроения, речи, походки; нарушение глотания, координации, памяти, поведения, сна, терморегуляции; наличие или прогрессирование слабости, онемения в конечностях [15, 16].
Цефалгия. Основными типами ее при исключении «красных» и «оранжевых флагов» [17] являются эпизодическая или перманентная головная боль напряжения; кашлевая, возникающая при физических и когнитивных нагрузках головная боль; ком-
<линическая 2021 п эакти keu Том 12 №2
прессионная/ишемическая (от сдавления перикра-ниальных мышц, скальпа, мягких тканей, сосудов защитными шлемами, масками, очками), вторичная головная боль (при воспалении придаточных пазух носа, менингоэнцефалите, диффузной лейкоэнцефалопатии, васкулите, эпидуральной гематоме, церебральном инсульте, тромбозе синусов и вен, кровоизлиянии в гипофиз, внутричерепной гипертензии, гипоксии, гиперкапнии, отеке мозга) [18, 19], а также новая (ранее отсутствующая), пульсирующая или давящая, от умеренной до сильной, голокраниальная, продолжительная (более 72 ч), мигренеподобная, связанная с активацией тригеминоваскулярной системы, резистентная к стандартной терапии головная боль, ассоциированная с системной вирусной инфекцией (поражением легких, повышенными уровнями в крови D-димера, IL-6, TNF-α, тромбоцитопенией, лимфопенией, гиперферритинемией) [20–22]. Изменение частоты, выраженности приступов, повышение доз препаратов по сравнению с периодом до пандемии, трансформация в хроническую форму имеют место при наличии мигрени у больных до инфицирования SARS-CoV-2 [23]. Особенностью постковидной ми- гренеподобной цефалгии является ее сохранение более 6 недель при исчезновении других симптомов COVID-19 [24, 25]. Развитие псевдомигреноз-ной, орофациальной, височно-мандибулярной, ма-стикаторной боли обычно связано с психогенным стрессом или локальным миозитом [26, 27].
Краниопатии. Дебютирующие в остром периоде заболевания нарушения обоняния, вкуса, зрения и слуха чаще всего обратимы в течение первых 3 нед. [4, 28, 29]. Отсутствие или частичное восстановление системы чувств наблюдается при воспалительных невропатиях I, II, IV, VII, VIII черепных нервов [30–34], ятрогенном повреждении X, XII нервов (синдром Тапиа) после интубации трахеи [35]. Вовлечение в патологический процесс II, III, V, VI нервов возможно при тромбозе кавернозного синуса [36], III, VII, IX, X, XII — при стволовом инсульте (собственное наблюдение; рис. 1), аутоиммунных осложнениях (синдромы Гийена–Барре, Миллера Фишера) [37, 38], X — при сенсорной ларингеальной невропатии (sensory laryngeal neuropathy, SLN) [39], постинфекционной вирусной вагусной невропатии (postviral vagal neuropathy, PVVN), клинически проявляющихся в виде упорного, толерантно-
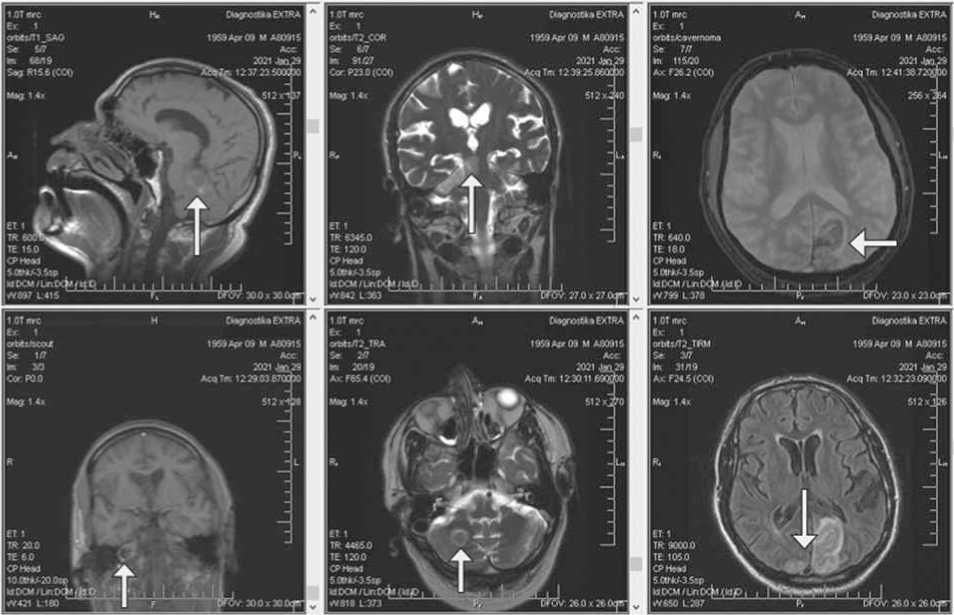
Рис. 1. Артерио-артериальная церебральная эмболия ветвей базилярной артерии. Гемисиндром ствола мозга, мозжечка справа. Асимметричные инфаркты затылочных долей.
Fig. 1. Arterio-arterial cerebral embolism of basial artery branches. Right-side hemi-syndrome of the brainstem, cerebellum. Asymmetric infarctions of occipital lobes.

Рис. 2. Злокачественный отечный экзофтальм Грейвса. Хемоз, офтальмоплегия.
Fig. 2. Malignant edematous Graves’ exophthalmos. Chemosis, ophthalmoplegia.
го к терапии кашля, купируемого при назначении амитриптилина, габапентина [40, 41].
Аутоиммунные осложнения — больные с воспалительными демиелинизирующими полиради-кулоневропатиями (синдром Гийена–Барре, синдром Миллера Фишера), лейкоэнцефалопатией, аутоиммунным энцефалитом, ромбэнцефалитом Бикерстаффа, лимбическим энцефалитом, ан-ти-NMDAR-энцефалитом, острым диссеминированным энцефаломиелитом, поперечным/про-дольным миелитом, оптикомиелитом, рассеянным склерозом, миастенией de novo , множественными мононевритами, цервикобрахиальной плексопа-тией [4, 42–45]. Некоторые из этих форм дебютируют в постковидном периоде [46, 47], одним из драматичных осложнений которого является злокачественный отечный экзофтальм Грейвса (аутоиммунный тиреодит) (собственное наблюдение, рис. 2). Зарегистрированы также единичные случаи поствакцинального поперечного миелита, развитие синдрома Гийена–Барре после COVID-19-вак-цинирования Pfizer [48, 49], однако число больных с поствакцинальными иммуноопосредованными осложнениями не должно возрастать, так как доказательств причинной связи их развития с вакцинацией от COVID-19 пока не имеется.
Дефицитарные формы поражения нервной системы, сохраняющиеся в раннем восстановительном периоде. В продолжении персонализированного лечения и проведении реабилитационных мероприятий с использованием мультидисципли-нарного подхода, традиционных и новых технологий в первые 6 месяцев после выписки из стационара нуждаются больные с частично восстановленными или сохраняющимися речевыми, двигательными, чувствительными, вегетативными, психическими и когнитивными нарушениями. Методы и объем лечения определяются нозологией и формами неврологических осложнений: менингоэнцефалит; энцефалит; лейкоэнцефалит; синдром паркинсонизма, «запертого человека»; церебеллит; ромбэнцефалит Бикерстаффа; лейкоэнцефалопатия; энцефалопатии критических состояний; тромбозы мозговых синусов и церебральных вен; ишемический, геморрагический инсульты; спинальный инсульт; энцефаломиелит; миелит; оптикомиелит; плексопатии; моно-, мульти-, полиневропатии; нейромиопатия; миастения [4, 50–52].
Абдоминалгия. Появление ее при наличии или отсутствии респираторных симптомов может быть связно со спазмом брюшных мышц; кашлевой гры-
<линическая 2021 п эакти keu Том 12 №2
жей живота; кишечной дискинезией; развитием пневмоперитонеума, панкреатита, гепатита, острой печеночной недостаточности, лекарственного гастроэнтерита, колита; обострением имеющихся у больных коморбидных форм желудочно-кишечных заболеваний; диссекцией аорты; аортитом [57–59]; тромбозом брыжеечных, селезеночных артерий или их ветвей [60, собственное наблюдение].
Нейропатическая постковидная боль (острая и хроническая) имеет место при воспалении, ишемии, компрессионном повреждении периферических нервов, сплетений, активации нейронов задних рогов спинного мозга, автономных волокон симпатической нервной системы, вовлечении в патологический процесс таламуса, соматосенсорной коры головного мозга [61, 62]. Основной контигент — больные, выписанные на долечивание и реабилитацию после интенсивной терапии в ко-видном госпитале (post-intensive care syndrome, нейро- и полинейропатии критических состояний, CIN). Сдавление периферических нервов, их ветвей (nerve entrapment sensory neuropathy, NESN) на верхних и нижних конечностях при умеренно выраженном и тяжелом остром респираторном дис-тресс-синдроме возможно в положении лежа на животе. Характерные для нейропатической боли симптомы (наличие парестезий, гиперпатии, аллодинии, признаков автономной дисфункции) типичны для постгерпетической невралгии, диабетической болезненной нейропатии, парестетической ноталгии (поражении паравертебральных задних ветвей спинномозговых нервов и ганглиев), сенсорных периферических невропатий, сенсорной амиотрофической невралгии Персонейджа–Тер-нера, аксональных и демиелинизирующих вариантов воспалительной и параинфекционной полира-дикулоневропатий [63–65]. Развитие центральной постинсультной боли обусловлено поражением таламуса, ствола мозга, спиноталамических трактов [66, 67].
Поражения периферической нервной системы проявляются в виде мононевропатий, множественных невропатий, полиневропатий, плексопа-тий, полирадикулоневропатий, в генезе которых, помимо воспаления и компрессии [68, 69], значимая роль отводится молекулярной мимикрии между вирусными белками и белками периферических нервов (GM1, GD1a, GТ1a, GQ1b) [70, 71].
Постковидные эпилептические приступы. Носительство вируса, проникновение его в нейроны коры головного мозга не инициирует разви- тия эпилептиформной активности, не влияет на клинические характеристики и частоту приступов у больных COVID-19. Важное, но не определяющее значение для эпилептизации нейронов имеет структурно-функциональная дезорганизация в очаге поражения, вызванная воспалительным, аутоиммунным процессом, ишемией мозга в острой стадии заболевания, спровоцированного SARS-CoV-2 [72, 73]. В постковидном периоде эпилептические приступы могут возникать и протекать тяжело (серийно в виде бессудорожного и судорожного эпилептического статуса — билатеральных тонико-клонических, миоклонических судорог или, крайне редко, опсоклонуса-миоклонуса) не только у больных эпилепсией [74, 75]. Возможна связь их развития с невыявленными в преморбидном периоде структурными изменениями иной этиологии (атрофия, склероз гиппокампа, аномалии развития, мальформации, травма мозга) [73].
Синдром хронической усталости (chronic fatigue syndrome, CFS). Синонимы: исландская болезнь; миалгический энцефаломиелит (chronic fatiguesyndrome, also calledmyalgicencephalomyelitis, CFS/ME); эпидемическая нейромиастения; синдром поствирусной астении; постактивная фаза инфекционных синдромов (post-active phase of infectious syndromes, PAPIS); синдром хронической усталости и иммунной дисфункции (chronic fatigue syndrome and immune dysfunction, CFIDS), болезнь непереносимости системной нагрузки (systemic exertion intolerance disease, SEID). Клинические проявления характеризуются различной степенью тяжести, затяжным или волнообразным течением. Основные негативные признаки, такие как диспноэ, плохая переносимость или невозможность выполнения физических и когнитивных нагрузок, не исчезающая после отдыха утомляемость, недомогание после физической нагрузки (post-exertional malaise, PEM), мышечные боли/миалгии различной локализации, сохраняются на протяжении не менее 6 месяцев после перенесенной вирусной инфекции, инициирующей продукцию цитотоксинов, провоспалительных цитокинов и аутоантител против ключевых ферментов, обеспечивающих функционирование митохондрий и саморегуляцию энергетического метаболизма [76, 77]. К причинно-значимым отнесены вирусы гриппа, простого герпеса I, II, VI типа, Эпштейна–Барр, цитомегаловируса, гепатита С, а с 2020 года — SARS-CoV-2 [78, 79]. Симптомы-спутники — субфебрилитет; эпизоды лихорадки, гипергидроза; лимфадено-

кт ГА
патия; лимфоцитопения; сохраняющиеся кашель, стойкая одышка; снижение SpO2 при физической нагрузке; стеснение в груди; мышечная слабость; парестезии; мигрирующие артралгии; фибромиалгия; головная боль; плохая переносимость света, шума; несистемное головокружение; ощущение тумана в глазах, голове (brain fog); синкопоподобные пароксизмы; постуральная скоротечная ортостатическая гипотензия, тахикардия; дисфория; сенсорно-перцептивные, соматизированные, коммуникативные, поведенческие, аффективные расстройства; сексуальная дисфункция; нарушения засыпания, сна, памяти, внимания, осмысливания [80, 81]. Эти осложнения встречаются у 30–50% реконвалесцентов, чаще у женщин, чем у мужчин и детей; их выраженность и стойкость более высока у больных, находившихся на лечении в палатах интенсивной терапии и реанимационных отделениях, с полиорганными и коморбидными формами патологии [82, 83]. Сохраняющиеся негативные сдвиги в физическом и социальном функционировании отрицательно отражаются на качестве жизни, оценке проводимой лекарственной терапии и реабилитации больных [84].
Когнитивные нарушения. Основой их развития и прогрессирования являются сохраняющаяся гипоперфузия мозга; нарушения метаболизма; индуцированное вирусом структурное повреждение нейронов (страдают в той или иной степени отделы мозга, обеспечивающие фиксацию и сохранение памяти, — кора височных, затылочных долей, гиппокамп, миндалевидные ядра, таламус, мозжечок); вторично нарушается функционирование нейрохи- мических механизмов восприятия, усвоения, консолидации информации, необходимой для обеспечения психической, интеллектуальной деятельности индивидуума [85, 86]. Больные с нейрокогнитив-ным дефектом предъявляют жалобы на возникшие проблемы с памятью (усвоение новой информации, понимание, воспроизведение увиденного, услышанного, прочитанного), выполнением повседневной деятельности, общением с окружающими. При оценке нейропсихологического тестирования и двигательной активности выявляются дефекты коммуникативности, внимания, узнавания, понимания, мышления, моторики, запоминания, воспроизведения ряда слов, цифр, фигур. Страдают приспособительное поведение, работоспособность, познавательная деятельность, осмысливание, эпизодическая, процедурная, семантическая, оперативная, фиксационная, кратковременная память, управление финансами, взаимоотношения в семье [87, 88]. Когнитивные нарушения не связаны с приемом лекарств, критическая самооценка когнитивного потенциала сохраняется, степень снижения — в диапазоне от легких до умеренно выраженных нарушений [89, 90]. При выявлении на магнитно-резонансной томограмме (МРТ) и в ликворе маркеров нейродегенеративного процесса, возникшие изменения в когнитивной сфере являются недементны-ми [91, 92], вместе с тем присутствие и репликация коронавируса в структурах и органоидах мозга, наличие «тлеющего» воспалительного процесса, стимулирующего отложение бета-амилоида и тау-белка в нейронах височной доли, относятся к значимым факторам развития болезни Альцгеймера у перенесших COVID-19 и прогрессирования ее, у кого она уже есть [93, 94].
Психические и поведенческие расстройства — неотъемлемая часть постковидного «хвоста» [95, 96]. Память о перенесенной болезни, ее проявлениях, страхе ухода из жизни, возможность рецидива болезни, неполное восстановление физического и психического здоровья, осознание полной или частичной зависимости от окружающих становятся причиной их развития, независимо от того, где и как лечился больной (в реанимационном отделении, палате интенсивной терапии, амбулаторно или самостоятельно). Сохранение, усугубление соматического неблагополучия, появление новых симптомов, неудовлетворенность качеством проводимой терапии, незащищенность порождают в зависимости от типа личности, его самооценки, степени комплаенса и значимости конкретного социального тригерра дезадаптив-ное реагирование невротического и аффективного регистра [97, 98]. К основным клиническим формам относятся психологический дистресс; посттравматическое стрессовое расстройство; астения; дистимия; ангедония; ипохондрия; фобия; тревога; панические атаки, их подтипы; генерализованное тревожное расстройство; катастрофи-зация; навязчивые состояния; депрессия; дизре-гуляторный синдром Алана Бэддели (dysexecutive syndrome, DES) — потеря контроля за поведением при наличии когнитивных и эмоциональных нарушений [99–101]. Эмоциональная неустойчивость проявляется в виде смены настроения, дисфории, раздражительности, плаксивости, вербальной и физической агрессии. Клинически и прогностически столь же значимы расстройства поведения. Больные апатичны, гиподинамичны, предпочита-
<линическая 2021 п эакти keu Том 12 №2
ют постельный режим, самоизоляцию; нарушаются коммуникации с родственниками, друзьями, коллегами по работе; страдают исполнительные функции; снижаются аппетит, мыслительная, двигательная, сексуальная активность. Внимание концентрируется на соматовисцеральных проявлениях, их динамике. Некоторые испытывают cтойкие неприятные обонятельные галлюцинации (паросмия, фантоcмия) [102, 103]. Попытки родственников и врача повлиять на самооценку больного провоцируют психотические реакции, взрывное поведение, конверсионные нарушения, суицид. Негативный вклад в их развитие вносит определяемое (по МРТ, ПЭТ) повреждение вирусом функционально значимых для реализации аффекта зон в передних отделах лобных и височных долей головного мозга [104, 105].
Автономная дисфункция проявляется в колебаниях уровня артериального давления (АД) и частоты сердечных сокращений в покое, при вер-тикализации, малых физических нагрузках, форсированном выдыхании при закрытом носе и рте, задержке дыхания с резким натуживанием (проба Вальсальвы) [106, 107]. При выполнении орто-и клиностатических проб выявляется постуральная ортостатическая гипотензия, ортостатическая тахикардия без гипотензии (postural tachycardia syndrome, POTS) [108, 109]. В положении лежа (у 41% пациентов) и стоя (у 72%) возникают ощущение «проваливания», несистемное головокружение [110]; высока вероятность развития аритмий [111, 112], вазодепрессорного [113, 114], рефлекторного обморока (никтурического, при дефекации) [115], кардиомиопатии Такоцубо — обратимой дискинезии левого желудочка сердца, угрожающей жизни больного, связанной с катехоламинемией, стрессовой гиперактивностью симпатической нервной системы [116, 117]. Заслуживает внимания и другой клинический феномен — синдром постуральной гипоксемии (platypnea-orthodeoxia syndrome, POS). Причиной обращения к врачу становится появление позиционной одышки (тахипноэ) при вертика-лизации, вызывающей паническое состояние; в горизонтальном положении самочувствие больного не страдает [118, 119]. Аналогичные симптомы имеют место при любой физической нагрузке, сопровождающейся гипоперфузией мозга [106, 110, 120]. В момент возникновения пароксизма регистрируется ситуационное падение сатурации в диапазоне 8–12%. Основной контингент: больные, перенесшие острый респираторный дистресс-синдром [118].
К базовым признакам аутоиммунной вегетативной ганглионопатии, верхней, нижней стволовой и эндокринной дисфункции , помимо указанных, отнесены нарушения терморегуляции (внезапные суточные колебания температуры в виде гипер-/гипотермии, плохая переносимость холода/жары, пойкилотермия), сна (инсомния); спонтанно возникающие эпизоды диспноэ, повышенной потливости; вегетативные (кардиальные, абдоминальные, дизурические) пароксизмы; кашлево-мозговой синдром — cough/vasovagal syncope (беттолепсия, респираторный припадок); синдром Рейно; синдром раздраженного кишечника; потеря аппетита; анорексия; астенодинамия/истоще-ние; дисменорея; либидо; вторичный (центральный) гипо- и гипертиреоз; болезнь Грейвса (злокачественный экзофтальм); гипокортицизм (надпочечниковая недостаточность); синдром неадекватной секреции антидиуретического гормона (syndrome of inappropriate secretion of antidiuretic hormone, SIADH) [121–123]. Исключительно редко развиваются нейроофтальмические вегетативные синдромы (Горнера, Эди–Холмса) [124, 125].
Нейротрофические и метаболические нарушения обращают на себя внимание не только в остром, но и в постковидном периоде. Их развитие связано с нейротропным, воспалительным потенциалом SARS-CoV-2, реактивацией Herpes zoster , длительной иммобилизацией больного, локальной ишемией тканей, наличием сахарного диабета, сенсорной, вегетативной нейропатии, длительным использованием гипотензивных, седативных препаратов, вазопрессоров, миорелаксантов, кортикостероидов [126, 127]. К клинически значимым проявлениям относятся синдром Мелькерсона– Розенталя [128]; периорбитальный отек; целлюлит; флегмона глазницы; некроз; перфорация твердого неба [129]; эктазия слюнных желез; сухость во рту (ксеростомия) [130], конъюнктивы, роговицы глаз (ксерофтальмия, синдром сухого глаза) [131]; выпадение волос/алопеция [132]; гетеротопическая ос-сификация [133]; снижение минеральной плотности костной ткани; остеопороз; остеосклероз; остеонекроз таранной, пяточной кости, головки плечевой, бедренной кости [134]; «обмороженные» пальцы рук, акроишемия стоп (COVID toes/pseudo-chilblain) [135]; типичные и атипичные пролежни (локализация — лицо, передняя стенка грудной клетки, живот, гребни подвздошной кости, колени) [136, 137]; язвы слизистых оболочек губ, щек, десен, полости рта, твердого неба, языка [138].
КТ ГА
Поражение мышц (миалгии, миопатии, миастенический синдром). Развитие и подострое течение воспалительного процесса, инфицирование мышечных клеток, экспрессирующих рецепторы ангиотензинпревращающего фермента 2 (angiotensin-converting enzyme 2), длительная иммобилизация, вентиляция легких с применением миорелаксантов, назначение хлорохина, гидроксихлорохина, рибавирина, кортикостероидов становятся причиной развития и сохранения у больных локального отека, уплотнения мышц, мышечной слабости, утомляемости, миалгий, диспноэ, похудания (уменьшение объема мышечной массы). Углубленное инструментальное (электромиография, МРТ, ультразвуковое исследование мышц верхних и нижних конечностей, сердца, диафрагмы, диафрагмального нерва в области шеи, межреберных мышц, мышц верхних и нижних конечностей) и лабораторное (определение содержания в крови провоспалительных цитокинов, КФК, миоглобина) обследование, исследование мышечной ткани при биопсии и аутопсии выявляет у пациентов достоверные признаки поражения нервно-мышечного аппарата в виде вялого тетрапареза/ тетраплегии; дисфагии; миастенической утомляемости мышц; саркопении (миопении); воспалительной миопатии; кардиомиопатии; миозита; некроза мышц (рабдомиолиза); атрофии мышц диафрагмы, межреберных мышц, живота, скелетной мускулатуры; дисфункции, гипертрофии, фиброза мышц диафрагмы при искусственной вентиляции легких; повышения в крови уровня общей и МВ-фракции КФК [139, 140]. Обращает внимание гетерогенность клинических форм. Первое место занимают первичная миопатия критических состояний (critical illness myopathy, CIM); другие варианты, возникающие в остром и постковидном периоде, являются раритетными: параспинальный ковидмиозит поясничных мышц, тазового пояса, фациобульбарная конечностная форма; посвакцинальный ковид-миозит; иммуноопосредованные воспалительная миопатия (inflammatory and immune myopathies, IIM), миозит, дерматомиозит; генерализованная, локальная миастения de novo [141, 142]; некоторые из них (рабдомиолиз, дерматомиозит с антителами к MDA5, некротический аутоиммунный миозит / NAM /анти-HMGCR-миопатия — подтип IIM) могут стать причиной летального исхода [143, 144]. Проведение дифференциального диагноза дает возможность исключить идиопатические воспалительные миопатии, статинассоциированную ауто- иммунную миопатию, дерматомиозит, полиомиозит при заболеваниях соединительной ткани; анти-SS-OM-миозит, вторичные нейрогенные формы поражения мышц при позиционной компрессионной невропатии; нейропатии диафрагмального нерва при сахарном диабете, алиментарной недостаточности, воспалительных аутоиммунных, лекарственных формах полинейропатий, сенсомоторной аксональной полиневропатии критических состояний (critical illness polyneuropathy, CIP), полинейропатии-миопатии (CIPM, CINM) [145, 146]. Приобретенная конечностная и туловищная слабость в отделении интенсивной терапии (ICUAW) встречается часто, но выявляется редко [147]. Раннее распознавание, определение нозологии осложнения, знание патогенеза и течения патологического процесса позволяют своевременно назначить и провести персонализированную терапию и реабилитацию, минимизируя развитие негативных функциональных последствий у конкретного больного.
Дисфункция базальных ганглиев, нигростри-атной системы, мозжечка. Нарушение функции базальных ганглиев относится к раритетным формам поражения нервной системы при COVID-19. Оно связано с внутримозговыми кровоизлияниями, нейровоспалением — некротической формой геморрагической лейкоэнцефалопатии, инфарктами мозга, тромбозом глубоких церебральных вен, причиной которых стали артериит/эндотелиит, гиперкоагуляция подкорковых сосудов, многоуровневое повреждение (корково-подкорковые зоны, верхние, средние сегменты ствола, мозжечок), среди причин которого фигурируют также пара-инфекционные аутоиммунные, токсико-гипоксические и лекарственные поражения мозга [148, 149]. Топический диагноз при невозможности проведения нейровизуализации основывается на оценке моторных проявлений. К ним относятся тремор рук, миоклонус мягкого неба, мозжечковая атаксия, кататония, акатизия, акинетико-ригидный синдром, акинетический мутизм, синдром «запертого» человека (locked-in), хореический гиперкинез, генерализованный и локальный миоклонус, опсокло-нус-миоклонус [150–152]. В постковидном периоде сохранение у этих больных нейровоспаления, окислительного дистресса, накопление в структурах мозга альфа-синуклеина, индуцирование локальных аутоиммунных реакций — важные условия для развития и прогрессирования после нейроинвазии нейродегенеративного процесса [153, 154]. Разрушительное действие COVID-19 особенно выражено
<линическая 2021 п эакти keu Том 12 №2
у пациентов с болезнью Паркинсона и Альцгеймера [155, 156]. Показатель смертности выше при болезни Альцгеймера [157].
Лекарственные осложнения. Используемые при лечении больных COVID-19 лекарственные препараты могут обусловить развитие парестезий (лопинавир/ритонавир), головной боли (азитромицин, тоцилизумаб), миалгии, миозита, токсической миопатии, рабдомиолиза (хлорохин, гидроксихлорохин, азитромицин, колхицин, лине-золид, кортикостероиды), нейромиопатии (хлорохин, гидроксихлорохин), нарушение зрения и слуха (хлорохин, гидроксихлорохин), головокружения, атаксии (азитромицин гидроксихлорохин, умифе-новир/арбидол), лекарственно-индуцированных аритмий, гипотензии, обморока, судорог, остановки сердца (хлорохин, гидроксихлорохин, ремдеси-вир, азитромицин), церебральной тромботической микроангиопатии, лейкоэнцефалопатии (тоцилизу-маб) [158–161]. Некоторые препараты становятся причиной эмоциональных расстройств (хлорохин азитромицин лопинавир/ритонавир, тоцилизумаб, кортикостероиды, интерферон α 2b), нарушений сна (азитромицин интерферон α 2b) [158]. Негативное влияние на когнитивные, исполнительные функции оказывают кортикостероиды, тоцилизумаб, интерферон α 2b [160]. Аномальное поведение, бред, возбуждение, галлюцинации провоцируют хлорохин, гидроксихлорохин, кортикостероиды, лопина-вир/ритонавир, кортикостероиды, интерферон α 2b, умифеновир/ арбидол, фавипиравир [158, 160].
Развитие летального исхода, внутримозгового кровоизлияния, ишемического инсульта, тромбоза церебральных синусов и вен с/без тромбоцитопении, паралича Белла, дисфонии, тремора, острого поперечного миелита, острого диссеминированного энцефаломиелита, синдрома Гийена–Барре, фокальных эпилептических приступов de novo зарегистрировано при введении вакцин AstraZeneca, Pfizer, Moderna, Janssen, Covaxin [162–165], но эти осложнения при всей их трагичности возникают не чаще, чем при вакцинальной профилактике других инфекций. Преимущества вакцинации на популяционном уровне перевешивают риски неврологических осложнений. Антиковидные вакцины, вероятнее всего, являются провоцирующим фактором — триггером, а не причиной их развития.
ЗАКЛЮЧЕНИЕ
Таким образом, основная цель SARS-CoV-2 — дыхательные пути, но следующие его мишени — мозг, мышечная и иммунная системы. У пациентов с тяжелым течением инфекции более вероятно развитие таких неврологических осложнений, как острая цереброваскулярная недостаточность, нарушение сознания и повреждение скелетной мускулатуры. Вовлечение в патологический процесс центральной нервной системы является предиктором плохого прогноза. У таких больных может быстро ухудшиться состояние и наступить летальный исход. При клинической оценке состояния больных врачам, независимо от их специальности, необходимо обращать пристальное внимание не только на респираторные проявления болезни, но и на неврологическую симптоматику, наличие и прогрессирование которой возможно как в остром, так и постостром периоде (COVID-19 Long Tail).
ДОПОЛНИТЕЛЬНАЯ ИНФОРМАЦИЯ
Вклад авторов. В.В. Белопасов — идея и концепция обзора, анализ литературы, клинических данных, написание текста; Е.Н. Журавлева, Н.П. Нугманова, А.Т. Абдрашитова — клиническая оценка больных, подготовка иллюстраций. Авторы подтверждают соответствие своего авторства международным критериям ICMJE (все авторы внесли существенный вклад в разработку концепции, проведение исследования и подготовку статьи, прочли и одобрили финальную версию перед публикацией).
Author contribution. Belopasov V.V. — concept of the review, literature analysis, manuscript editing, Zhuravleva E.N., Nugmanova N.P., Abdzashi-tova A.T. — consult of the patient, illustrations. The authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work.
Источник финансирования. Авторы заявляют об отсутствии внешнего финансирования при проведении исследования.
Funding source. This study was not supported by any external sources of funding.
Список литературы Постковидные неврологические синдромы
- Yachou Y, El Idrissi A, Belopasov V, Benali SA. Neuroinvasion, neurotropic and neuroinflam-matory events of SARS-CoV-2: understanding the neurological manifestations in COVID-19 patients. Neurol Sci. 2020;41(10):2657-2669. doi: 10.1007/s10072-020-04575-3
- McGowan EM, Haddadi N, Nassif NT, Lin Y. Targeting the SphK-S1P-SIPR Pathway as a Potential Therapeutic Approach for COVID-19. Int J Mol Sci. 2020;21(19):7189. doi: 10.3390/ijms21197189
- Баклаушев В.П., Кулемзин С.В., Горчаков А.А., и др. COVID-19. Этиология, патогенез, диагностика и лечение // Клиническая практика. 2020. Т. 11, № 1. С. 7-20. [Baklaushev VP, Kulemzin SV, Gorchakov AA, et al. COVID-19. Etiology, pathogenesis, diagnosis and treatment. Journal of Clinical Practice. 2020;11(1):7-20. (In Russ).] doi: 10.17816/clinpract26339
- Белопасов В.В., Яшу Я., Самойлова Е.М., Баклаушев В.П. Поражение нервной системы при COVID-19 // Клиническая практика. 2020. Т. 11, № 2. С. 60-80. [Belopasov VV, Yashu Ya, Samoilova EM, Baklaushev VP. Lesion of the nervous system in COVID-19. Journal of Clinical Practice. 2020;11(2):60-80. (In Russ).] doi: 10.17816/clinpract34851
- Reza-Zaldívar EE, Hernández-Sapiéns MA, Minjarez B, et al. Infection Mechanism of SARS-COV-2 and Its Implication on the Nervous System. Front Immunol. 2021;11:621735. doi: 10.3389/fimmu.2020.621735
- COVID-19 rapid guideline: managing the long-term effects of COVID-19. London: National Institute for Health and Care Excellence (UK); 2020.
- Garrigues E, Janvier P, Kherabi Y, et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020;81(6):e4-e6. doi: 10.1016/j.jinf.2020.08.029
- Yong SJ. Persistent brainstem dysfunction in long-COVID: a hypothesis. ACS Chem Neurosci. 2021;12(4):573-580. doi: 10.1021/acschemneuro.0c00793
- Taboada M, Cariñena A, Moreno E, et al. Post-COVID-19 functional status six-months after hospitalization. J Infect. 2021;82(4):e31-e33. doi: 10.1016/j.jinf.2020.12.022
- Oronsky B, Larson C, Hammond TC, et al. A review of persistent post-COVID syndrome (PPCS). Clin Rev Allergy Immunol. 2021;1-9. doi: 10.1007/s12016-021-08848-3
- Garg P, Arora U, Kumar A, Wig N. The «post-COVID» syndrome: how deep is the damage? J Med Virol. 2021;93(2):673-674. doi: 10.1002/jmv.26465
- Iqba I A, Iqbal K, Arshad AS, et al. The COVID-19 sequelae: a cross-sectional evaluation of post-recovery symptoms and the need for rehabilitation of COVID-19 survivors. Cureus. 2021;13(2):e13080. doi: 10.7759/cureus.13080
- Moreno-Pérez O, Merino E, Leon-Ramirez JM, et al. Post-acute COVID-19 syndrome. Incidence and risk factors: a mediterranean cohort study. J Infect. 2021;82(3):378-383. doi: 10.1016/j.jinf.2021.01.004
- Wijeratne T, Crewther S. COVID-19 and long-term neurological problems: Challenges ahead with Post-COVID-19 Neurological Syndrome. Aust J Gen Pract. 2021 ;(50). doi: 10.31128/AJGP-COVID-43
- Seyed AS, Afsahi AM, Mohsseni PM, et al. Late complications of COVID-19; a systematic review of current evidence. Arch Acad Emerg Med. 2021;9(1):e14. doi: 10.22037/aaem.v9i1.1058
- Nuzzo D, Cambula G, Bacile I, et al. Long-term brain disorders in post COVID-19 neurological syndrome (PCNS) patient. Brain Sci. 2021;11(4):454. doi: 10.3390/brainsci11040454
- García-Azorín D, Trigo J, Talavera B, et al. Frequency and type of red flags in patients with COVID-19 and headache: a series of 104 hospitalized patients. Headache. 2020;60(8):1664-1672. doi: 10.1111/head.13927
- Bobker SM, Robbins MS. COVID19 and headache: a primer for trainees. Headache. J Head Face Pain. 2020;60(8):1806-1811. doi: 10.1111/head.13884
- Silva MT, Lima MA, Torezani G, et al. Isolated intracranial hypertension associated with COVID-19. Cephalalgia. 2020;40(13):1452-1458. doi: 10.1177/ 0333102420965-963
- Toptan T, Aktan C, Basar A, Bolay H. Case series of headache characteristics in COVID-19: headache can be an isolated symptom. Headache. 2020;60(8):1788-1792. doi: 10.1111/head.13940
- Karadaç Ö, Öztürk B, Sonkaya AR, et al. Latent class cluster analysis identified hidden headache phenotypes in COVID-19: impact of pulmonary infiltration and IL-6. Neurol Sci. 2021;1-9. doi: 10.1007/s10072-020-04978-2
- Planchuelo-Gómez Á, Trigo J, de Luis-García R, et al. Deep phenotyping of headache in hospitalized COVID-19 patients via principal component analysis. Front Neurol. 2020;11:583870. doi: 10.3389/fneur.2020.583870
- Al-Hashel JY, Ismail II. Impact of coronavirus disease 2019 (COVID-19) pandemic on patients with migraine: a web-based survey study. J Headache Pain. 2020;21(1):115. doi: 0.1186/s10194-020-01183-6
- Caronna E, Ballvé A, Llauradó A, et al. Headache: A striking prodromal and persistent symptom, predictive of COVID-19 clinical evolution. Cephalalgia. 2020;40(13):1410-1421. doi: 10.1177/0333102420965157
- Poncet-Megemont L, Paris P, Tronchere A, et al. High prevalence of headaches during COVID-19 infection: a retrospective cohort study. Headache. 2020;60(10):2578-2582. doi: 10.1111/head.13923
- Badrah M, Riad A, Kassem I, et al. Craniofacial pain in COVID-19 patients with diabetes mellitus: Clinical and laboratory description of 21 cases. J Med Virol. 2021;93(5):2616-2619. doi: 10.1002/jmv.26866
- Szyszka-Sommerfeld L, Machoy M, Lipski M, Wozniak K. Electromyography as a means of assessing masticatory muscle activity in patients with pain-related temporomandibular disorders. Pain Res Manag. 2020;2020:9750915. doi: 10.1155/2020/9750915
- Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020;277(8):2251-2261. doi: 10.1007/s00405-020-05965-1
- Veronese S, Sbarbati A. Chemosensory systems in COVID-19: evolution of scientific research. ACS Chem Neurosci. 2021;12(5):813-824. doi: 10.1021/acschemneuro.0c00788
- Lee Y, Min P, Lee S, Kim SW. Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J Korean Med Sci. 2020;35(18):e174. doi: 10.3346/jkms.2020.35.e174
- Nguyen NN, Hoang VT, Lagier JC, et al. Long-term persistence of olfactory and gustatory disorders in COVID-19 patients. Clin Microbiol Infect. 2021;S1198-743X(20)30781-3. doi: 10.1016/j.cmi.2020.12.021
- Oliveira RM, Santos DH, Olivetti BC, Takahashi JT. Bilateral trochlear nerve palsy due to cerebral vasculitis related to COVID-19 infection. Arq Neuropsiquiatr. 2020;78(6):385-386. doi: 10.1590/0004-282X20200052
- Doblan A, Kaplama ME, Ak S, et al. Cranial nerve involvement in COVID-19. Am J Otolaryngol. 2021;42(5):102999. doi: 10.1016/j.amjoto.2021.102999
- Corrêa DG, Hygino da Cruz LC, Lopes FR, et al. Magnetic resonance imaging features of COVID-19-related cranial nerve lesions. J Neurovirol. 2021;27(1):171-177. doi: 10.1007/s13365-020-00934-0
- Decavel P, Petit C, Tatu L. Tapia syndrome at the time of the COVID-19 pandemic: Lower cranial neuropathy following prolonged intubation. Neurology. 2020;95(7):312-313. doi: 10.1212/WNL.0000000000010011
- Khacha A, Bouchal S, Ettabyaoui A, et al. Cavernous sinus thrombosis in a COVID-19 patient: A case report. Radiol Case Rep. 2021;16(3):480-482. doi: 10.1016/j.radcr.2020.12.013
- Katyal N, Narula N, Acharya S, Govindarajan R. Neuromuscular complications with SARS-Cov-2 infection: a review. Front Neurol. 2020;11:1052. doi: 10.3389/fneur.2020.01052
- Dos Santos Martins TG. Isolated post SARS-CoV-2 diplopia. J Neurol. 2021;268(2):391. doi: 10.1007/s00415-020-10072-6
- Cava i agli A, Peiti G, Conti C, et al. Cranial nerves impairment in post-acute oropharyngeal dysphagia after COVID-19. Eur J Phys Rehabil Med. 2020;56(6):853-857. doi: 10.23736/S1973-9087.20.06452-7
- Dicp i nigaitis PV, Canning BJ. Is there (will there be) a post-COVID-19 chronic cough? Lung. 2020;198(6):863-865. doi: 10.1007/s00408-020-00406-6
- Visca D, Beghè B, Fabbri LM, et al. Management of chronic refractory cough in adults. Eur J Intern Med. 2020;81:15-21. doi: 10.1016/j.ejim.2020.09.008.
- Halpert G, Shoenfeld Y. SARS-CoV-2, the autoimmune virus. Autoimmun Rev. 2020;19(12):102695. doi: 10.1016/j.autrev.2020.102695
- Abu-Rumeileh S, Abdelhak A, Foschi M, et al. Guillain-Barre syndrome spectrum associated with COVID-19: an up-to-date systematic review of 73 cases. J Neurol. 2021;268(4):1133-1170. doi: 10.1007/s00415-020-10124-x
- Panariello A, Bassetti R, Radice A, et al. Anti-NMDA receptor encephalitis in a psychiatric COVID-19 patient: A case report. Brain Behav Immun. 2020;87:179-181. doi: 10.1016/j.bbi.2020.05.054
- Бойко А.Н., Сиверцева С.А., Спирин Н.Н. Поражение нервной системы при инфекции COVID-19 с акцентом на ведение пациентов с рассеянным склерозом // Неврология, нейропсихиатрия, психосоматика. 2020. Т. 12, № 1. С. 44-47. [Boyko AN, Sivertseva SA, Spirin NN. Lesion of the nervous system in COVID-19 infection with an emphasis on the management of patients with multiple sclerosis. Neurology, neuro-psychiatry, psychosomatics. 2020;12(1):44-47. (In Russ).] doi: 10.14412/2074-2711-2020-1S-44-47
- Memon AB, Al-Hader R, Patel S, et al. Late-onset rapidly progressive MRI- negative-myelitis after COVID-19 illness. Clin Neurol Neurosurg. 2021;202:106513. doi: 10.1016/j.clin-euro.2021.106513
- Sansone P, Giaccari LG, Aurilio C, et al. Postinfectious Guillain-Barré syndrome related to SARS-CoV-2 infection: a systematic review. Life (Basel). 2021;11(2):167. doi: 10.3390/life11020167
- Waheed S, Bayas A, Hindi F, et al. Neurological complications of COVID-19: guillain-barre syndrome following pfizer COVID-19 vaccine. Cureus. 2021;13(2):e13426. doi: 10.7759/cureus.13426
- Lunn MP, Cornblath DR, Jacobs BC, et al. COVID-19 vaccine and Guillain-Barre syndrome: let's not leap to associations. J Brain. 2021;144(2):357-360. doi: 10.1093/brain/awaa444
- Гусев Е.И., Мартынов М.Ю., Бойко А.Н., и др. Новая ко-ронавирусная инфекция (COVID-19) и поражение нервной системы: механизмы неврологических расстройств, клинические проявления, организация неврологической помощи // Журнал неврологии и психиатрии им. С.С. Корсакова. 2020. Т. 120, № 6. С. 7-16. [Gusev EI, Martynov MYu, Boyko AN, et al. New coro-navirus infection (COVID-19) and damage to the nervous system: mechanisms of neurological disorders, clinical manifestations, organization of neurological care. Journal of Neurology and Psychiatry named after S.S. Korsakov. 2020;120(6):7-16. (In Russ).] doi: 10.17116/jnevro20201200617
- Avenali M, Martinelli D, Todisco M, et al. Clinical and elec-trophysiological outcome measures of patients with post-infectious neurological syndromes related to COVID-19 treated with intensive neurorehabilitation. Front Neurol. 2021;12:643713. doi: 10.3389/fneu r.2021.643713
- Курушина О.В., Барулин А.Е. Поражение центральной нервной системы при COVID-19 // Журнал неврологии и психиатрии им. С.С. Корсакова. 2021. Т. 121, № 1. С. 92-97. [Kurushina OV, Barulin AE. Damage to the central nervous system in COVID-19. Journal of Neurology and Psychiatry named after S.S. Korsakov. 2021;121(1):92-97. (In Russ).]
- Tung-Chen Y, Blanco-Alonso S, Antón-Huguet B, et al. Dolor torácico persistente tras resolución de la enfermedad por cor-onavirus 2019 (COVID-19). Semergen. 2020;46(Suppl 1):88-90. doi: 10.1016/j.semerg.2020.06.006
- Yousefzai R, Bhimaraj A. Misdiagnosis in the COVID-19 era: when zebras are everywhere, don't forget the horses. JACC Case Rep. 2020;2(10):1614-1619. doi: 10.1016/j.jaccas.2020.04.018
- Pogg iali E, Vercelli A, Demichele E, et al. Diaphragmatic rupture and gastric perforation in a patient with COVID-19 pneumonia. Eur J Case Rep Intern Med. 2020;7(6):001738. doi: 10.12890/2020 001738
- Newton-Cheh C, Zlotoff DA, Hung J, et al. Case 24-2020: a 44-year-old woman with chest pain, dyspnea, and shock. N Engl J Med. 2020;383(5):475-484. doi: 10.1056/NEJ-Mcpc2004975
- Gahide G, Frandon J, Vendrell JF. COVID-19 patients presenting with afebrile acute abdominal pain. Clin Med (Lond). 2020;20(3):e4-e6. doi: 10.7861/clinmed.2020-0150
- Ивашкин В.Т., Шептулин А.А., Зольникова О.Ю., и др. Новая коронавирусная инфекция (COVID-19) и система органов пищеварения // Российский журнал гастроэнтерологии, гепатологии, колопроктологии. 2020. Т. 30, № 3. С. 7-13. [Ivash-kin VT, Sheptulin AA, Zolnikova OYu, et al. New coronavirus infection (COVID-19) and the digestive system. Russian Journal of Gastroenterology, Hepatology and Coloproctology. 2020;30(3):7-13. (In Russ).] doi: 10.22416/1382-4376-2020-30-3-7
- Коган Е.А., Березовский Ю.С., Проценко Д.Д., Багдасарян Т.Р. Патологическая анатомия инфекции, вызванной SARS-CoV-2 // Судебная медицина. 2020. Т. 6, № 2. С. 8-30. [Kogan EA, Berezovsky YuS, Protsenko DD, Bagdasar-yan TR. Pathological anatomy of infection caused by SARS-CoV-2. Russian Journal of Forensic Medicine. 2020;6(2):8-30. (In Russ).] doi: 10.19048/2411 -8729-2020-6-2-8-30
- Cheung S, Quiwa JC, Pillai A, et al. Superior mesenteric artery thrombosis and acute intestinal ischemia as a consequence of COVID-19 infection. Am J Case Rep. 2020;21:e925753. doi: 10.12659/AJCR.925753
- Widyadharma IP, Sari NN, Pradnyaswari KE, et al. Pain as clinical manifestations of COVID-19 infection and its management in the pandemic era: a literature review. Egypt J Neurol Psychiatr Neurosurg. 2020;56(1):121. doi: 10.1186/s41983-020-00258-0
- Weng LM, Su X, Wang XQ. Pain symptoms in patients with coronavirus disease (COVID-19): a literature review. J Pain Res. 2021;14:147-159. doi: 10.2147/JPR.S269206
- Clauw DJ, Hauser W, Cohen SP, Fitzcharles MA. Considering the potential for an increase in chronic pain after the COVID-19 pandemic. PAIN. 2020;161(8):1694-1697. doi: 10.1097/j.pain.0000000000-001950
- Aksan F, Nelson EA, Swedish KA. A COVID-19 patient with intense burning pain. J Neurovirol. 2020;26(5):800-801. doi: 10.1007/s13365-020-00887-4
- Attal N, Martinez V, Bouhassira D. Potential for increased prevalence of neuropathic pain after the COVID-19 pandemic. Pain Rep. 2021;6(1):e884. doi:10.1097/PR9.000-0000000000884
- Meyer-FrieRem CH, Gierthmïihlen J, Baron R, et al. Pain during and after COVID-19 in Germany and worldwide: a narrative review of current knowledge. Pain Rep. 2021;6(1):e893. doi: 10.1097/ PR9.0000000000000893
- Alonso-Matielo H, da Silva Oliveira VR, de Oliveira VT, Dale CS. Pain in COVID era. Front Physiol. 2021;12:624154. doi: 10.3389/fphys.2021.624154
- Bureau BL, Obeidat A, Dhariwal MS, Jha P. Peripheral neuropathy as a complication of SARS-Cov-2. Cureus. 2020;12(11):e11452. doi: 10.7759/cureus.11452
- Fernandez CE, Franz CK, Ko JH, et al. Imaging review of peripheral nerve injuries in patients with COVID-19. Radiology. 2021;298(3):E117-E130. doi: 10.1148/radiol.202020-3116
- Andalib S, Biller J, Di Napoli M, et al. Peripheral nervous system manifestations associated with COVID-19. Curr Neurol Neu-rosci Rep. 2021;21(3):9. doi: 10.10-07/s11910-021-01102-5
- Sabharwal P, Chakraborty S, Tyagi N, Kumar A. Acute flaccid quadriparesis in a recovering COVID-19 patient: a clinical dilemma. Indian J Crit Care Med. 2021;25(2):238-239. doi: 10.5005/ jp-journals-10071-23728
- Карлов В.А., Бурд С.Г., Лебедева А.В., и др. Эпилепсия и COVID-19. Тактика и лечение. Рекомендации Российской противоэпилептической лиги // Эпилепсия и пароксизмальные состояния. 2020. Т. 12, № 1. С. 84-88. [Karlov VA, Burd SG, Lebe-deva AV, et al. Epilepsy and COVID-19. Tactics and treatment. Recommendations of the Russian Antiepileptic League. Epilepsy and Paroxysmal States. 2020;12(1):84-88. (In Russ).]
- Danoun OA, Zillgitt A, Hill C, et al. Outcomes of seizures, status epilepticus, and EEG findings in critically ill patient with COVID-19. Epilepsy Behav. 2021;118:107923. doi: 10.1016/j.yebeh.2021.107923
- Kincaid KJ, Kung JC, Senetar AJ, et al. Post-COVID seizure: A new feature of "long-COVID". Eur Neur Sci. 2021;23:100340. doi: 10.1016/j.ensci.2021.100340
- Dono F, Nucera B, Lanzone J, et al. Status epilepticus and COVID-19: A systematic review. Epilepsy Behav. 2021;118:107887. doi: 10.1016/j.yebeh.2021.107887
- Belli S, Balbi B, Prince I, et al. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived the hospitalisation. Eur Respir J. 2020;56(4):2002096. doi: 10.1183/13993003.02096-2020
- Mohr A, Dannerbeck L, Lange TJ, et al. Cardiopulmonary exercise pattern in patients with persistent dyspnoea after recovery from COVID-19. Respir Med. 2021;16(1):732. doi: 10.4081/mrm.2021.732
- Townsend L, Dyer AH, Jones K, et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS One. 2020;15(11):e0240784. doi: 10.1371/journal.pone.0240784
- Roy D, Ghosh R, Dubey S, et al. Neurological and neuropsychiatry impacts of COVID-19 pandemic. Can J Neurol Sci. 2021;48(1):9-24. doi: 10.1017/cjn.2020.173
- Tuzun S, Keles A, Okutan D, et al. Assessment of musculoskeletal pain, fatigue and grip strength in hospitalized patients with COVID-19. Eur J Phys Rehabil Med. 2021. doi: 10.23736/S1973-9087.20.06563-6
- Ortelli P, Ferrazzoli D, Sebastianelli L, et al. Neuropsycho-logical and neurophysiological correlates of fatigue in post-acute patients with neurological manifestations of COVID-19: Insights into a challenging symptom. J Neurol Sci. 2021;420:117271. doi: 10.1016/j.jns.2020.117271
- Mohabbat AB, Mohabbat NM, Wight EC. Fibromyalgia and chronic fatigue syndrome in the age of COVID-19. Mayo Clin Proc Innov Qual Outcomes. 2020;4(6):764-766. doi: 10.1016/j.mayocpiqo.2020.08.002
- Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-95. doi: 10.1016/j.ijid.2020.03.017
- Ferraro F, Calafiore D, Dambruoso F, et al. COVID-19 related fatigue: Which role for rehabilitation in post-COVID-19 patients? A case series. J Med Virol. 2021;93(4):1896-1899. doi: 10.1002/jmv.26717
- Mine rs S, Kehoe PG, Love S. Cognitive impact of COVID-19: looking beyond the short term. Alzheimers Res Ther. 2020;12(1):170. doi: 10.1186/s13195-020-00744-w
- Guedj E, Million M, Dudouet P, et al. (18)F-FDG brain PET hypometabolism in post-SARS-CoV-2 infection: substrate for persistent/delayed disorders? Eur J Nucl Med Mol Imaging. 2021 ;48(2):592-595. doi: 10.1007/s00259-020-04973-x
- Whiteside DM, Oleynick V, Holker E, et al. Neurocognitive deficits in severe COVID-19 infection: Case series and proposed model. Clin Neuropsychol. 2021;1-20. doi: 10.1080/13854046.2021.1874056
- Stracciari A, Bottini G, Guarino M,; Cognitive and Behavioral Neurology Study Group of the Italian Neurological Society. Cognitive and behavioral manifestations in SARS-CoV-2 infection: not specific or distinctive features? Neurol Sci. 2021;1-9. doi: 10.1007/s10072-021-05231-0
- Остроумова Т.М., Черноусов П. А., Кузнецов И. В. Когнитивные нарушения у пациентов, перенесших COVID-19 // Неврология, нейропсихиатрия, психосоматика. 2021;13(1):126-130. [Ostroumova TM, Chernousov PA, Kuz-netsov IV. Cognitive disorders in patients who underwent COVID-19. Neurology, neuropsychiatry, psychosomatics. 2021;13(1):126-130. (In Russ).] doi: 10.14412/2074-2711-2021-1-126-130
- Alemanno F, Houdayer E, Parma A, et al. COVID-19 cognitive deficits after respiratory assistance in the subacute phase: A COVID-rehabilitation unit experience. PLoS One. 2021;16(2):e0246590. doi: 10.1371/journal. pone.0246590
- Pajo AT, Espiritu AI, Apor AD, Jamora RD. Neuropathologic findings of patients with COVID-19: a systematic review. Neurol Sci. 2021;1-12. doi: 10.1007/s10072-021-05068-7
- Paterson RW, Brown RL, Benjamin L, et al. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. 2020;143(10):3104-3120. doi: 10.1093/brain/awaa240
- Струментова Е.С., Лобзин В.Ю., Лобзин С.В. Нарушение обоняния, поражение центральной нервной системы и риск развития нейродегенеративных заболеваний при COVID-19 // Opinion Leader. 2020. № 8. С. 28-34. [Strumentova ES, Lobzin VYu, Lobzin SV. Olfactory impairment, central nervous system damage and risk of neurodegenerative diseases in COVID-19. Opinion Leader. 2020;(8):28-34. (In Russ).]
- El B i ni Dhouib I. Does coronaviruses induce neurodegenerative diseases? A systematic review on the neurotropism and neuroinvasion of SARS-CoV-2. Drug Discov Ther. 2021;14(6):262-272. doi: 10.5582/ddt.2020.03106
- Steardo L, Steardo L, Verkhratsky A. Psychiatric face of COVID-19. Transl Psychiatry. 2020;10(1):261. doi: 10.1038/s41398-020-00949-5
- Новикова Л.Б., Акопян А.П., Шарапова К.М., Латыпова Р.Ф. Неврологические и психические расстройства, ассоциированные с COVID 19 // Артериальная гипертензия. 2020. Т. 26, № 3. Р. 317-326. [Novikova LB, Akopyan AP, Shara-pova KM, Latypova RF. Neurological and mental disorders associated with COVID 19. Arterial Hypertension. 2020;26(3):317-326. (In Russ).] doi: 10.18705/1607-419X-2020-26-3-317-326
- Jasti M, Nalleballe K, Dandu V, Onteddu S. A review of pathophysiology and neuropsychiatric manifestations of COVID-19. J Neurol. 2020;1-6. doi: 10.1007/s00415-020-09950-w
- Rogers JP, David AS. A longer look at COVID-19 and neuropsychiatric outcomes. Lancet Psychiatry. 2021;8(5):351-352. doi: 10.1016/S2215-0366(21)00120-6
- Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611-627. doi: 10.1016/S2215-0366(20)30203-0
- Харламенкова Н.Е., Быховец Ю.В., Дан М.В., Никитина Д.А. Переживание неопределенности, тревоги, беспокойства в условиях COVID-19 // Психологический журнал. 2020. [Kharlamenkova NE, Bykhovets YuV, Dan MV, Nikitina DA. Experiencing uncertainty, anxiety, and anxiety in the conditions of COVID-19. Psychological Journal. 2020. (In Russ).] Режим доступа: http://ipras.ru/cntnt/rus/institut_p/covid-19/kommentarii-eksp/har-1.html. Дата обращения: 15.03.2021.
- Дороженок И.Ю. Депрессии в период пандемии COVID-19 (разборы клинических случаев) // Неврология, нейропсихиатрия, психосоматика. 2021;13(1):81-86. [Dorozhe-nok IYu. Depression during the COVID-19 pandemic (analysis of clinical cases). Neurology, neuropsychiatry, psychosomatics. 2021;13(1):81-86. (In Russ).] doi: 10.14412/2074-2711-2021-1-81-86
- içlek A, Balc MK. Phantosmia with COVID-19 related olfactory dysfunction: report of nine case. Indian J Otolaryngol Head Neck Surg. 2021;1-3. doi: 10.1007/s12070-021-02505-z
- Liu DT, Sabha M, Damm M, et al. Parosmia is associated with relevant olfactory recovery after olfactory training. Laryngoscope. 2021;131(3):618-623. doi: 10.1002/lary.29277
- Fontana IC, Bongarzone S, Gee A, et al. PET Imaging as a tool for assessing COVID-19 brain changes. Trends Neurosci. 2020;43(12):935-938. doi: 10.1016/ j.tins.2020.10.010
- Al-Sarraj S, Troakes C, Hanley B, et al. Invited review: the spectrum of neuropathology in COVID-19. Neuropathol Appl Neuro-biol. 2021;47(1):3-16. doi: 10.1111/nan.12667
- Belli S, Balbi B, Prince I, et al. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived the hospitalisation. Eur Respir J. 2020;56(4):2002096. doi: 10.1183/13993003.02096-2020
- Goodman BP, Khoury JA, Blair JE, Grill MF. COVID-19 dysauto-nomia. Front Neurol. 2021;12:624968. doi: 10.3389/fneur.2021.624968
- Johansson M, Stаhlberg M, Runold M, et al. Long-haul post-COVID-19 symptoms presenting as a variant of postural orthostatic tachycardia syndrome: the swedish experience. JACC Case Rep. 2021. doi: 10.1016/j.jaccas.2021.01.009
- Blitshteyn S, Whitelaw S. Postural orthostatic tachycardia syndrome (POTS) and other autonomic disorders after COVID-19 infection: a case series of 20 patients. Immunol Res. 2021;1-6. doi: 10.1007/s12026-021-09185-5
- Motiejunaite J, Balagny P, Arnoult F, et al. Hyperventilation: a possible explanation for long-lasting exercise intolerance in mild COVID-19 survivors? Front Physiol. 2021;11:614590. doi: 10.3389/fphys.2020.614590
- Pasquetto G, Conti GB, Susana A, et al. Syncope, Brugada syndrome, and COVID-19 lung disease. JArrhythm. 2020;36(4):768-770. doi: 10.1002/joa3.12375
- 112.Doodnauth AV, Jallad A, Rizk D, et al. Syncope associated with sinus nodal dysfunction in a COVID-19 patient: a case report and review of the literature. Am J Med Case Rep. 2021;9(4):263-267. doi: 10.12691/ajmcr-9-4-15
- Oates CP, Turagam MK, Musikantow D, et al. Syncope and presyncope in patients with COVID-19. Pacing Clin Electro-physiol. 2020;43(10):1139-1148. doi: 10.1111/pace.14047
- 114.Hernandez PI, Talavera de la EB, Valle PG, Garcia AD. Isolated syncope as a form of presentation of COVID-19 infection. Neurologia. 2021;36(2):185-187. doi: 10.1016/j.nrl.2020.11.001
- Birlutiu V, Birlutiu RM, Feiereisz AI. SARS-CoV-2 infection associated with micturition syncope: Our experience with 4 case reports. Medicine (Baltimore). 2020;99(31):e21512. doi: 10.1097/MD.0000000000021512
- Singh S, Desai R, Gandhi Z, et al. Takotsubo syndrome in patients with COVID-19: a systematic review of published cases. SN Compr Clin Med. 2020;1-7. doi: 10.1007/s42399-020-00557-w
- Finsterer J, Stollberger C. SARS-CoV-2 associated polyrad-iculitis and myocarditis may favour Takotsubo syndrome. Med Hypotheses. 2021;148:110509. doi: 10.1016/j.mehy.2021. 110-509
- Tan GP, Ho S, Fan BE, et al. Reversible platypnea-orth-odeoxia in COVID-19 acute respiratory distress syndrome survivors. Respir Physiol Neurobiol. 2020;282:3510-3515. doi: 10.1016/j.resp.2020.103515
- Singh K, Kadnur H, Ray A, et al. Platypnea-orthodeoxia in a patient with severe COVID-19 pneumonia. Arch Chest Dis. 2020;90(4). doi: 10.4081/monal-di.2020.1609
- Novak P. Post COVID-19 syndrome associated with or-thostatic cerebral hypoperfusion syndrome, small fiber neuropathy and benefit of immunotherapy: a case report. Eur Neur Sci. 2020;21:100276. doi: 10.1016/j.ensci.2020.100276
- Chigr F, Merzouki M, Najimi M. Autonomic brain centers and pathophysiology of COVID-19. ACS Chem Neurosci. 2020;11:1520-1522. doi: 10.1021/acschemneuro.0c00265
- Dani M, Dirksen A, Taraborrelli P, et al. Autonomic dysfunction in 'long COVID': rationale, physiology and management strategies. Clin Med (Lond). 2021;21(1):e63-e67. doi: 10.7861/clinmed.2020-0896
- Трошина Е.А., Мельниченко ГА., Сенюшкина Е.С., Мокрышева Н.Г. Адаптация гипоталамо-гипофизарно-тиреоидной и гипоталамо-гипофизарно-надпочечниковой систем к новому инфекционному заболеванию — COVID-19 в условиях развития COVID-19-пневмонии и/или цитокинового шторма // Клиническая и экспериментальная тиреоидология. 2020. Т. 16, № 1. С. 21-27. [Troshina EA, Melnichenko GA, Seny-ushkina ES, Mokrysheva NG. Adaptation of the hypothalamic-pitu-itary-thyroid and hypothalamic-pituitary-adrenal systems to a new infectious disease-COVID-19 in the development of COVID-19-pneu-monia and/or cytokine storm. Clinical and Experimental Thyroidol-ogy. 2020;16(1):21-27. (In Russ).] doi: 10.14341/ket12461
- De Gennaro R, Gastaldo E, Tamborino C, et al. Selective cranial multineuritis in severe COVID-19 pneumonia: two cases and literature review. Neurol Sci. 2021;42(5):1643-1648. doi: 10.1007/s10072-021-05087-4
- Kaya Tutar N, Kale N, Tugcu B. Adie-holmes syndrome associated with COVID-19 infection: a case report. Indian J Ophthalmol. 2021;69(3):773-774. doi: 10.4103/ijo.IJO_3589_20
- Alzahrani AS, Mukhtar N, Aljomaiah A, et al. The impact of COVID-19 viral infection on the hypothalamic-pituitary-adrenal axis. Endocr Pract. 2021;27(2):83-89. doi: 10.1016/j.eprac.2020.10.014
- Kothandaraman N, Rengaraj A, Xue B, et al. COVID-19 en-docrinopathy with hindsight from SARS. Am J Physiol Endocrinol Metab. 2021;320(1):E139-E150. doi: 10.1152/ajpendo.00480.2020
- Taçlidere B, Mehmetaj L, Ozcan AB, et al. Melkersson-Rosenthal syndrome induced by COVID-19. Am J Emerg Med. 2021;41:262.e5-262.e7. doi: 10.1016/j.ajem.2020.08.018
- Ahmed O, Aladham Y, Mahmood S, Abdelnaby MM. Complicated sinusitis with sphenopalatine artery thrombosis in a COVID-19 patient: a case report. J Surg Case Rep. 2021 ;2021(3):rjab010. doi: 10.1093/jscr/rjab010
- Gherlone EF, Polizzi E, Tetè G, et al. Frequent and persistent salivary gland ectasia and oral disease after COVID-19. J Dent Res. 2021;100(5):464-471. doi: 10.1177/002203452-1997112
- Katz J. Prevalence of dry mouth in COVID-19 patients with and without Sicca syndrome in a large hospital center. Ir J Med Sci. 2021;1-3. doi: 10.1007/s11845-020-02480-4
- Пушкина Н.В. Алопеции и COVID-19. Варианты ведения трихологических пациентов // Косметика и медицина. 2021. № 1. С. 134-140. [Pushkina NV. Alopecia and COVID-19. Options for the management of trichological patients. Cosmetics and Medicine. 2021;(1):134-140. (In Russ).]
- Meyer C, Haustrate MA, Nisolle JF, Deltombe T. Heterotopic ossification in COVID-19: a series of 4 cases. Ann Phys Rehabil Med. 2020;63(6):565-567. doi: 10.1016/j.rehab.2020.09.010
- Barker-Davies RM, O'Sullivan O, Senaratne KP, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54(16):949-959. doi: 10.1136/bjsports-2020-102596
- Putko RM, Bedrin MD, Clark DM, et al. SARS-CoV-2 and limb ischemia: a systematic review. J Clin Orthop Trauma. 2021;12(1):194-199. doi: 10.1016/j.jcot.2020.11.018
- Ramondetta A, Ribero S, Costi S, Dapavo P. Pression-in-duced facial ulcers by prone position for COVID-19 mechanical ventilation. Dermatol Ther. 2020;33(4):e13748. doi:10.1111dth.13-748
- 137.Yu JN, Wu BB, Feng LP, Chen HL. COVID-19 related pressure injuries in patients and personnel: A systematic review. J Tissue Viability. 2021;S0965-206X(21)00040-1. doi: 10.1016/j.jtv.2021.04.002
- Pauli MA, Pereira LM, Monteiro ML, et al. Painful palatal lesion in a patient with COVID-19. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;S2212-4403(21)00160-7. doi: 10.1016/j.oooo.2021.03.010
- Ramani SL, Samet J, Franz CK, et al. Musculoskeletal involvement of COVID-19: review of imaging. Skeletal Radiol. 2021;1-11. doi: 10.1007/s00256-021-03734-7
- Bax F, Lettieri C, Marini A, et al. Clinical and neurophysio-logical characterization of muscular weakness in severe COVID-19. Neurol Sci. 2021;1-6. doi: 10.1007/s10072-021-05110-8
- Mehan WA, Yoon BC, Lang M, et al. Paraspinal myositis in patients with COVID-19 Infection. AJNR Am J Neuroradiol. 2020;41(10): 1949-1952. doi: 10.3174/ajnr.A6711
- 142.Theodorou DJ, Theodorou SJ, Axiotis A, et al. COVID-19 vaccine-related myositis. QJM. 2021;hcab043. doi: 10.1093/qjmed/hcab04
- Barp A, Velardo D, Ciscato P, et al. Anti-HMGCR myopathy misdiagnosed as motor neuron disease and complicated with COVID-19 infection. Neurol Sci. 2021;1-4. doi: 10.1007/s10072-021-05146-w
- Quintana-Ortega C, Remesal A, Ruiz de Valbuena M, et al. Fatal outcome of anti-MDA5 juvenile dermatomyositis in a pae-diatric COVID-19 patient: a case report. Mod Rheumatol Case Rep. 2021;5(1):101-107. doi: 10.1080/24725625.2020.1832755
- Nasuelli NA, Pettinaroli R, Godi L, et al. Critical illness neuromyopathy (CINM) and focal amyotrophy in intensive care unit (ICU) patients with SARS-CoV-2: a case series. Neurol Sci. 2021;42(3):1119-1121. doi: 10.1007/s10072-020-04820-9
- Manzano GS, Woods JK, Amato AA. COVID-19-associ-ated myopathy caused by type I interferonopathy. N Engl J Med. 2020;383(24):2389-2390. doi: 10.1056/NEJMc2031085
- Van Aerde N, van den Berghe G, Wilmer A, et al. Intensive care unit acquired muscle weakness in COVID-19 patients. Intensive Care Med. 2020;46(11):2083-2085. doi: 10.1007/s00134-020-06244-7
- Méndez-Guerrero A, Laespada-García MI, Gómez-Grande A, et al. Acute hypokinetic-rigid syndrome following SARS-CoV-2 infection. J Neurology. 2020;95(15):e2109-e2118. doi: 10.12-12/WN L.0000000000010282
- Roy D, Song J, Awad N, Zamudio P. Treatment of unexplained coma and hypokinetic-rigid syndrome in a patient with COVID-19. BMJ Case Rep. 2021;14(3):e239781. doi: 10.1136/bcr-2020-239781
- Diezma-Martín AM, Morales-Casado MI, García-Al-varado N, et al. Tremor and ataxia in COVID-19. Neurologia. 2020;35(6):409-410. doi: 10.1016/j.nrl.2020.06.005
- Chan JL, Murphy KA, Sarna JR. Myoclonus and cerebel-lar ataxia associated with COVID-19: a case report and systematic review. J Neurol. 2021;1-32. doi: 10.1007/s00415-021-10458-0
- Cohen ME, Eichel R, Steiner-Birmanns B, et al. A case of probable Parkinson's disease after SARS-CoV-2 infection. Lancet Neurol. 2020;19(10):804-805. doi: 10.1016/S1474-4422(20)30305-7
- Brundin P, Nath A, Beckham JD. Is COVID-19 a perfect storm for Parkinson's disease? Trends Neurosci. 2020;43(12):931-933. doi: 10.1016/j.tins.2020.10.009
- Wang H, Qin R, Zhang J, Chen Y. Possible immunity, inflammation, and oxidative stress mechanisms of Alzheimers disease in COVID-19 patients. Clin Neurol Neurosurg. 2021;201:106414. doi: 10.1016/j.clineuro.2020.106414
- Antonini A, Leta V, Teo J, Chaudhuri KR. Outcome of Parkinson>s disease patients affected by COVID-19. Mov Disord. 2020;35(6):905-908. doi: 10.1002/mds.28104
- Воробьев С.В., Шалепо К.В., Спасибова E^., и др. Инфекционные агенты как фактор риска развития болезни Альцгеймера // Журнал инфектологии. 2020. T. 12, № 1. С. 5-13. [Vorobyov SV, Shalepo KV, Spasibova EV, et al. Infectious agents as a risk factor for the development of Alzheimers disease. Journal of Infectology. 2020;12(1):5-13. (In Russ).] doi: 10.22625/2072-6732-2020-12-1-5-13
- 157.Yu Y, Travaglio M, Popovic R, et al. Alzheimer's and Parkinson's diseases predict different COVID-19 outcomes: a uk biobank study. Geriatrics (Basel). 2021;6(1):10. doi: 10.3390/geriat-rics6010010
- Borah P, Deb PK, Chandrasekaran B, et al. Neurological consequences of SARS-CoV-2 infection and concurrence of treatment-induced neuropsychiatric adverse events in COVID-19 patients: navigating the uncharted. Front Mol Biosci. 2021;8:627723. doi: 10.3389/fmolb.2021.627723
- Saniasiaya J, Kulasegarah J. Auditory cinchonism in COVID era. Ear Nose Throat J. 2020;99(9):597-598. doi: 10.1177/0145561320947255
- Al-Ramadan A, Rabab'h O, Shah J, Gharaibeh A. Acute and post-acute neurological complications of COVID-19. Neurol Int. 2021;13(1):102-119. doi: 10.3390/neurolint13010010
- Chang WT, Toh HS, Liao CT, Yu WL. Cardiac involvement of COVID-19: a comprehensive review. Am J Med Sci. 2021;361(1):14-22. doi: 10.1016/j.amjms.2020.10.002
- See I, Su JR, Lale A, et al. US case reports of cerebral venous sinus thrombosis with thrombocytopenia after Ad26. COV2.S; Vaccination, March 2 to, 2021. JAMA. 2021;e217517. doi: 10.1001/jama.2021.7517
- Wolf ME, Luz B, Niehaus L, et al. Thrombocytopenia and intracranial venous sinus thrombosis after "COVID-19 Vaccine AstraZeneca" exposure. J Clin Med. 2021;10(8):1599. doi: 10.3390/jcm10081599
- Román GC, Gracia F, Torres A, et al. Acute transverse myelitis (ATM): clinical review of 43 patients with COVID-19-asso-ciated ATM and 3 post-vaccination ATM serious adverse events with the ChAdOx1 nCoV-19 vaccine (AZD1222). Front Immunol. 2021;12:653786. doi: 10.3389/fimmu.2021.653786
- Waheed S, Bayas A, Hindi F, et al. Neurological complications of COVID-19: Guillain-Barre syndrome following Pfizer COVID-19 vaccine. Cureus. 2021;13(2):e13426. doi: 10.7759/cureus.13426