The use of computed tomography for the study of chronic maxillary sinusitis: based on crania from the Pucar'a de Tilcara fortress, Argentina
Автор: Zubova A.V., Moiseyev V.G., Dmitrenko L.M., Ananyeva N.I., Stulov I.K., Andreev E.V., Kulkov A.M., Obodovskiy A.V., Potrakhov N.N.
Журнал: Archaeology, Ethnology & Anthropology of Eurasia @journal-aeae-en
Рубрика: Anthropology and paleogenetics
Статья в выпуске: 3 т.48, 2020 года.
Бесплатный доступ
Короткий адрес: https://sciup.org/145145502
IDR: 145145502 | DOI: 10.17746/1563-0110.2020.48.3.143-153
Текст обзорной статьи The use of computed tomography for the study of chronic maxillary sinusitis: based on crania from the Pucar'a de Tilcara fortress, Argentina
Chronic maxillary sinusitis (CMS) is a long-lasting inflammation of the mucosa of the maxillary sinuses. Clinical manifestations of this disease include periodic headaches, obstruction of nasal breathing, reduction of the sense of smell, general discomfort and fatigue. In the acute phase of the disease, these can be accompanied by fever and a purulent discharge from the nose (Arefieva et al., 2014: 26; Sipkin et al., 2013: 83–84). The initial infection can have different origin. It can be rhinogenic related to respiratory infections and allergic reactions, hematogenous related to severe infectious diseases, or odontogenic (Mukovozov, 1982: 105). In some cases, chronic sinusitis can result from infection penetration after maxillofacial injuries (Bell et al., 1988). In cases of osteomyelitis or apical periodontitis, the odontogenic infection can penetrate the sinuses directly, if the floor of the sinus in the area of the upper molar and premolar roots is resorbed. But in some cases, the presence of direct communication between the sinus and the alveolus of the infected tooth is not necessary (Buskina, Gerber, 2000; Abrahams, Glassberg, 1996).
The mechanism of development of the disease is similar irrespective of its etiology. The inflammation starting as a result of a sinus infection or an allergic reaction causes swelling of the mucosa, which obstructs outflows of the sinus. This leads to a decrease of partial pressure of oxygen and to a shift of pH inside the sinus towards more acidic values. Aerobic microflora gets partially replaced by anaerobes (mainly by streptococci and bacteria of the genus Prevotella ), and the disease becomes chronic (Arefieva et al., 2014: 20). As the mucosa of the maxillary sinus is bonded with the periosteum, long-lasting inflammations of the sinuses lead to the emergence of foci of boneremodeling and resorption in the walls of the sinus (Sundman, Kjellström, 2013: 447). Such bone-changes can be detected in skeletal remains, which provide an opportunity to study the frequency of this pathology in ancient populations.
Chronic maxillary sinusitis has been the focus of a number of studies employing samples from Northern America, Europe, Africa, and India (Teul et al., 2013; Sundman, Kjellström, 2013; Roberts, 2007; Lewis, Roberts, Manchester, 1995; Panhuysen, Coenen, Bruintjes, 1997; Mushrif-Tripathy, 2014). The results of these studies show that the prevalence of the disease can vary broadly, ranging from 20% to 98.7%. Most of the studies consider living in crowded areas and air pollution as the main cause of a high frequency of CMS (Lewis, Roberts, Manchester, 1995: 503; Roberts, 2007: 804). But other possible factors have not been systematically analyzed.
For correct interpretations of the reasons of CMS in ancient populations, different forms of CMS should be distinguished, since the risk factors for rhinogenic, odontogenic, and hematogenous CMS are different. For the CMS of hematogenous origin, the factor is the presence of a severe disease, leading to infection spreads into sinuses through the circulatory system. Rhinogenic CMS are typically triggered by respiratory infections or air pollution with mechanical particles, which stimulate allergic swelling of the mucosa. The prevalence of odontogenic CMS depends on the state of oral health, which in modern societies is mainly related to social status and hygiene, but in ancient populations to diet (see, e.g., Machicek, Zubova, 2012; Zubova, Marchenko, Grishin, 2016; Lukacs, 1989; Rose, Condon, Goodman, 1985).
Attempts to distinguish between odontogenic and other forms of CMS have been made, to the best of our knowledge, in three studies. The first reports the results for the medieval samples from Maastricht (Panhuysen, Coenen, Bruintjes, 1997). According to this, most cases of CMS in the samples are odontogenic. But this conclusion was based only on an increased prevalence of dental pathologies in the samples, without a direct analysis of the association between dental lesions and maxillary sinus inflammations. In the second study, the prevalence of CMS was compared in samples from medieval England, Northern America, and Africa (Roberts, 2007). The results of that study have shown that while the prevalence of dental pathologies was high in all the samples, CMS was a rare condition in most (Ibid.: 798, tab. 7). According to Roberts, the frequency of CMS was mostly dependent on environmental conditions, occupation, and social status. The importance of dental pathologies for the development of CMS was underlined in the third study, which employed medieval samples from Poland (Teul et al., 2013). The prevalence of odontogenic CMS across the samples was 18.8%, while more than 80% of the cases were explained by such common factors as environment, lifestyle, and climate. The frequency of CMS in all these studies was only approximately estimated, since it was impossible to firmly distinguish inflammations of different etiology with the methods employed.
Diagnosis of CMS in virtually all studies to date has been carried out either via visual macroscopic investigation of affected sinuses (Sundman,
Kjellström, 2013) or using a medical endoscope (Lewis, Roberts, Manchester, 1995; Teul et al., 2013). Both approaches were aimed at detecting the presence of bone remodeling (porosity or bone spicules) on the internal surface of the walls of the sinus (Boocock, Roberts, Manchester, 1995; Sundman, Kjellström, 2013: Fig. 2). Using these methods, it is impossible to determine sources of infections of the sinuses except in the cases where visible fistulas are present in the alveoli (Roberts, 2007: 798, 799). Importantly, both techniques are destructive.
An alternative is the use of computed tomography (CT), which is considered the “gold standard” for diagnosis of CMS in modern medicine (Patel, Ferguson, 2012). This is a non-destructive method perfectly suited for a complex assessment of the paranasal sinuses, dentition, and ostiomeatal complex. Despite its advantages, CT has not been used for the study of CMS in ancient cranial samples before. The main aim of this study was to analyze the diagnostic potential of CT for studying pathologies of the maxillary sinuses in skeletal samples.
Materials
A cranial series dated to the late 8th to 16th centuries AD from the Pucará de Tilcara Fortress in northwestern Argentina was studied. The site is located in the Quebrada de Humahuaca valley, 1800–2800 m a.s.l., near the confluence of the Guasamayo and Río Grande rivers (Otero, 2013: 3). This area is transitory between the Junga and Pune ecological zones. The gorge is situated in the zone of a subtropical climate characterized by warm and arid summers and dry and cool winters. The summer temperature reaches 40–45 °C, while in winter it is only 2–4 °C with occasional frosts. During the late 15th to 16th centuries, the fortress was a large administrative center of the Inca Empire in Argentina, with a population ranging from 538 to 2690 people (Zaburlín, 2009). The founders of the fortress, the Omaguaca Indians, were predominantly agriculturalists cultivating maize, potatoes, quinoa, and common beans, but also practicing some gathering. The only domesticated animal was the llama (Handbook…, 1946: 620).
The cranial series from Pucará de Tilcara (MAE, No. 5148) was moved to the Museum of Anthropology and Ethnography (Kunstkamera) in 1910 via an exchange with the Ethnographic Museum of Buenos Aires (Dmitrenko, 2017;
Dmitrenko, Zubova, 2020: 150). The sample includes the artificially deformed skulls of 20 individuals. Eighteen of these are adults (7 female and 11 male), one sub-adult (14–15 years) and one child (6–8 years). The age at death of the adults was determined on the basis of endocranial suture fusion (Alekseev, Debets, 1964: 29–40), taking into account the possible influence of the artificial cranial deformation on the rate and pattern of suture closure (Gerszten, 1993). Dental wear and the presence of degenerative-dystrophic changes in the temporomandibular joint were taken into account as well (Standards…, 1994: 16–21). Sex was determined on the basis of the dimorphic features of the occipital bone, brow-ridge, supraorbital area, and mastoid process (Alekseev, Debets, 1964: 29–40). The skull of the child was not included in the analysis, since his maxillary sinuses were not completely developed.
Mandibles were absent in 18 out of 19 skulls examined. Several skulls display post-mortem changes: exfoliation of the compact bone layer, widening of the cranial sutures, or tooth loss (in all but three individuals). But in general the skulls are well preserved. Maxillary bones were present in all individuals, and in most cases (84.2%) they did not exhibit any post-mortem damage.
Ante-mortem and peri-mortem traumas were detected in several skulls. These include three cases of healed nasal bone fractures, two cases of a healed fracture of the parietal bones, and two cases of peri-mortem trauma of the parietal and frontal bones. The prevalence of dental pathologies is rather high. Antemortem loss of one or several teeth was detected in 47.3% of the skulls. One individual had had surgery for extracting the lower third molars (Zubova et al., 2020). All the individuals older than 20 years displayed signs of chronic periodontitis, while carious lesions were observed in 69.23% of cases.
Methods
Computed tomography images of all the skulls was made using the medical scanner Philips Brilliance 64. The scanning protocol was as follows: voltage on the X-ray tube 120 kV, tube current 100 μA, without filter, slice thickness 0.9 mm. For a more detailed visualization of the internal surfaces of the sinus, the skulls from Pucará de Tilcara were additionally scanned using microfocus X-ray computed tomography device MRKT-04 constructed at the St. Petersburg Electrotechnical University “LETI”, under the following protocol: X-ray tube voltage 140 kV, amperage 50 μA, no filter, slice thickness 0.1 mm. Post-processing of the images was carried out at the Bekhterev National Medical Research Center of Psychiatry and Neurology, using the Extended Brilliance Workspace workstation; at the “LETI”, using experimental software; and at the Center of X-ray Diffraction Studies of St. Petersburg State University, using CTAn and CTVox (Bruker-microCT). Multiplanar (MPR) and volume (VR) reconstructions were performed.
Several pathological conditions were being detected on the CT images. First, signs of osteitis in the maxillary sinus walls were recorded. The term “osteitis” in the medical literature is used for the inflammation of the bone walls of the sinus leading to irregular thickening and heterogeneous density on the background of focal sclerosis or focal destruction (Biedlingmaier et al., 1996; Erdogan, Fidan, Giritli, 2016; Mafee, Tran, Chapa, 2006; Georgalas et al., 2010; Momeni, Roberts, Chew, 2007; Snidvongs et al., 2014). The porosity and bone spicules, fixed in bioarchaeological studies, are manifestations of osteitis as well. Previous studies employed a visual examination with 3-scored scale for describing these lesions (Sundman, Kjellström, 2013: 450), which implies a qualitative evaluation of the severity of the pathology by a researcher. In contrast to this, using CT data makes it possible to employ quantitative criteria for the same purpose. According to the published protocols (Georgalas et al., 2010), we used the maximum thickness of one of the sinus walls of 3 mm and more as the threshold for diagnosing osteitis. The walls were measured at osteosclerotic foci of both left and right maxillary sinuses, avoiding corners of the sinuses.
Sources of odontogenic infections were detected in the CT images using a number of markers, including the presence of channels connecting the sinus with the alveoli, foci of chronic periodontitis and osteomyelitis, and other dental pathologies. In order to detect the presence of rhinogenic or hematogenous sinusitis, the conditions of bone-tissue of the osteomeatal complex elements were evaluated, and manifestations of inflammation in other paranasal sinuses and the middle ear cavity were traced. In individuals with antemortem trauma of the facial skeleton, the presence of inflammation of the facial bones was additionally assessed, since in such cases traumatogenic infections of the sinuses were possible.
Results
Five cases of CMS were detected in the sample, all in individuals older than 40 years. Four were observed in male skulls, and only one in a female individual. Detail description of the cases follows.
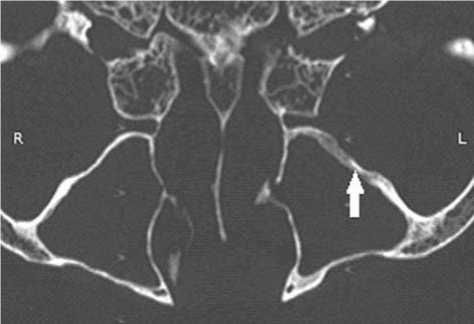
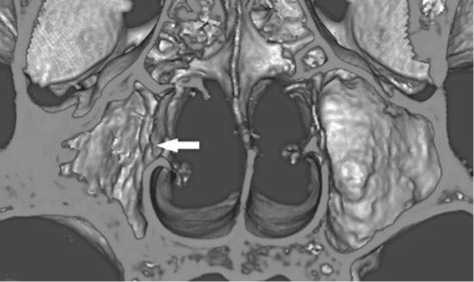
5148-1. Male, 40–50 years . Thickening of the postero-lateral wall of the left maxillary sinus, up to 4 mm in size (Fig. 1, a ) is visible on the CT scan. The floor of the cavity is thinned. The root systems of the left first molar (lost shortly before death) and left second premolar display manifestations of apical periodontitis. The alveoli of these teeth are widened. A thin linear bone defect, connecting the alveolus of the first molar and the sinus, is present. This connection might have been the way through which the cavity was infected (Fig. 1, b ). A widening of the periodontal space and an initial stage of apical periodontitis is observed in the right premolars as well, but no pathological changes were detected in the right sinus. The anterior wall of the left maxilla is concaved inwards and covered with bone spicules. Such spicules, as well as porosis, are also visible in the posterior wall of the cavity. The frontal sinuses of the individual displayed sclerotic changes and thickening of the wall more pronounced in the left sinus.
Chronic periodontal disease caused the antemortem loss of all the upper molars and upper first premolar in this individual. The alveolar process around the second molars is completely resorbed. Traumatic lesions of the facial skeleton were not detected.
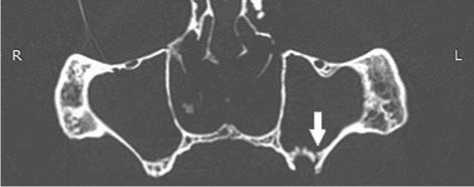
5148-3. Male, 40–50 years. Sclerotic changes and thickening of the walls of the right maxillary sinus, up to 5 mm, are observed in the CT scan (Fig. 2). The alveolus of the second right molar is connected with the sinus by a network of thin channels formed as a result of apical periodontitis and the spreading of infection to bone tissue. The vestibular wall of the alveolus was destroyed by apical inflammation. The second and third right molars were lost less than three months before the death of the individual. The external relief of the posterolateral wall of the right maxilla is abnormal, demonstrating porosis and remodeling of bone tissue.
In this individual, chronic periodontal disease and carious lesions of the first and second left molars were detected. Apical periodontitis was observed in the alveoli of the second molars, and probably a granuloma formed in the alveolus of the lingual root of the left second molar. A peri-mortem comminuted
а
b
Fig. 1. CT images of the skull 5148-1 in axial (a) and coronal (b) projections.
a – the arrow points to thickening of the wall of the left maxillary sinus; b – the arrow points to a channel between an alveola exhibiting periodontal disease and the sinus.
blunt force frontal bone fracture was detected around glabella and the left superciliary arch. The strength of the blow was not very high, as the lesion did not penetrate to the inner layers of the bone. But an examination of the CT scan has shown the presence of a linear defect of the right half of the posterior wall of the frontal sinus related to the frontal bone lesion. As the trauma was caused shortly before death, it did not lead to infection of the frontal sinus. Signs of a completely healed fracture of the right nasal bone were detected. This fracture was not accompanied by an inflammatory process.
5148-18. Female, 45–50 years. Sclerotic changes and thickening of the walls of the right maxillary sinus, up to 6 mm, are observed in the CT scan. The internal surface of the sinus is irregular because of bone remodeling (Fig. 3). Signs of inflammation spread from the alveoli of the premolars are visible at the external surface of the right maxilla. The anterior surface of the maxilla is rough and irregular, deformations and porosis are present in the posterior wall of the bone. The external surface of the left maxilla has no pathological changes. The walls of the
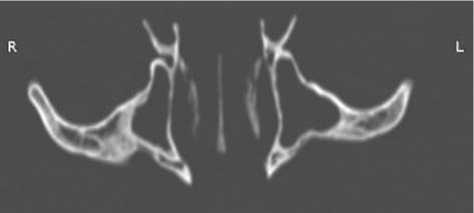
Fig. 2. CT image of the skull 5148-3 in axial projection, showing thickening and deformation of the walls of the right maxillary sinus.
а
b
Fig. 3. CT images of the skull 5148-18 in axial projection (a) and a 3D-reconstruction of its maxillary sinuses ( b , the arrow points to irregularity of the posterior wall of the sinus due to bone remodeling).
right half of the frontal sinus and both halves of the sphenoid sinus are markedly thickened, their contours display irregularity and moderate sclerotic changes.
Most of the teeth, except the I1 and the right canine, were lost ante-mortem. Chronic periodontal disease and almost complete reduction of the alveolar margin of the maxilla were detected in this individual. Cranial trauma is absent.
5148-19. Male, about 40 years. Moderate (up to 3.2 mm) thickening of the antero-lateral walls of both maxillary sinuses is observed in the CT scan.
The second premolars and all molars were lost long before the death of the individual because of chronic periodontal disease. The right incisors were lost antemortem, though much later than the premolars and molars, while the left incisors and both canines were lost post-mortem. A bone exostosis is visible in the area of the lost M2. The external surface of the anterior walls of the maxilla has no pathological changes. The posterior walls of this bone display deformations related to the resorption of bone tissue of the alveolar process around the molars. Cranial trauma is absent.
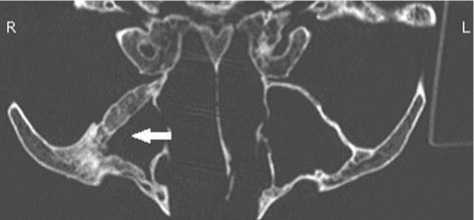
5148-20. Male, 45–50 years. Thickening of the wall of the left maxillary sinus, up to 3.5 mm, and apical periodontitis of the second left premolar are observed in the CT scan. The alveolus of this tooth is connected with the sinus by a linear defect, which does not form a visible fistula (Fig. 4). The premolar was lost shortly before the death of the individual and was accompanied by the formation of apical abscess perforating on the anterior wall of the maxilla. The internal surface of the sinus is irregular because of the remodeled bone.
Manifestations of chronic periodontal disease are observed in this skull. The right canine, first premolar, first and third molars, and the left first to third molars and the second premolar were lost antemortem. The right first incisor was also lost as a result of a trauma. The first left premolar and second right molar display carious cavities. The right nasal bone exhibits a posttraumatic deformation without signs of inflammation.
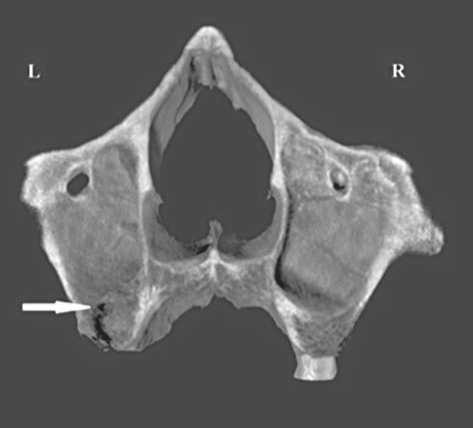
Fig. 4. CT image of the skull 5148-20 in coronal projection (the arrow points to a bone defect connecting the alveolus of the left premolar and the sinus).
Discussion
Our computed tomography study of the cranial collection from Pucará de Tilcara has shown that four of the five cases of CMS in the sample (5148-1, 3, 18, 20) could have been odontogenic. This conclusion is based on the presence of connections between infectious loci in the dentition and the maxillary sinuses. Traumatic sinusitis in these cases can be excluded because no trauma is observed in individuals 1 and 18, while the nasal bone fractures detected in individuals 3 and 20 do not display signs of inflammation. In only one case a trauma of the frontal sinus might have led to infection of the maxillary sinuses (individual 3). But this trauma was peri-mortem and could not have influenced the general pathological state of the individual.
No clear manifestations of rhinogenic inflammation were observed. The preserved fragments of the uncinate processes of the ethmoid bone in the individuals with CMS do not exhibit signs of inflammation. No manifestations of porosity or bone remodeling were detected in the nasal bones or nasal cavity. In all the four cases, inflammation is found in only one sinus, while rhinogenic sinusitis is typically bilateral. The localization of the most pronounced pathological changes of bone tissue at the antero-and postero-lateral walls of the sinuses also points towards a non-rhinogenic etiology of the sinusitis in these individuals, as rhinogenic sinusitis affects the internal wall of the sinus first (Mukovozov, 1982: 110). Nevertheless, the rhinogenic factor cannot be completely excluded in two cases (1 and 18), as in these individuals other paranasal sinuses were affected as well. Infection in these cases might have been secondary. The nature of the pathological condition observed in individual 19 cannot be ascertained from the results of our tomographic and paleopathological observations. All the molar teeth of this individual were lost long before his death. Their alveoli are completely obliterated, and complete reduction of the alveolar process is observed in this part of the dental arch. Thus, the channels connecting the alveoli with the sinuses cannot be traced. Unlike other cases, sinusitis in this individual is bilateral, but it cannot be used as direct evidence of rhinogenic infection without some additional confirmation. Traumatic sinusitis can be firmly excluded in this case because no signs of facial trauma were detected.
The odontogenic origin of all the cases of CMS in the sample was additionally confirmed by the results of a principal component analysis (PCA)
carried out using Statistica for Windows 7.0. The following variables were used (Table 1): main dental pathologies, except caries and enamel hypoplasia (these were excluded since the key teeth were lost ante- or post-mortem in more than a third of the individuals); chronic sinusitis (maximum thickness of the wall of the sinus more than 3 mm); congenital or traumatic deformations of the nasal septum, which, according to recent studies, are risk factors for CMS and frontal sinusitis (see, e.g., Piskunov S.Z., Piskunov G.Z., 2013: 53, 77). Other variables analyzed via PCA were: cribra orbitalia— the marker of anemia leading to weakening of the immune system; chronic otitis; trauma of the nasal area; manifestations of inflammation under the piriform aperture, visible in some skulls (Fig. 5); and the presence of bone remodeling on the external surfaces of the postero-lateral parts of the maxilla.
These pathologies were subjected to the analysis in a binary form (presence/absence).
All the individuals displaying signs of CMS plotted in one cluster in the area of negative values of PC1 (Fig. 6). Judging by the factor loadings, these individuals display a complex of features, including CMS per se , apical periodontitis, antemortem loss of the premolars and molars, and remodeling of bone tissue of the external surface of the maxilla (Table 2). This result is yet one more confirmation of the odontogenic nature of the CMS cases. The individuals not displaying the features mentioned above exhibited positive values of PC1. Deviation of the nasal septum, nasal bone trauma, cribra orbitalia, chronic otitis, and inflammation under the piriform aperture were not related to the presence of CMS. These variables are correlated with second and lower PCs.
Table 1 . Individual distribution of orofacial pathologies and nasal bone trauma
|
£ ” ~ LO "5 О z 0) Ш О c ф ~ -Q 0 E Z 0 |
X CD (Z) |
ro tn ГО c CD p О II st |
CD p О Ф £ C "^ О ГО ГО у |
0 0 0 0 0 |
0 p ro p < |
(D ^ О tn tn 0 E < E |
О tn tn 0 E 0 ro ф E c < Q- |
Q) 0) ГО 0 ^ ^ ■S S E « 2 ” 5 c S X оз го E |
tn ro X ro E p 0 0 |
.5 ro 0 ro 0 |
ro E ro Ф ro tn ro z |
p 0 p c 0 -C 0 |
|
1 |
a |
0 |
0 |
+ |
+ |
+ |
+ |
+ |
+ |
0 |
0 |
0 |
|
2 |
a |
0 |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
+ |
0 |
|
3 |
a |
0 |
0 |
+ |
+ |
+ |
+ |
+ |
+ |
0 |
+ |
0 |
|
4 |
a |
0 |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
|
5 |
a |
0 |
0 |
+ |
+ |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
|
6 |
a |
+ |
0 |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
+ |
0 |
|
7 |
a |
+ |
0 |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
8 |
a |
0 |
0 |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
9 |
a |
+ |
+ |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
10 |
a |
+ |
+ |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
11 |
a |
0 |
+ |
+ |
0 |
+ |
+ |
0 |
0 |
0 |
0 |
0 |
|
12 |
a |
0 |
0 |
+ |
0 |
+ |
+ |
0 |
0 |
0 |
0 |
0 |
|
13 |
a |
0 |
0 |
+ |
+ |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
|
14 |
a |
0 |
0 |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
+ |
|
15 |
a |
+ |
+ |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
17 |
a |
+ |
+ |
0 |
0 |
0 |
0 |
0 |
0 |
+ |
0 |
0 |
|
18 |
a |
+ |
0 |
+ |
+ |
+ |
+ |
+ |
+ |
0 |
0 |
0 |
|
19 |
a |
+ |
0 |
+ |
+ |
+ |
+ |
0 |
+ |
0 |
0 |
0 |
|
20 |
a |
+ |
+ |
+ |
+ |
+ |
+ |
0 |
+ |
0 |
+ |
0 |
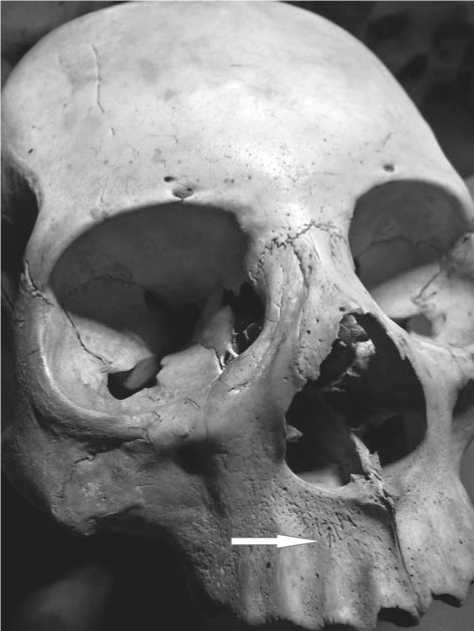
Fig. 5. A skull displaying alteration of the structure of bone tissue below the piriform aperture.
Notably, while a statistical association between apical periodontitis (infectious and inflammatory diseases in the root area) and CMS was detected, the study of the CT images has shown that this association is not strict. As can be seen from Table 1, in two out of seven individuals with apical periodontitis, no pathological change of the maxillary sinuses was detected.
From the methodological point of view, an interesting result of the PCA is the correlation between the signs of CMS observed in CT images and the presence of remodeled bone tissue at the external surface of the maxilla (three cases). The thickness of the walls of the maxillary sinus in all the individuals displaying this feature was more than 3.5 mm. This corresponds to the maximum scores of 4 and 5 on the scale of the severity of osteitis (Georgalas et al., 2010: 456). In the absence of the possibility of applying CT examination or endoscopic observation, the presence of remodeled bone tissue can be used as an external symptom of severe osteitis and, accordingly, CMS. This hypothesis, however, is to be tested using larger samples. But, even if the hypothesis is confirmed, this feature can only be used for individual diagnosis. The use of this at the population level will lead to underestimation of the prevalence of CMS, as the absence of visible signs of bone remodeling does not imply the absence of CMS.
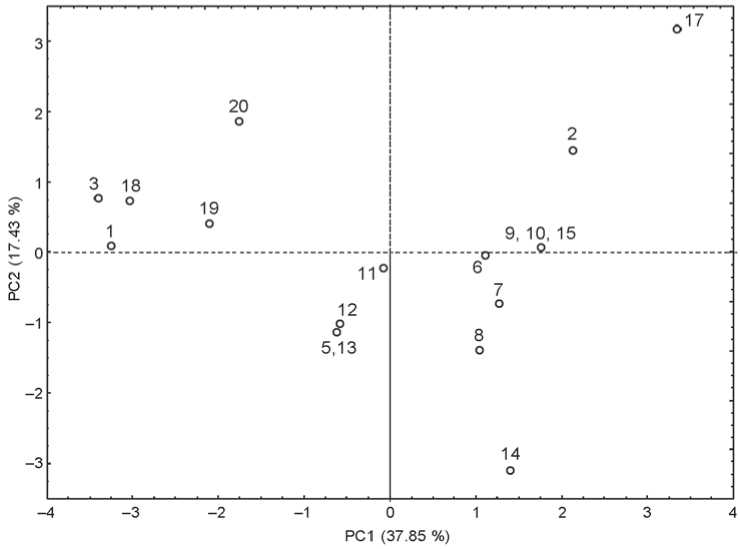
Fig. 6. Scatterplot of the first two principal components of dental and sinus pathological markers (numbers in the plot refer to the numbers of the skulls in the collection MAE No. 5148).
Table 2. Factor loadings on the first two principal components
|
Variable |
PC1 |
PC2 |
|
Deviation of the nasal septum |
0.23 |
0.47 |
|
Infalmmation below the piriform aperture |
0.51 |
0.55 |
|
Chronic periodontitis |
–0.49 |
–0.61 |
|
Apical periodontitis |
–0.85 |
0.14 |
|
Ante-mortem loss of the molars |
–0.87 |
0.03 |
|
Ante-mortem loss of the premolars |
–0.82 |
0.23 |
|
Bone remodeling at the external surfaces of the maxilla |
–0.73 |
0.18 |
|
Chronic maxillary sinusitis |
–0.85 |
0.36 |
|
Cribra orbirtalia |
0.41 |
0.57 |
|
Nasal bone trauma |
–0.13 |
0.40 |
|
Chronic otitis |
0.17 |
–0.56 |
The low frequency of CMS observed in the sample from Pucará de Tilcara might result from several factors. The first is the absence of agents of serious infections (such as measles, scarlet fever, and influenza) in the region, which might trigger CMS as a complication (Fedorova, 2011). Widespread in Europe, these infections were only transmitted to South America during the Age of Exploration, or later (Ramenofsky, 2003). The second factor is the absence of industrial pollution, which clearly affected the health status of some European archaeological samples (Lewis, Roberts, Manchester, 1995). The third is the architecture and location of the fortress. It was situated at the top of a hill, which facilitated natural ventilation of the settlement. The open plan of the residential buildings (Zaburlín, 2010, Tarragó et al., 2010; Otero, 2013) prevented the accumulation of smoke and allergenic particles inside the houses. Finally, the dry subtropical climate with warm summers and moderately cold winters might have prevented spread of the disease. The influence of these factors on the prevalence of CMS in various samples will be the subject of a special study.
Conclusions
Our study has demonstrated a number of advantages of the use of X-ray computed tomography (CT) for the study of chronic maxillary sinusitis (CMS) in archaeological samples. The prevalence of the disease assessed using CT data is similar to that obtained by more traditional techniques like microscopic examination or endoscopy, since all these methods rely on manifestations of osteitis. But CT is non- destructive and permits the use of an objective criterion for diagnosis of CMS: the thickness of the walls of the maxillary sinus displaying manifestations of osteitis. The severity of the disease can be thus determined according to a modern scale (Georgalas et al., 2010). One more advantage of CT is the possibility of objectively diagnosing odontogenic CMS and cases of secondary infection of the sinuses by detecting defects connecting the alveoli of the molars and premolars and the sinus. Such channels are not visible during macroscopic examination. All these capacities of the method applied to archaeological samples make it possible to distinguish more objectively between odontogenic CMS and cases of the transition of rhinogenic infections and allergic reactions in a chronic form.
Acknowledgement
This study was supported by the Russian Foundation for Basic Research, Project No. 18-00-00360 (18-00-00511, 18-00-00350).


