Tibial lengthening over a bioactive degradable intramedullary implant: a case report
Автор: Popkov A.V., Gorbach E.S., Mamedov U.F., Stepanov R.V.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Случай из практики
Статья в выпуске: 6 т.29, 2023 года.
Бесплатный доступ
Introduction Long duration of distraction osteosynthesis remains an unsolved problem. One of the promising ways to stimulate reparative regeneration of bone tissue is the technology of combined osteosynthesis with intramedullary elastic reinforcement with titanium wires coated with hydroxyapatite. A significant drawback of this combined distraction osteosynthesis is the planned removal of intramedullary wires several months after disassembling the Ilizarov apparatus.The purpose of this work is to demonstrate the possibility of stimulating reparative regeneration and reducing the duration of distraction osteosynthesis using an intramedullary degradable implant with bioactive filling.Methods We present the first in clinical practice case of surgical leg lengthening in a female 10-year-old patient using the Ilizarov apparatus an intramedullary degradable implant made of polycaprolactone (PCL) saturated with hydroxyapatite to stimulate reparative regeneration in the tibia. Monthly radiographic monitoring of the process of reparative regeneration of bone tissue was supplemented by computed tomography after disassembling the Ilizarov apparatus.Results The process of lengthening the tibia was accompanied by pronounced formation of a bone “sleeve” around the implant, which was directly connected to the endosteum of the tibia. The density of bone substance in the medullary canal reached 496.6 HU. The cortical layer of the tibia in the elongation zone increased to 4 mm, and its density was equal to 1288.8 HU.Discussion Leg lengthening of 4 cm was achieved along with simultaneous correction of valgus recurvatum bone deformity at IO = 15 days/cm, that is two times shorter than the generally accepted excellent IO in distraction osteosynthesis according to Ilizarov.Conclusions Biodegradable polycaprolactone implants saturated with hydroxyapatite might be not inferior to titanium wires coated with hydroxyapatite in regard to the degree of osteoinduction and do not require repeated surgical intervention to remove them.
Distraction osteosynthesis, ilizarovs apparatus, biodegradable implant, hydroxyapatite
Короткий адрес: https://sciup.org/142240036
IDR: 142240036 | УДК: 616.718.5/.6-089.227.844 | DOI: 10.18019/1028-4427-2023-29-6-645-649
Текст научной статьи Tibial lengthening over a bioactive degradable intramedullary implant: a case report
Distraction osteosynthesis, developed by G.A. Ilizarov, is a unique method of bone tissue bioengineering due to its ability to generate in vivo a vascularized bone tissue that features micro- and macrostructure of the native bone [1]. Moreover, the surrounding soft tissues are simultaneously exposed to regeneration and lengthening under the influence of tension stress [2]. The evolution of the distraction osteosynthesis resulted in the development of numerous technologies for lower and upper limb length discrepancy, bone defects and deformities [3-5]. Many orthopaedic surgeons, giving their due to the advantages of the Ilizarov method, point to significant duration of the external frame
wearing that remains an unresolved problem [6-9]. The index of external fixation (IEF) varies from 0.7 to 5.9 months/cm and depends on the age, etiology, affected bone segment and amount of lengthening. We believe that such a long time of external fixation really increases the likelihood of pin-site infection. The research aimed to stimulate osteogenesis started at the Ilizarov Centre by the end of the XX and the beginning of the XXI century [2, 10, 11]. The technology of combined osteosynthesis with intramedullary elastic reinforcement with titanium nails coated with hydroxyapatite appeared to be one of the simple but very promising ways of stimulating reparative bone tissue regeneration [12]. According to experimental studies conducted at our institution, it does not contradict the principles of the Ilizarov method and does not interfere with intramedullary blood supply [13]. The average IEF of the femur using this technology in children was 20.3 ± 1.36 days/cm [10]. The only but a significant drawback of such combined distraction osteosynthesis is obligatory removal of intramedullary nails a few months after Ilizarov frame removal.
Our case report demonstrates a possibility to lengthen tibia over a biodegradable intramedullary nail that is filled with hydroxyapatite in order to stimulate bone union and avoid nail removal as the previous treatment protocol required [10, 12].
MATERIALS AND METHODS
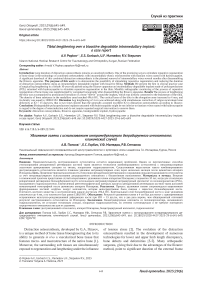
We present a case of 4-cm tibial lengthening in 10-y.o. girl with congenital lower limb length discrepancy due to left tibia. Length discrepancy was complicated by 10° valgus recurvatum deformity with the deformity apex located at the junction of the proximal and middle third of the tibial shaft (Fig. 1, a).
At our institution, the parents of the child were proposed the method of Ilizarov limb lengthening over an intramedullary degradable polycaprolactone (PCL) implant saturated with hydroxyapatite (HA) for treatment (Fig. 1, b).
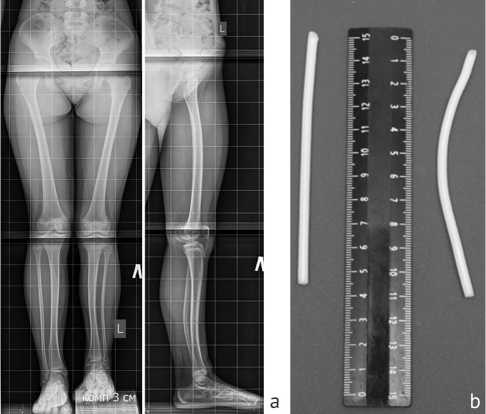
Fig. 1. Preoperative period: a – standing radiographs of lower limb; b – biodegradable implants
The implant materials were ε-polycaprolactone (Sigma-Aldrich, United States; Mn 80000) and hydroxyapatite (Fluidinova, Portugal; 10 ± 5 μm). PCL was dissolved in high purity acetone with a concentration of 15 wt %. Hydroxyapatite was pre-ground in a ball mill in a ceramic chamber with ceramic grinding media with added acetone in a mass ratio of 1.5:1 at a rotation speed of 72 rpm for 12 hours. The PCL solution was added and mixed with HA in the ball mill. The mixture was poured in a thin layer into a preheated fluoroplastic mold. After drying, the composite was crushed in a low-speed polymer crusher (Shini SG-1621N, Taiwan). Filabot EX2 single screw extruder (Filabot, USA) was used to obtain 4-mm wide filaments. Additionally, HA-particles were applied to the implant surface by dipping into a suspension of HA-powder in a solvent of known concentration, and then dried to remove the residual solvent. The implants have the following mechanical properties: ultimate tensile strength 18.3 ± 2.4 MPa (by stretching) and 32.0 ± 3.4 MPa (by pulling) and elastic modulus 425.7 ± 21.9 MPa (by stretching) and 213.9 ± 8.8 MPa (by pulling). For comparison, the titanium alloy nails demonstrate ultimate tensile strength 950 MPa (by stretching) and 1080 MPa (by pulling) and elastic modulus 113.8 MPa (by stretching) and 110 MPa (by pulling) [14]. The implant applied for treatment was 100 mm long and 4 mm wide.
The parents signed an informed consent on the treatment protocol of Ilizarov tibial lengthening and insertion of a PCL/HA intramedullary implant. Institutional ethics board approval for the study was obtained.
Surgery
The first stage of the operation was PCL/HA nail insertion into the medullary canal.
An oblique hole in proximal tibial metaphysis towards the medullary canal was formed using a 5-mm awl through 3 cm soft-tissue approach. Use of awl provided “reaming” for the implant in metaphyseal and proximal and middle diaphysis. The slightly bent implant was inserted manually through this hole, external part of implant cut and then the soft tissues were sutured tightly.
The Ilizarov frame assembly comprised three rings connected with rods and hinges. The positioning of hinges depended on deformity apex and CORA. Partial corticotomy was performed with a conventional chisel and completed with osteoclasis. Upon radiographic control, the frame systems were stabilized. It is important to emphasize that the implant in the medullary canal does not interfere with the insertion of wires but requires strict implementation of the corticotomy technique. There is a risk to cut PCL/HA implant if standard osteotomy would be used.
Post-operative period
Each patient was evaluated every 10-14 days during distraction and deformity correction phase and then monthly during the consolidation phase. Regular radiography (Shimadru Sonialvision 4, Japan) for immediate and every two-weeks bone regeneration control was supplemented by CT (Toshira Aquilion 64, Japan) upon Ilizarov frame removal.
Elongation phase was initiated on the 7th postoperative day at the rate of 1 mm/day divided into 4 times. Planned amount of lengthening was achieved in 42 days (Fig. 2, a).
The fixation phase lasted 23 days. In three weeks of fixation phase the radiology revealed continuity of cortices in the lengthening zone and disappearance of the central fibrous zone of the bone regenerate. It enables frame removal (Fig. 2, b). After frame removal the patient was recommended to walk with progressive weight-bearing on the operated leg. Two months after the external fixator removal, the patient walked with full weight bearing, without additional means of support. The recovery of ROM in adjacent joints was noticed.

Fig. 2. Radiographs of the left tibia: a – by the end of the distraction period; b – radiographs at frame removal
Detailed description of radiographs and computed tomograms. From the first days of distraction the transverse corticotomy of the tibia at the apex of the deformity provided the separation of bone fragments in the absence of direct contact between them. However, the image of regenerated bone tissue got visible since 14th day after the onset of elongation. It could be described as heterogeneous, with separate “islands” of compactions. After one month, the bone regenerate image filled the entire diastasis between the bone fragments. Until the end of the distraction phase the continuity of longitudinally oriented trabeculae maintained. Optical density of the regenerated bone exceeded both optical density of the paraosseous tissues and the density of endosteal callus. Another feature was periosteal and endosteal reaction. Its first signs appeared two weeks after the beginning of lengthening. Throughout the distraction phase, on the image of newly formed bone there was no central zone so called “fibrous, non-mineralized zone of the distraction regenerate”, which is typical in conventional Ilizarov lengthenings. Intramedullary osteogenesis was observed, particularly along the trajectory of the PCL/HA nail.
The radiological signs of bone union were observed in three weeks of fixation phase, it corresponded to continuity of cortices in the lengthening gap and disappearance of the central fibrous zone of the bone regenerate. The frame was removed at this stage. Thus, EFI was 18 days per cm.
Two months after the frame removal, radiographs showed remodeling of callus, increase in the density of newly formed bone (Fig. 3, a, b). There was no deformity neither fractures. Alignment remained normal.
Computed tomography (Fig. 3, c, d, e) performed after the removal of the Ilizarov fixator confirmed a three continuous cortices at lengthening site (their density was 1288.8 ± 141.2 HU), and mineralized central zone of the distraction regenerated bone. The cortical plate along the anterior surface of the leg was presented in the form of separate fragments.
Longitudinally oriented merging trabeculae in the structure of the endosteal part of the regenerated bone formed a bone "sleeve" (Fig. 3, c, d, e) around the implant with the density of 496.6 ± 20.9 HU. No destruction areas neither cysts in the tibia were revealed.

Fig. 3. After frame removal: a – radiographs two months after frame removal; b – amplified image of lengthened tibia, arrows point the trajectory of intramedullary implant and surrounding ossification; c – 3D reconstruction of the left leg by CT scan, protruding end of the implant is visible; d – cross section of the proximal part of newly formed bone; e – cross section of the proximal part of newly formed bone
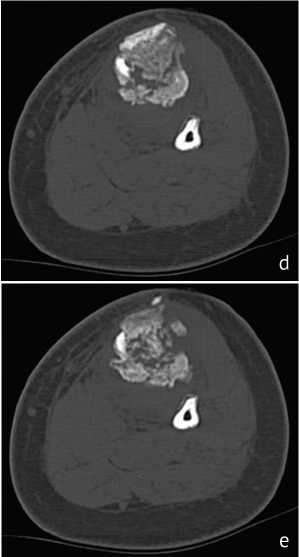
Computed tomography (Fig. 3 c, d, e) performed after the removal of the Ilizarov fixator confirmed a three continuous cortices at lengthening site (their density was 1288.8 ± 141.2 HU), and mineralized central zone of the distraction regenerated bone. The cortical plate along the anterior surface of the leg was presented in the form of separate fragments.
Longitudinally oriented merging trabeculae in the structure of the endosteal part of the regenerated bone formed a bone "sleeve" (Fig. 3 c, d, e) around the implant with the density of 496.6 ± 20.9 HU. No destruction areas neither cysts in the tibia were revealed.
Thus, the consecutive radiographs demonstrated that lengthening with external frame and intramedullary implant made of hydroxyapatite-saturated polycaprolactone provided optimal conditions for bone regeneration. The increased activity of osteogenesis was manifested in the formation of the distraction regenerated bone without evident central fibrous non-mineralized zone, associated with developed periosteal reaction.
DISCUSSION
The use of biodegradable implants providing advantage of non-removal after is a promising approach [15-17]. Due to osteoinductive filling they induce bone formation around it and provide osteointegration stimulating osteogenic activity in the bone marrow canal ensuring stability of bone fragments until union throughout the time of implant resorbtion [18]. The features of implants made of polymers of lactic and glycolic acids for self-locking and auto-compression related to changing in structure under hydrolysis reaction is discussed [19]. There are no studies about possibility to apply intramedullary biodegradable nails for limb lengthening where applied force is traction one and request for bone metabolism is higher than for fracture union. The case presented in the article demonstrates the first experience in this combined technology.
Polycaprolactone (PCL) is a biodegradable thermoplastic used in a variety of medical applications, including bioprinting of hard tissues such as bones and cartilages. It is a polymer that provides improved control of the mechanical properties of ready-made 3D structures. In surgery the 3D implants made of polycaprolactone are used to fill in defects of skull bones and as elastic matrices to fill damaged cartilage tissue [20, 21]. In traumatology, pins and screws made of bioresorbable material are indicated for avulsion [22]. But all available absorbable implants are not bioactive without osteoinductive properties.
The principal difference of the nail that we used in the presented case is hydroxyapatite particles both on the implant surface and as a filling. It is well-known that hydroxyapatite possesses osteoinductive activity [18, 20, 21]. This feature could be favorable for bone lengthening especially in conditions of compromised bone regeneration [23].
This technology demonstrated by this case as excellent bone regeneration. The specific radiological signs were pronounced periosteal reaction both on adjacent bone fragments and at the level of diastasis and bone regenerate without apparent central fibrous zone, so-called “growth zone”. This active bone formation resulted in reduced time of external fixation with index of 18 days per cm.
We have a hypothesis, the result can be explained that bone tissue trabeculae are formed not only under the influence of longitudinal tension forces, but also due to surrounding nail osteoformation related to osteoinductive properties of hydroxyapatite. The elastic PCL/HA intramedullary nail elicits a controlled action and reaction to the host tissue environment with a controlled resorption to be replaced by stimulated regenerating bone tissue.
CONCLUSIONS
This case demonstrates effectiveness of bioactive degradable intramedullary nail in combination with external fixation for tibial lengthening. Intramedullary implant ensures mechanical stability
Conflict of interest Authors declare no conflict of interest.
Funding source This paper has no funding source.
and biological stimulation for bone regenerate and union. Resorbility and biocompatibility of the nail provide advantage to avoid a procedure to avoid implant in follow-up.
Список литературы Tibial lengthening over a bioactive degradable intramedullary implant: a case report
- Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;(238):249-281.
- Morcos MW, Al-fallad H, Hamdy R. Comprehensive Review of Adipose Stem Cells and Their Implication in Distraction Osteogenesis and Bone Regeneration. Biomed Res Int. 2015;2015:842975. doi: 10.1155/2015/842975
- Hosny GA. Limb lengthening history, evolution, complications and current concepts. J Orthop Traumatol. 2020;21(1):3. doi: 10.1186/s10195-019-0541-3
- Fenton C, Henderson D, Samchukov M, et al. Comparative Stiffness Characteristics of Ilizarov- and Hexapod-type External Frame Constructs. Strategies Trauma Limb Reconstr. 2021;16(3):138-143. doi: 10.5005/jp-journals-10080-1539
- Black SR, Kwon MS, Cherkashin AM, et al. Lengthening in Congenital Femoral Deficiency: A Comparison of Circular External Fixation and a Motorized Intramedullary Nail. J Bone Joint Surg Am. 2015;97(17):1432-40. doi: 10.2106/JBJS.N.00932
- Sun XT, Easwar TR, Manesh S, et al. Complications and outcome of tibial lengthening using the Ilizarov method with or without a supplementary intramedullary nail: a case-matched comparative study. J Bone Joint Surg Br. 2011;93(6):782-787. doi: 10.1302/0301-620X.93B6.25521
- Koczewski P, Shadi M. Factors influencing bone regenerate healing in distraction osteogenesis. Ortop Traumatol Rehabil. 2013;15(6):591-599. doi: 10.5604/15093492.1091515
- Pejin Z. Femoral lengthening in children and adolescents. Orthop Traumatol Surg Res. 2017;103(1S):S143-S149. doi: 10.1016/j.otsr.2016.05.020
- Hasler CC, Krieg AH. Current concepts of leg lengthening. J Child Orthop. 2012;6(2):89-104. doi: 10.1007/s11832-012-0391-5
- Popkov D, Lascombes P, fourneau P, Popkov A. Current approaches to flexible intramedullary nailing for bone lengthening in children. J Child Orthop. 2016;10(6):499-509. doi: 10.1007/s11832-016-0781-1
- .Shevtsov VI, Erofeev SA, Gorbach EN, Yemanov AA. Osteogenesis features for leg lengthening using automatic distractors with the rate by 3 mm for 180 times (experimental study). Genij Ortopedii. 2006;(1):10-16. (In Russ.)
- Popkov A, Foster P, Gubin A, et al. The use of flexible intramedullary nails in limb lengthening. Expert Rev Med Devices. 2017;14(9):741-753. doi: 10.1080/17434440.2017.1367284
- Popkov DA, Popkov AV, Kononovich NA, et al. Experimental study of progressive tibial lengthening in dogs using the Ilizarov technique. Comparison with and without associated intramedullary K-wires. Orthop Traumatol Surg Res. 2014;100(7):809-814. doi: 10.1016/j.otsr.2014.06.021
- Standard Specification for Titanium and Titanium Alloy Bars and Billets [Electronic resource]. doi: 10.1520/B0348_B0348M-21. Available at: https://www.astm.org/b0348_b0348m-21.html. Accessed Sept 28, 2023.
- Rokkanen PU, Böstman O, Hirvensalo E, et al. Bioabsorbable fixation in orthopaedic surgery and traumatology. Biomaterials. 2000;21(24):2607-13. doi: 10.1016/s0142-9612(00)00128-129
- Gaiarsa GP, Dos Reis PR, Mattar R Jr, et al. Comparative study between osteosynthesis in conventional and bioabsorbable implants in ankle fractures. Acta Ortop Bras. 2015;23(5):263-267. doi: 10.1590/1413-785220152305121124
- Kuru T, Mutlu I, Bilge A, et al. Biomechanical Comparison of Headless Compression Screws, Kirschner Wires and Bioabsorbable Pins in Distal Oblique Metatarsal Osteotomy for Correction of Hallux Valgus. J Am Podiatr Med Assoc. 2022:1-21. doi: 10.7547/21-204
- Popkov AV, Kulbakin DE, Popkov DA, et al. Solution blow spinning of PLLA/hydroxyapatite composite scaffolds for bone tissue engineering. Biomed Mater. 2021;16(5). doi: 10.1088/1748-605X/ac11ca
- Su Y, Nan G. Treatment of medial humeral epicondyle fractures in children using absorbable self-reinforced polylactide pins. Medicine (Baltimore). 2020;99(17):e19861. doi: 10.1097/MD.0000000000019861
- Bahraminasab M, Doostmohammadi N, Talebi A, et al. 3D printed polylactic acid/gelatin-nano-hydroxyapatite/platelet-rich plasma scaffold for critical-sized skull defect regeneration. Biomed Eng Online. 2022;21(1):86. doi: 10.1186/s12938-022-01056-w
- Ghayor C, Bhattacharya I, Guerrero J, et al. 3D-Printed HA-Based Scaffolds for Bone Regeneration: Microporosity, Osteoconduction and Osteoclastic Resorption. Materials (Basel). 2022;15(4):1433. doi: 10.3390/ma15041433
- Sanders J, Goldstein RY. Open Reduction and Pin Fixation of Pediatric Lateral Humeral Condylar Fractures. JBJS Essent Surg Tech. 2020;10(4):e19.00066. doi: 10.2106/JBJS.ST.19.00066
- Popkov A, Aranovich A, Antonov A, et al. Lower limb lengthening and deformity correction in polyostotic fibrous dysplasia using external fixation and flexible intramedullary nailing. J Orthop. 2020;21:192-198. doi: 10.1016/j.jor.2020.03.014